ORIGINAL REPORT
FEASIBILITY STUDY ON SWALLOWING TELEREHABILITATION IN PATIENTS WITH CORONAVIRUS DISEASE 2019
Shigeto SOYAMA, MS1†, Tomoo MANO, MD, PhD2† and Akira KIDO, MD, PhD2
From the 1Medical Technology Center, Nara Medical University Hospital, Kashihara, Japan and 2Department of Rehabilitation Medicine, Nara Medical University, Kashihara, Japan
Objective: Direct swallowing rehabilitation assessment in patients with highly infectious diseases, such as COVID-19, is not recommended. We aimed to explore the feasibility of using telerehabilitation for managing dysphagia in patients with COVID-19 in isolated hospital rooms.
Design: Open-label trial.
Subjects/patients: We examined 7 enrolled patients with COVID-19 who presented with dysphagia and were treated with telerehabilitation.
Methods: Telerehabilitation was performed for 20 min daily and included indirect and direct swallowing training. Dysphagia was assessed before and after telerehabilitation using the 10-item Eating Assessment Tool, the Mann Assessment of Swallowing Ability and graphical evaluation using tablet device cameras.
Results: All patients showed significant improvement in swallowing ability, evaluated by the range of the upward movement of their larynxes and the Eating Assessment Tool and Mann Assessment of Swallowing Ability scores. The change in swallowing evaluation scores was correlated with the number of telerehabilitation sessions. There was no infection spread to the medical staff treating these patients. Dysphagia in patients with COVID-19 was improved using telerehabilitation while ensuring a high degree of safety for clinicians.
Conclusion: Telerehabilitation might eliminate the risks associated with patient contact and has the advantage of infection control. Its feasibility needs further exploration.
LAY ABSTRACT
We explored the feasibility of using telerehabilitation for managing dysphagia in patients with COVID-19 in isolated hospital rooms. We enrolled 7 patients with dysphagia. Telerehabilitation was performed for 20 min per day and included indirect and direct swallowing training. All patients showed significant improvement in their swallowing ability, evaluated by the range of the upward movement of their larynxes and the Eating Assessment Tool and Mann Assessment of Swallowing Ability scores. The change in swallowing evaluation scores was correlated with the number of telerehabilitation sessions. There was no spread of infection to the medical staff who treated these patients. Dysphagia in patients with COVID-19 was improved using telerehabilitation while ensuring a high degree of safety for clinicians. Telerehabilitation might eliminate the risks associated with patient contact and has the advantage of infection control. Its feasibility should be explored further.
Key words: feasibility study COVID-19; deglutition disorders; dysphagia; telerehabilitation.
Citation: JRM-CC 2023; 6: jrmcc12348. DOI: https://doi.org/10.2340/jrmcc.v6.12348
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: May 9, 2023; Published: June 5, 2023
Correspondence address: Tomoo Mano, Department of Neurology, Nara Medical University, 840 Shijo-cho, Kashihara, Nara 634-8521, Japan. E-mail: manoneuro@naramed-u.ac.jp
†Contributed equally to this paper.
Competing interests and funding: The authors have no conflicts of interest to declare.
This research received no external funding.
Pneumonia due to coronavirus disease 2019 (COVID-19) is characterized by hypoxic respiratory insufficiency. Respiratory support, such as endotracheal intubation and mechanical ventilation, is provided to patients with declining oxygen saturation levels. However, these interventions may increase the risk of dysphagia and, in some cases, lead to post-intubation dysphagia (1). Hence, clinical examination of swallowing, oral care and targeted swallowing training are required before these patients can be discharged (2). Moreover, early intervention is important to prevent malnutrition and pneumonia (3). However, direct prolonged examination of swallowing in patients who are positive for, or are suspected of having, highly infectious diseases is not recommended due to the risk of transmission.
Telerehabilitation involves the interactive assessment of patients by medical professionals without face-to-face interaction. Recent studies have demonstrated the validity and safety of swallowing assessments via telerehabilitation in patients with varying degrees of dysphagia (4). The use of telerehabilitation leads to high levels of patient-reported satisfaction, reinforcing the hypothesis that the delivery of rehabilitative services at a distance is a feasible alternative to routine care (5). Telerehabilitation and care demand improved models of referral and access along with greater flexibility of programmes and professional roles, with management support (6). Multidisciplinary medical teams, should recognise the need for systematic assessment of their recovery and further care in the intensive care unit.
We previously reported a case of a patient with COVID-19 who developed dysphagia characterised by aspiration and caused by drinking (7). The patient underwent telerehabilitation to manage dysphagia to minimise the risk of transmitting infection. Although simple telerehabilitation reportedly manages swallowing difficulties, including contactless assessment and training via videoconferencing, it has major limitations. The cameras used by patients in previous studies produced front-view images that were insufficient to evaluate the upward movement of the thyroid. In this study, we explored the feasibility of telerehabilitation and care for managing dysphagia in patients with COVID-19 in isolation hospital rooms.
METHODS
Patient selection
We enrolled patients with COVID-19 who had dysphagia between May 2021 and August 2021. The inclusion criteria were as follows: (i) COVID-19 diagnosis, (ii) subjective dysphagia and (iii) provision of written informed consent. The exclusion criteria were as follows: (i) a disturbed state of consciousness, (ii) severe cognitive impairment and severe mental disorders, (iii) inability to answer questionnaires and (iv) judged to be inappropriate for inclusion in this study by the investigators (SS and TM). This was an open-label trial to explore the feasibility and safety of dysphagia telerehabilitation and care. This study was conducted in accordance with the Declaration of Helsinki and Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan and was approved by the institutional ethics committee of the Nara Medical University Hospital. Informed consent was obtained from all patients involved in the study.
Intervention
Telerehabilitation is a relatively new method of conducting online clinical assessments (8). The utilization of contactless telerehabilitation by videoconferencing software on a tablet lowers the risk of infection. Multiple additional benefits have been reported, including improved access to rehabilitation medicine, greater time and cost efficiency, greater client focus and enhanced caseload management (9). In addition to the usual oral care conducted by a nurse, we used stickers to mark both sides of the thyroid notch (Fig. 1) to improve the evaluation accuracy. Telerehabilitation was performed for 20 min per day and included indirect and direct swallowing training. Indirect swallowing training included the following: swallowing self-exercises, language training (articulation training), head lift exercises, and coughing and huffing. Direct swallowing training, which was conducted by a speech therapist, included adjustment of the trunk posture angle, neck rotation with the chin down, swallowing awareness training and advice on modifying the bite amount.
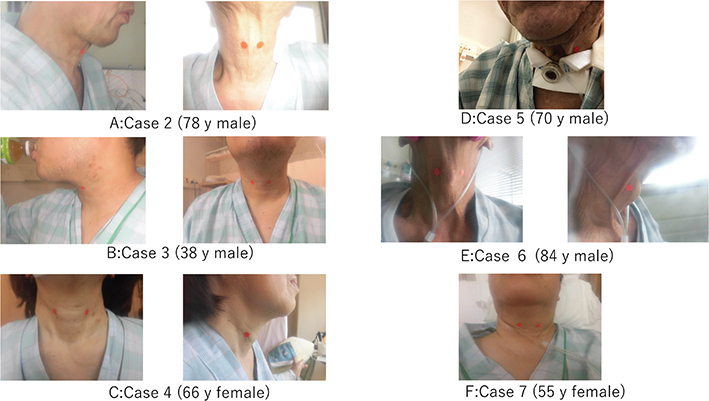
Fig. 1. Stickers marking both sides of the thyroid notch in patients (A–F).
Evaluation
Swallowing was assessed through visual inspection and palpation of the thyroid notch, aided by the placement of stickers on both sides of the notch, a method based on previous reports that used motion tracking systems (10). The physician could easily evaluate the image through the camera, and the front-view image accurately captured the upward movement of the larynx.
We evaluated the range of the upward movement of the larynx as well as swallowing using this method while employing 2 scales: the 10-item Eating Assessment Tool (EAT-10) and the Mann Assessment of Swallowing Ability (MASA) (11, 12). We tested the feasibility of these scales in healthy volunteers before the initiation of this trial, such as how nurses could perform evaluations in the isolation hospital room, adjustment of the camera, etc. The EAT-10 is a self-administered symptom-specific outcome instrument for dysphagia while the MASA is a screening tool that assesses 24 clinical parameters of dysphagia. The MASA evaluation was performed with the assistance of nurses who were wearing personal protective equipment in the patient’s isolated hospital room. The number of compliances was defined as the number of telerehabilitation implementation units and not the number of days.
Statistical analyses
The Shapiro–Wilk test was used to assess whether the data were normally distributed. The Wilcoxon signed-rank test was used to compare longitudinal changes in the parameters between pre- and post-intervention. The null hypothesis stated that there was no change in the parameters between pre- and post-intervention. Results were considered statistically significant at p < 0.05. Correlations between compliance with treatment for swallowing rehabilitation and the functional swallowing scale were assessed using Spearman’s correlation coefficient. Correlation coefficients (r) > 0.40 indicated strong correlations. Statistical analyses were performed using the software package SPSS 23.0 J (SPSS Japan, Tokyo, Japan).
RESULTS
We recruited 12 patients with COVID-19 who presented with dysphagia. Two patients with severe cognitive impairment and severe mental disorders, 1 who was unable to answer questionnaires and 2 who were judged to be inappropriate for inclusion by the investigator (after surgery for cancer, concomitant cerebral infarction) were excluded. Eventually, we enrolled 7 patients. The clinical characteristics of these patients are presented in Table I, and all data are presented as means (SDs). The patients had a mean age of 59.7 ± 25 (range, 38–84) years and a mean disease duration of 9.8 ± 19 days (Table I). The individual data from the study period are presented in Fig. 2. The intervention period lasted 9.9 ± 9.5 (range, 2–28) days. Data comparison before and after the intervention showed that the range of the upward movement of the larynx significantly improved with telerehabilitation (p < 0.05). In line with this finding, the EAT-10 score significantly decreased by 9.6 ± 6.7 (p < 0.05) points (Fig. 2A), while the MASA score significantly increased by 13.1 ± 12.0 points (p < 0.05) (Fig. 2B). These findings suggest that swallowing was improved with telerehabilitation. Furthermore, changes in the EAT-10 and MASA scores from baseline were correlated with patient compliance (Fig. 2). This improved the evaluation and operational processes required for its use in clinical practice. There was no spread of infection to the medical staff who treated these patients.
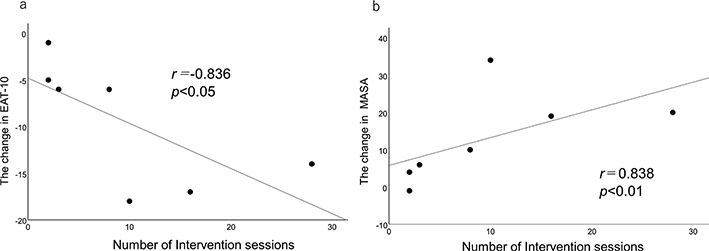
Fig. 2. Correlation between compliance with the intervention and changes in swallowing (A) the 10-item Eating Assessment Tool (EAT-10) score and (B) the Mann Assessment of Swallowing Ability (MASA) score.
Sound and image quality disturbances occurred twice during telerehabilitation. Three patients complained of discomfort with the stickers, and we were unable to ascertain whether the skin to which the stickers were applied moved with the thyroid cartilage in 5 times. Moreover, at the beginning of the 1st week of intervention, 2 patients reported difficulty completing the 20-min session due to fatigue. Thus, we switched to face-to-face rehabilitation on 3 occasions as the instructions could not be communicated adequately during telerehabilitation. Nevertheless, the patients followed all subsequent instructions correctly. No negative effects on motor or swallowing function were recorded.
DISCUSSION
The development of intensive and detail-oriented videoconferencing tools has enabled remote care to be delivered with the same quality as face-to-face rehabilitation assessments (13, 14). Although direct intervention has always been considered the gold standard of rehabilitation, it is necessary to consider alternative types of service delivery as a supplement or replacement of face-to-face treatments under certain circumstances. Recently, telerehabilitation has become an interesting model of care even in speech and language therapy, which has been examined by several studies (15, 16).
Management of dysphagia in patients with COVID-19 and patients with other conditions is fundamental for social reintegration. Contactless rehabilitation via videoconferencing software may minimise the risk of infection by reducing the number of staff in contact and evaluating laryngeal movement through images (17). With the report of its high service satisfaction, tele practice service appears promising in managing dysphagia in an intensive care unit (18). The evaluation items and compliance were associated, but it remains doubtful whether the evaluation index for acute follow-up was appropriate. EAT-10 seems to be effective for early screening in COVID-19 (12). We need to explore more suitable evaluation metrics in the next study.
Nevertheless, contactless assessments and patient training via videoconferencing have limitations; there were some troubles during this study. It is necessary to improve the performance of videoconferencing and review stickers, which are exchanged several times a week in some patients. Also, this study was conducted under some restrictions, and it is unclear whether it is versatile. The members of multidisciplinary team, nurses, therapists and rehabilitation doctor in this study had over a decade of experience, and the patient also had no cognitive impairment. We think that the microaspiration may be overlooked and silent aspiration may not be detected during a video conference. The major limitations of this pilot study were the small sample size, short intervention period and lack of controls. There was some selection sampling bias since patients with some comorbidities and severe respiratory dysfunction could not provide informed consent. Moreover, this study did not compare telerehabilitation to face-to-face rehabilitation. We would need a controlled trial with much greater numbers on a larger scale to clarify the effects of telerehabilitation for dysphagia.
CONCLUSION
This is the first report worldwide discussing the use of telerehabilitation and care for dysphagia in multiple cases of COVID-19. Functional assessment and training tasks related to food intake and swallowing rehabilitation can lead to the generation of droplets and aerosolised particles. Telerehabilitation can reduce the risk of spreading infection by minimizing contact. As telerehabilitation and care have the advantage of infection control, they may be applicable during future pandemics of infectious diseases (19).
ACKNOWLEDGMENTS
We thank the staff of the Department of Rehabilitation Medicine at Nara Medical University.
REFERENCES
- Wujtewicz M, Dylczyk-Sommer A, Aszkiełowicz A, Zdanowski S, Piwowarczyk S, Owczuk R. COVID-19 – what should anaethesiologists and intensivists know about it? Anaesthesiol Intensive Ther 2020; 52: 34–41. https://doi.org/10.5114/ait.2020.93756
- Brugliera L, Spina A, Castellazzi P, Cimino P, Tettamanti A, Houdayer E, et al. Rehabilitation of COVID-19 patients. J Rehabil Med 2020; 52: jrm00046. https://doi.org/10.2340/16501997-2678
- Suh GY, Kang EH, Chung MP, Lee KS, Han J, Kitaichi M, et al. Early intervention can improve clinical outcome of acute interstitial pneumonia. Chest 2006; 129: 753–761. https://doi.org/10.1378/chest.129.3.753
- Burns CL, Ward EC, Hill AJ, Kularatna S, Byrnes J, Kenny LM. Randomized controlled trial of a multisite speech pathology telepractice service providing swallowing and communication intervention to patients with head and neck cancer: evaluation of service outcomes. Head Neck 2017; 39: 932–939. https://doi.org/10.1002/hed.24706
- Laver KE, Schoene D, Crotty M. Telerehabilitation services for stroke. Cochrane Database Syst Rev 2013; 12: CD010255. https://doi.org/10.1002/14651858.CD010255.pub2
- Field PE, Franklin RC, Barker RN, Ring I, Leggat PA. Cardiac rehabilitation service for people in rural and remote areas: an integrative literature review. Rural Remote Health 2018; 18: 4738. https://doi.org/10.22605/rrh4738
- Soyama S, Mano T, Kido A. Oropharyngeal dysphagia telerehabilitation in the intensive care unit for COVID-19: a case report. CoDAS 2022; 34: e20210023. https://doi.org/10.1590/2317-1782/20212021023
- Dimer NA, Canto-Soares ND, Santos-Teixeira LD, de Goulart BNG. The COVID-19 pandemic and the implementation of telehealth in speech-language and hearing therapy for patients at home: an experience report. CoDAS 2020; 32: e20200144. https://doi.org/10.1590/scielopreprints.610
- Ward EC, Burns CL. Dysphagia management via telerehabilitation: a review of the current evidence. J Gastroenterol Hepatol Res 2014; 3: 1088–1094. https://doi.org/10.1007/s00455-001-9390-9
- Hashimoto H, Hirata M, Takahashi K, Kameda S, Katsuta Y, Yoshida F, et al. Non-invasive quantification of human swallowing using a simple motion tracking system. Sci Rep 2018; 8: 5095. https://doi.org/10.1038/s41598-018-23486-0
- Sadeghi Z, Ghoreishi ZS, Flowers H, Mohammadkhani P, Ashtari F, Noroozi M. Depression, anxiety, and stress relative to swallowing impairment in persons with multiple sclerosis. Dysphagia 2021; 36: 902–909. https://doi.org/10.1007/s00455-020-10207-x
- Marchese MR, Ausili Cefaro C, Mari G, Proietti I, Carfì A, Tosato M, et al. Oropharyngeal dysphagia after hospitalization for COVID-19 disease: our screening results. Dysphagia 2022; 37: 447–453. https://doi.org/10.1007/s00455-021-10325-0
- Winters JM. Telerehabilitation research: emerging opportunities. Annu Rev Biomed Eng 2002; 4: 287–320. https://doi.org/10.1146/annurev.bioeng.4.112801.112923
- Kushalnagar P, Paludneviciene R, Kushalnagar R. Video remote interpreting technology in health care: cross-sectional study of deaf patients’ experiences. JMIR Rehabil Assist Technol 2019; 6: e13233. https://doi.org/10.2196/13233
- Nordio S, Innocenti T, Agostini M, Meneghello F, Battel I. The efficacy of telerehabilitation in dysphagic patients: a systematic review. Acta Otorhinolaryngol Italy 2018; 38: 79–85. https://doi.org/10.14639/0392-100X-1816
- Molini-Avejonas DR, Rondon-Melo S, Amato CA. A systematic review of the use of telehealth in speech, language and hearing sciences. J Telemed Telecare 2015; 21: 367–376. https://doi.org/10.1177/1357633X15583215
- Rodriguez-Blanco C, Gonzalez-Gerez JJ, Bernal-Utrera C, Anarte-Lazo E, Perez-Ale M, Saavedra-Hernandez M. Short-term effects of a conditioning telerehabilitation program in confined patients affected by COVID-19 in the acute phase. A pilot randomized controlled trial. Medicina (Kaunas) 2021; 57: 684. https://doi.org/10.3390/medicina57070684
- Burns CL, Ward EC, Gray A, Baker L, Cowie B, Winter N, et al. Implementation of speech pathology telepractice services for clinical swallowing assessment: an evaluation of service outcomes, costs and consumer satisfaction. J Telemed Telecare 2019; 25: 545–551. https://doi.org/10.1177/1357633x19873248
- Malandraki GA, Arkenberg RH, Mitchell SS, Malandraki JB. Telehealth for dysphagia across the life span: using contemporary evidence and expertise to guide clinical practice during and after COVID-19. Am J Speech Lang Pathol 2021; 30: 532–550. https://doi.org/10.1044/2020_AJSLP-20-00252