ORIGINAL REPORT
OFF-LOADING PRESSURE RELIEF WITH FOAM CUT OUT CUSHIONS: EXPERIENCES FROM RANCHO LOS AMIGOS NATIONAL REHABILITATION CENTER
Jan FURUMASU, PT1, Robyn BUCKNER DPT1, Christine MATA, DPT1 and Philip REQUEJO, PhD2
From the 1Department of Physical Therapy, Rancho Los Amigos National Rehabilitation Center, and 2Rancho Research Institute, Downey, CA, USA
This paper explores the efficacy of the cushion fitting technique using foam cut out cushions for off-loading bony prominences in the sitting position, with a particular focus on reducing the high risk of developing pressure injuries among aging wheelchair users. This technique, historically employed at Rancho Los Amigos National Rehabilitation Center, has shown promising results in reducing pressure injuries for patients with spinal cord injuries. However, its widespread adoption remains limited. This manuscript aims to raise awareness about foam cut out cushions, its historical context, and its contemporary relevance by presenting customized solutions for individual patients with specific deformities. Key clinical points are highlighted, emphasizing the importance of skilled clinicians in the fitting process and the need to consider foam cut out cushions alongside other preventive measures. Case examples illustrate successful outcomes, demonstrating improved pelvic stability, posture, and off-loading of bony prominences. By promoting foam cut out cushions as a valuable cushioning option, this manuscript equips clinicians with knowledge to utilize this technique effectively.
LAY ABSTRACT
This paper investigates the effectiveness of using foam cut out cushions to relieve pressure on bony areas while sitting, especially for elderly wheelchair users who are prone to developing pressure injuries. This study delves into the historical background of foam cut out cushions and emphasizes their relevance in addressing the needs of modern patients. By customizing the cushions according to individual requirements, this research highlights a successful alternative for providing personalized cushion solutions to wheelchair users. The findings underscore the importance of adopting the cushion fitting technique to reduce pressure-related health risks, making it a valuable approach for enhancing the comfort and well-being of aging wheelchair users.
Key words: wheelchair cushion; seating; off-loading; pressure relief; mobility; aging.
Citation: JRM-CC 2023; 6: jrmcc18706. DOI: https://doi.org/10.2340/jrmcc.v6.18706
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Sep 29, 2023; Published: Nov 14, 2023
Correspondence address: Philip S. Requejo, Rancho Research Institute, Rancho Los Amigos National Rehabilitation Center, 7601 E. Imperial Highway, Downey, CA 90242, USA. E-mail: prequejo@ranchoresearch.org
Competing interests and funding: The authors have no conflicts of interest to declare.
The growing aging population, including those with disabilities, has raised the risk of pressure ulcers. Advanced age increases not only the frequency but also the severity of these ulcers (1, 2). According to the Agency for Healthcare Research and Quality (AHRQ), in the United States, approximately 2.5 million people develop pressure ulcers yearly (3). According to a clinical practice guideline for healthcare professionals published by the Consortium for Spinal Cord Medicine, pressure ulcers are an underestimated healthcare problem, particularly for individuals with spinal cord injury (4). The annual incidence of pressure ulcers among individuals with spinal cord injuries (SCI) is between 23 and 30%, but up to 85% of SCI individuals develop a pressure ulcer at some point during their lifetimes (1). The risk of developing pressure ulcers increases with injury duration, from 15% at 1 year to 30% at 20 years of follow-up (5). Hence, seat cushions with pressure-relief properties are crucial for preventing pressure ulcer development in aging individuals with SCI.
The foam cut out cushion (FCC) fitting technique is a specialized approach aimed at reducing pressure and minimizing the risk of pressure injuries, particularly targeting vulnerable areas like the ischial tuberosities and coccyx during prolonged sitting. This method has demonstrated a consistent track record of success, particularly at the Rancho Los Amigos National Rehabilitation Center (Rancho), where individuals with SCI continue to experience its benefits even after completing their treatment at the center (6).
For individuals who rely on wheelchairs over the long term, the development of postural deformities such as kyphosis, scoliosis, pelvic obliquity, and posterior pelvic tilt is a common concern (7–9). These deformities can significantly compromise functional abilities while sitting in a wheelchair, resulting in increased discomfort, susceptibility to pressure injuries, compromised balance, and limited use of the upper extremities. FCCs have proven to be highly effective in preventing pressure injuries, particularly for users with tissue atrophy in the pelvic region, as they completely alleviate pressure from high-risk areas. Despite the demonstrated effectiveness of this technique, widespread adoption among clinicians who have not been specifically trained at Rancho remains limited.
This paper aims to provide a historical and current context for FCC, paying tribute to its developers and demonstrating its contemporary applicability by illustrating the customizability of the FCC tailored for patient case example.
KEY CLINICAL POINTS OF FCC RECOMMENDATION
This paper highlights key clinical considerations for recommending FCCs, including:
- Effective off-loading of high-risk bony areas like the ischial tuberosities and coccyx.
- Customizability for accommodating various bony prominences and patient-specific asymmetries.
- The positive impact on quality of life, sitting tolerance, and pressure sore prevention.
- The importance of skilled clinicians in understanding patient anatomy and cushion interaction, facilitating patient training for self-replicable results.
- The recognition that cushion choice alone is insufficient for pressure injury prevention necessitates additional preventive measures.
CONCEPT OF OFF-LOADING VS. IMMERSION IN PRESSURE RELIEVING CUSHIONS
There are 2 main concepts of pressure relief in cushions: off-loading and immersion. The concept of immersion aims to minimize pressure beneath bony prominences by distributing the pressure more evenly over larger surfaces (Fig. 1). On the other hand, the concept of off-loading involves completely unweighting high-risk areas, such as bony prominences, by recessing the surface beneath the sitting area. This redistribution of pressure directs it toward larger and less bony structures, such as the posterior thighs and trochanters. The table presents the safe sitting pressure values proposed by Reswick in his influential 1976 paper (see Table I) (6). These thresholds are provided for different body regions to help assess the risk of pressure-related injuries, particularly in individuals who are immobile or have limited mobility. The values are given in millimeters of mercury (mmHg) and serve as guidelines for determining appropriate support surfaces or interventions to prevent the development of pressure ulcers or bedsores. The FCC technique developed by Rodgers and Reswick (6) utilizes the concept of off-loading (6) to achieve safe sitting pressures.
| Ischial tuberosities | 30–40 mm Hg |
| Greater Trochanter | 60 mm Hg |
| Posterior Thighs | 100 mm Hg |
| Sacrum/Coccyx | 10 mm Hg |
| Tips of Coccyx | 0 mm Hg |
| Mm Hg: Millimeters of Mercury. | |
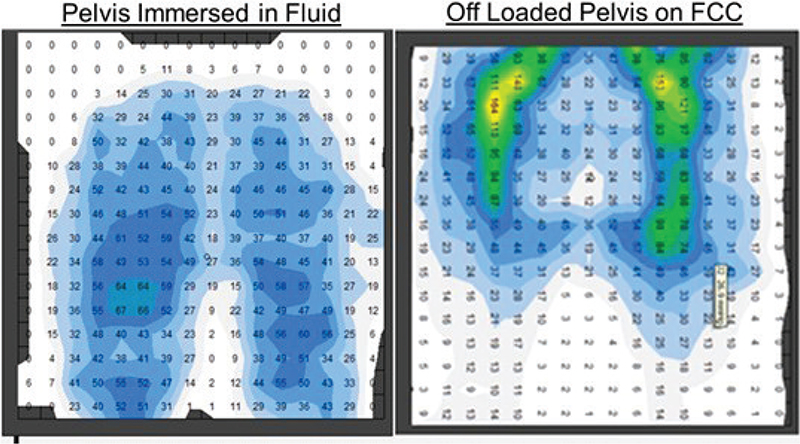
Fig. 1. Pressure mapping illustrates reduced direct pressure on at-risk bony prominences (ischial tuberosity and coccyx) with an off-loading foam cut out cushion (FCC) compared to an immersion fluid cushion by redistributing pressure to the cutout’s soft tissue edges (gluteus maximus and hamstrings).
HISTORICAL PERSPECTIVE IN THE CONCEPT OF FOAM CUT OUT CUSHIONS
The concept of FCC, designed to alleviate pressure, traces its roots back to John Rogers, a pioneering rehabilitation engineer at the Tissue Trauma Group in Rancho. He established the first pressure clinic in the early 1970s (6, 10, 11), and the development of the FCC cutting and fitting technique by John Rogers and Dr. Shannon Stauffer preceded the establishment of this clinic. During this period, pressure injuries were prevalent, affecting 68% of individuals with SCI and 35% of geriatric nursing home residents (12).
To ensure safe pressure levels in custom-designed FCCs, John Rogers devised a simple single transducer sensor and fitting technique. Like modern pressure mapping systems, this sensor allowed therapists to gauge pressure beneath bony prominences. By placing the sensor beneath the prominence and palpating it, therapists could determine the appropriate pressure level. This method allowed for effective customization of pressure-relieving cushions (FCCs) to target high-risk areas, particularly the ischial tuberosities. As a result, it was possible to maintain safe pressure levels, with a maximum sub-ischial pressure of approximately 30 mmHg and a safe pressure of 60 mmHg (10). The concept of FCCs, along with patient education, fitting techniques, and pressure measurement, was shared globally, reaching countries like Scotland and South Africa through collaboration and information exchange (10, 11, 13). Publications from various clinics echoed the approach developed at Rancho, with some variations in the fitting technique (10, 13).
However, in the early 1980s, off-the-shelf cushions using the immersion principle (air, gel or fluid mediums) for pelvis support became more accessible. Consequently, the use of FCCs declined among therapists outside of Rancho. Yet, our continued experience demonstrates that off-loading bony prominences with FCCs has been successful in preventing skin degradation, both in new injury cases and the aging population. Furthermore, the customization options offered by FCCs address other prominences (such as the pubic ramus, trochanter, and posterior femur) and asymmetries (such as the development of heterotrophic ossifications, scoliosis, and pelvic obliquities) that affect positioning and seating.
CURRENT RESEARCH COMPARING OFF-LOADING AND IMMERSION CUSHIONS
Recent research on off-loading cushions, like the RIDE™ orthotic-style cushion, confirms FCCs’ benefits and applicability through pressure mapping and magnetic resonance imaging (MRI) techniques (14, 15). Crane et al.’s study compared off-loading and immersion cushions using pressure mapping (14).
While pressure mapping aids clinicians in cushion selection, it does not predict tissue deformation, increasing the risk of pressure injuries (16). In contrast, MRI studies by Call et al. (15) and Sonenblum et al. (17) measured tissue deformation in high-risk areas, alongside pressure mapping peak pressures and PPI, supporting Crane’s findings.
These MRI studies, coupled with scientific models, enhance clinicians’ understanding of tissue deformation when assessing different cushions (14, 15, 17–21). Despite not being available during Rogers and colleagues’ cushion fitting technique development in the 1960s, these principles of off-loading cushions remain valid.
STANDARD CUT OUT CUSHION
Reswick and Rogers (6) introduced a 4” high cushion composed of Polyurethane, featuring a density of 0.07 g/cm³ (#5 lb. foam) with 3” high lamination beneath 1” of softer, lower-density material at 0.03 g/cm³ (#4 lb. foam). They established a guideline to maintain tissue loading under bony prominences below 30 mm Hg (22). A wooden template (Fig. 2) aids in precisely marking the cut out location, considering cushion width and pelvic anatomy. Cadaver studies showed that the male pelvis is about an inch narrower than the female pelvis. Therefore, cut out dimensions for females are 8 inches wide by 6 inches deep with a 3-inch depth (Fig. 3), while for males, it should be 7 inches wide by 5 inches deep with a 3-inch depth.
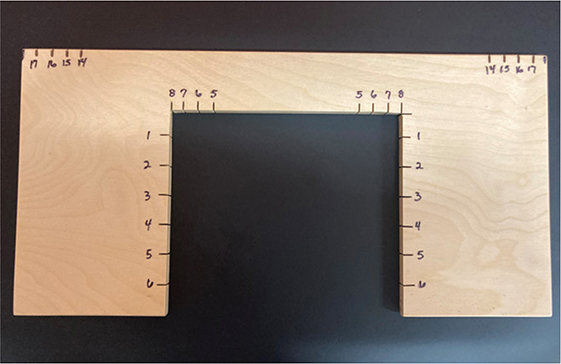
Fig. 2. Customization of cut out area using a wooden template.
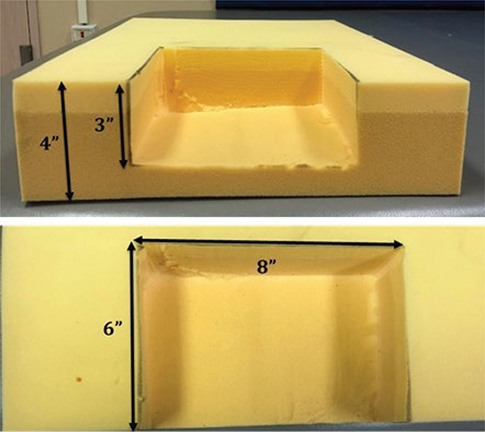
Fig. 3. Standard cut out cushion design specifications.
This standard cut out foam cushion is suitable for most clients without pelvic, hip or spine postural deformities or asymmetries (Fig. 4, Video 1). Polyurethane foam typically lasts 6 months to a maximum of 1 year with normal patient use. A comparison of sitting pressure (Fig. 5) illustrates the difference between a cushion without a cut out and a modified cushion with a cutout (Video 2). The top left image shows a cushion without a cutout, exerting excessive pressure on both ischial tuberosities, as seen in the pressure mapping below it. In contrast, the bottom right image displays a modified cushion with complete cutouts under the trochanters and posterior femur, effectively alleviating pressure from the ischial tuberosities.
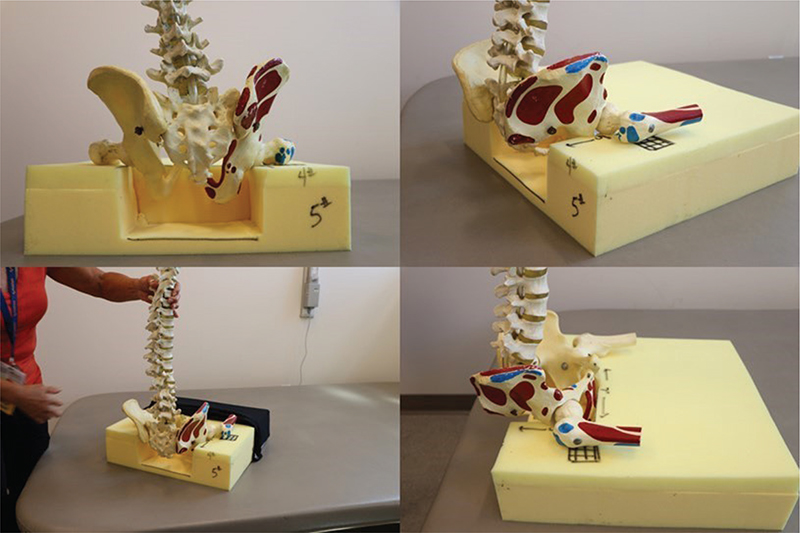
Fig. 4. Illustration of a standard cut out foam cushion, displaying the positioning of the pelvis within the cutout, effectively suspending the ischial tuberosities and coccyx.
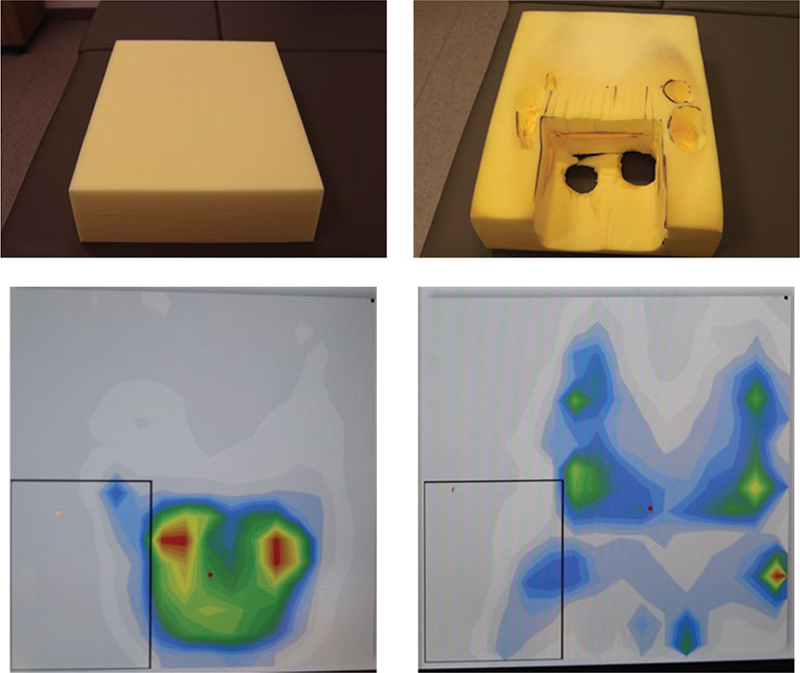
Fig. 5. Sitting pressure comparison, showing the difference between a cushion with (left) and without (right) a cutout.
CUSTOM CUT OUT CUSHIONS TO ADDRESS DEFORMITIES
The evaluation of postural deformities of the pelvis, hips and spine can be done on a mat or supine in a power recliner. In assessing scoliosis or asymmetries of the pelvis, hips, and spine, it is important to discern whether the deformity is fixed or flexible. A flexible deformity can be corrected, whereas a fixed deformity is best accommodated, or pain or increased pressure can result (Video 3).
Posterior pelvic tilt
To accommodate for a posterior pelvic tilt, the cutout can be moved forward 1” with a bridge or V cut to relieve the coccyx (Fig. 6). Palpation of the ischial tuberosities initially will confirm where placement of the cutout should be. If the patient sits with a level pelvis and upright trunk, the standard cutout (8” wide × 6” deep or 7” wide × 5” deep) can be cutout first. If there is excessive redundant tissue on the buttocks, this positions the pelvis forward, and the cutout for the ischial tuberosities needs to be moved forward. For example, if someone is morbidly obese, the pelvis is still approximately the same dimensions width wise, so the cutout is not wider, but the cutout will need to be moved forward 1–3” toward the center of the cushion.
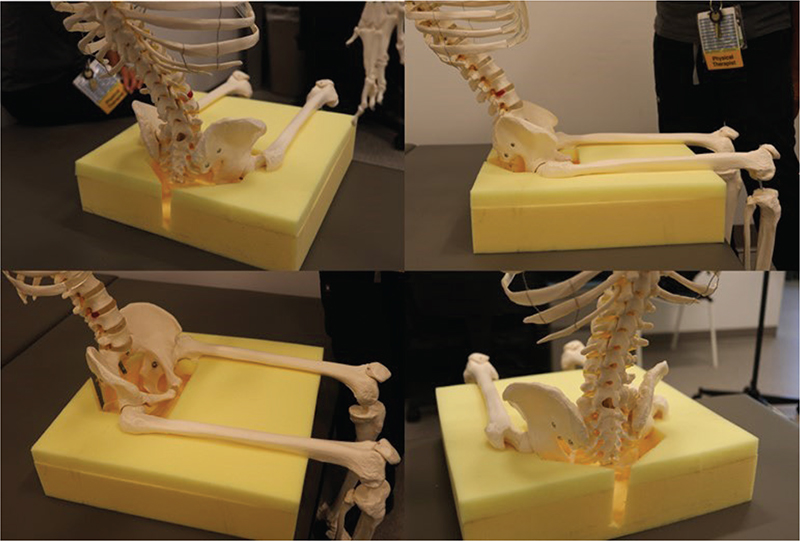
Fig. 6: Adjusting cutout for posterior pelvic tilt, demonstrating the adaptation of the cutout by a V cut to alleviate pressure on the coccyx, with initial confirmation through palpation of the ischial tuberosities.
Pelvic obliquity
If the pelvic obliquity has limited flexibility, a wedge placed under the cushion base itself (not the gel pad under the ischial tuberosity) can assist with reorienting the trunk from leaning laterally to a more midline alignment. For example, as in the picture, for a right pelvic obliquity, a wedge or 1” lift underneath the cushion, under the right hip, will provide lateral stability of pelvis and therefore a more midline trunk (Fig. 7).
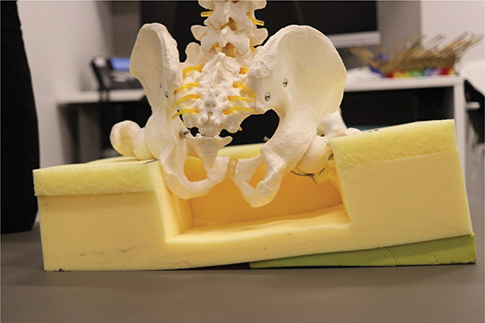
Fig. 7. Wedge placement for addressing pelvic obliquity, showcasing the use of a wedge or 1” lift underneath the cushion to aid in realigning the trunk.
Pre ischial bar
The pre-ischial bar further unweights the ischial tuberosities by placing the pre ischial bar (PIB) in front of the cutout underneath the cushion (Fig. 8). The weight of the legs counterbalances the pelvis upward, out of the cut out. This concept is useful if the person wants a lower cushion height but is bottoming out. For example, someone using an ultralightweight wheelchair with a low back, sitting on a 4” high spring air cushion, makes the back height too low or decreases his ability to push the wheels effectively. The addition of a PIB underneath the 3” cushion will assist in unweighting the ischial tuberosities.
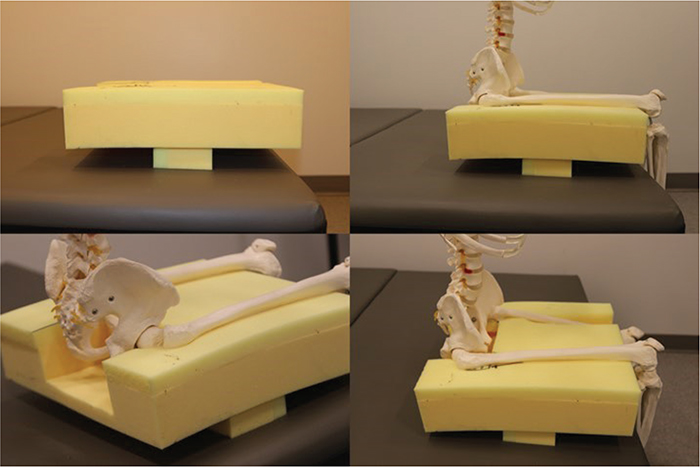
Fig. 8. Pre-ischial bar (PIB) for unweighting ischial tuberosities, demonstrating the placement of the PIB in front of the cushion cutout, effectively raising the pelvis out of the cutout by utilizing leg weight to counterbalance and offering a valuable solution for individuals requiring lower cushion height without bottoming out.
Leg trough
Accommodating a fixed hip extension deformity resulting from heterotrophic ossification is crucial to prevent pelvic obliquity and scoliosis when sitting. When 1 hip lacks 90 degrees of flexion, it forces the pelvis or trunk to lean toward the opposite side. To address this issue, a modification can be made to the foam cushion by cutting a trough that aligns with the fixed deformity (Fig. 9). This trough allows the pelvis to level out, enabling the trunk to assume a more upright posture. By creating this accommodation, the foam cushion provides better support, ensuring that the pelvis remains level and minimizing the risk of postural imbalances. This adjustment aims to improve the individual’s overall seating posture and reduce the potential complications associated with an uneven pelvis and trunk positioning caused by the fixed hip extension deformity.

Fig. 9. Leg trough modification to address fixed hip extension deformity, showcasing the critical adaptation of a foam cushion through the creation of a trough and aligning with the fixed deformity to promote a level pelvis and an upright trunk posture.
Trochanteric cutouts
The trochanters, bony prominences slightly forward and lateral to the ischial tuberosities, can be palpated. When these trochanters become prominent and exhibit signs of redness, off-loading can be achieved through various methods: gridding the top layer of foam to reduce surface tension, tunneling out the firmer foam underneath the softer 4# foam or selectively removing foam specifically under the bony prominences, as depicted in the accompanying picture (Fig. 10).

Fig. 10. Trochanteric cut outs for off-loading, illustrating the techniques to address prominent and reddened trochanters using methods such as gridding the top foam layer, tunneling the firmer foam beneath the softer 4# foam or selectively removing foam under the trochanters.
CASE EXAMPLES ADDRESSING DEFORMITIES
The following is a collection of 5 case examples that highlight the contemporary relevance of FCC. These case examples highlight the importance of tailoring cushions to meet the specific needs of each patient’s unique case.
Case 1
This case report describes a young man with T2 paraplegia, a fixed right pelvic obliquity (where the right side of his pelvis is lower than the left), and a right lumbar curve scoliosis (Video 4). He uses a custom-designed back support and prefers sitting on a ROHO(R) air cushion. To address the issue of him leaning to the right due to his pelvic obliquity, a wedge was placed underneath the ROHO cushion to shift his trunk and weight more toward the midline, improving his trunk stability. This concept of using a wedge can be applied to various types of cushions, including foam cushions and floatation cushions using gel or air, to accommodate fixed deformities and promote a more balanced sitting position (Fig. 11). The goal is to provide better support and balance for individuals with postural challenges.
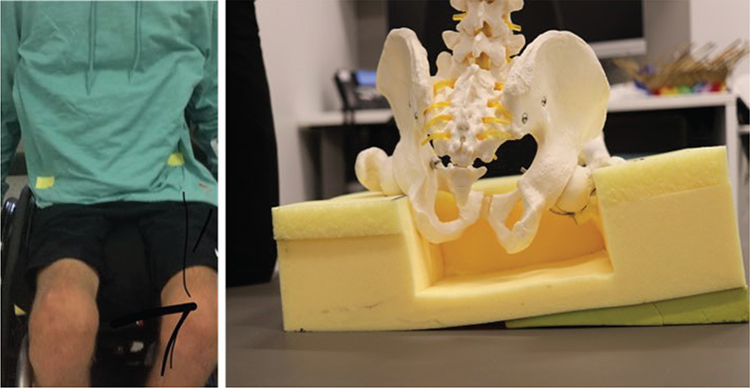
Fig. 11. Application of a wedge to improve trunk stability in a T2 paraplegic patient with fixed right pelvic obliquity and lumbar curve scoliosis, illustrating the concept of using a wedge to shift trunk weight toward the midline, enhancing seating stability and supporting individuals with postural challenges across various cushion types.
Case 2
This case report focuses on a young man with T2 paraplegia who developed collapsing scoliosis, right pelvic rotation, right pelvic obliquity, left hip heterotopic ossification, and pressure sores (Video 5). He was admitted for skin flap surgery and a left hip Girdlestone procedure. Preoperatively, he had difficulty maintaining an upright position in his wheelchair due to spasticity, fixed left hip extension and a collapsing scoliosis.
Postoperatively, the goal was to provide a cushion that could off-load pressure from his ischial tuberosities and accommodate his deformities. A foam cushion was customized with a diagonal cut to address his right-forward pelvic rotation, with the cutout offset to the left by 1 inch to accommodate his right pelvic obliquity (Fig. 12). Additionally, the left side of the cushion was cut 1 inch shorter to accommodate the femur length difference resulting from the Girdlestone procedure.

Fig. 12. Custom foam cushion design for a T2 paraplegic patient post skin flap surgery and left hip girdlestone procedure, featuring a diagonal cut with a one-inch offset to address right-forward pelvic rotation and accommodate right pelvic obliquity, resulting in an improved upright posture. This needs to be under the 5 figs on page 26.
As shown in the pictures, the patient achieved a more upright posture when seated on the custom foam cushion compared to a ROHO cushion (Fig. 12). These custom solutions provided pelvic stability and midline trunk support to improve the patient’s overall seating comfort and posture.
Case 3
This case report discusses the design of a custom-cut cushion for a gentleman with a C6–C7 tetraplegia and fragile, atrophied albino skin (Video 6). Throughout the 35 years since his injury, the patient’s skin had become more vulnerable, requiring modifications to his cushion.
Initially, the cushion had cutouts under the ischial tuberosities and sacral area. However, due to the patient’s evolving needs and changes in his anatomy, the cushion design was adjusted. The posterior femur area became bony, necessitating a complete cutout underneath it. The lower cutout also featured a coccygeal relief to accommodate the patient’s preferred position of stability, a posterior pelvis.
Additionally, the cushion had cutouts for the trochanters and tailbone, which were now modified to be complete cutouts under the trochanters and posterior femur (Fig. 13). Pressure mapping was used to identify areas of increased pressure, helping guide the customization process. The front edge of the cutout was also graded to reduce surface tension for the pubic ramus.
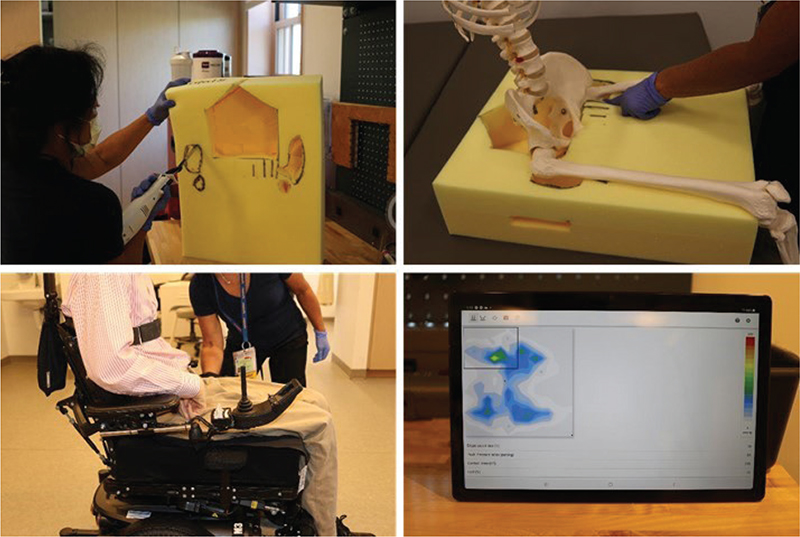
Fig. 13. Custom cushion design for a C6–C7 tetraplegic patient with fragile skin and evolving needs, featuring complete cutouts under the trochanters and posterior femur, coccygeal relief, and graded front edge to reduce surface tension, emphasizing the role of palpation and pressure mapping in tailoring foam cushions to evolving patient anatomy and pressure relief requirements.
The report emphasizes the importance of palpation and pressure mapping as essential tools for designing custom foam cushions. These techniques help ensure that the cushion is tailored to the patient’s specific anatomy and pressure relief needs, especially when dealing with fragile skin and changing conditions over time.
Case 4
This case report involves a patient with a complex medical history, including spinal cord injury, brain injury, and the presence of heterotrophic ossificans (HO) in the left hip and knee (Fig. 14, Video 7). Despite previous surgical intervention for the HO, the patient faced challenges in sitting upright and maintaining balance without upper extremity support due to recurrence of HO in the left hip. As a result, the patient sought a cushion to enhance balance and posture.
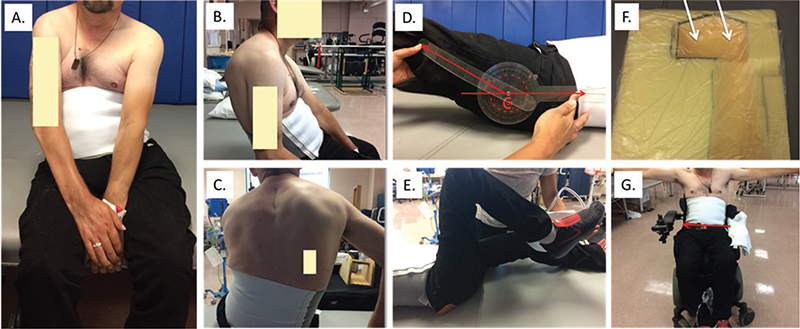
Fig. 14. Comparative illustration depicting the therapeutic impact of a customized foam cutout cushion on the postural challenges for this patient. (A) Frontal view in sitting, R pelvic obliquity and thoracolumbar curve observed with use of hands to balance. (B) Lateral view in sitting, posterior pelvic tilt, decreased lumbar lordosis, and increased thoracic kyphosis observed with use of hands to balance. (C) Posterior view in sitting, R pelvic obliquity, and thoracolumbar curve observed. (D) In supine (mat evaluation), limited L hip range of motion (fixed), pelvic obliquity (flexible), and thoracolumbar curve (semi-flexible). (E) In supine (mat evaluation), R hip flexion and knee flexion (adequate for sitting). Hip and knee extension limited. (F) Foam cut out cushion with trough made on L side to accommodate for the fixed hip extension contracture secondary to H.O. causing R pelvic obliquity and scoliosis. Posterior cutout for bony prominences shifted 1/2” forward and laterally to account for location of the sacrococcyx and ischial tuberosities from palpation. (G) Seated on foam cut out cushion with trough allowing hands-free balance. Semi-flexible pelvis leveled and semi-flexible thoracolumbar improved due to trough accommodating the fixed left hip extension contracture.
A comprehensive evaluation assessing skin integrity, sensation, spasticity, tone, range of motion, strength, and posture was performed. The patient exhibited multiple postural deformities, including right flexible pelvic obliquity (Fig. 14A), right semi-flexible thoracolumbar scoliosis, and fixed left hip extension contracture due to recurrence of HO (Fig. 14B, C).
To address these issues, a FCC was selected as the most suitable solution to accommodate and correct these postural deformities while maintaining transfer status. The customized cushion featured a trough on the left side to accommodate the left fixed hip extension contracture (Fig. 14D, E). This leveled the pelvis and reduced the semi-flexible scoliosis. The cushion also incorporated cutouts under the ischial tuberosities and coccyx to relieve pressure on these bony prominences. Subsequent reassessment of the patient on the foam cushion (Fig. 14F) revealed improved pelvic alignment, upright seated posture, and enhanced balance with raised arms (Fig. 14G).
In summary, this case report highlights the assessment and intervention for a patient with complex postural challenges, culminating in the customization of an FCC to promote stability, balance, and better posture in the patient’s power wheelchair.
SUMMARY
This paper investigates the efficacy of FCCs in preventing pressure injuries among elderly wheelchair users. It offers a historical perspective on FCC development, emphasizing their customization for individual patients. This paper raises awareness about FCC as a viable cushion option and encourages clinicians to consider it. Key points include complete off-loading of high-risk areas, customization benefits, enhanced quality of life, skilled clinician involvement, and the need for more than cushion selection to prevent pressure injuries. This paper concludes by highlighting FCC benefits in patients, such as improved pelvic stability, posture, bony prominence off-loading, and cushion customization.
ACKNOWLEDGEMENTS
We deeply appreciate the collaborative efforts that made this paper possible. We would like to thank Bob Yant, C5 Tetraplegic, founder of Cure Medical, for generous support. We also acknowledge Martin Ferguson-Pell, formerly of the Center for Rehabilitation Technology at Helen Hayes Hospital. We honor the memory of Jim Reswick and John Rogers, key figures in developing the cushion cutting technique, and Dr. Shannon Stauffer, Chief of Spinal Injuries Service at Rancho Los Amigos Hospital. Their contributions continue to advance our mission.
REFERENCES
- Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord 1996; 34: 255–263. https://doi.org/10.1038/sc.1996.46
- Vidal J, Sarrias M. An analysis of the diverse factors concerned with the development of pressure sores in spinal cord injured patients. Paraplegia 1991; 29: 261–267. https://doi.org/10.1038/sc.1991.37
- Preventing Pressure Ulcers in Hospitals. Content last reviewed April 2023. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/index.html.
- Consortium for Spinal Cord Medicine. Paralyzed Veterans of Americs, 2014. Pressure ulcer prevention and treatment following injury: a clinical practice guideline for health-care professional. [cited Oct 2023] Available from: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.mascip.co.uk/wp-content/uploads/2015/05/CPG_Pressure-Ulcer.pdf.
- Shiferaw WS, Akalu TY, Mulugeta H, Aynalem YA. The global burden of pressure ulcers among patients with spinal cord injury: a systematic review and meta-analysis. BMC Musculoskelet Disord 2020; 21: 334. https://doi.org/10.1186/s12891-020-03369-0
- Reswick JB, Rogers JE. Experience at Rancho Los Amigos Hospital With Devices and Techniques to Prevent Pressure Sores. In: Kenedi RM, Cowden JM, editors. Bed sore biomechanics: proceedings of a seminar on tissue ciability and clinical applications organised in association with the Department of Biomedical Engineering, the Institute of Orthopaedics (University of London), Royal National Orthopaedic Hospital, Stanmore, London, and held at the University of Strathclyde, Glasgow, in August, 1975. London: Macmillan Education UK; 1976, p. 301–310.
- McCarthy RE. Management of neuromuscular scoliosis. Orthop Clin N Am 1999; 30: 435–449, viii. https://doi.org/10.1016/S0030-5898(05)70096-1
- Berven S, Bradford DS. Neuromuscular scoliosis: causes of deformity and principles for evaluation and management. Semin Neurol 2002; 22: 167–178. https://doi.org/10.1055/s-2002-36540
- Allam AM, Schwabe AL. Neuromuscular scoliosis. PM & R 2013; 5: 957–963. https://doi.org/10.1016/j.pmrj.2013.05.015
- Ferguson-Pell MW, Wilkie IC, Reswick JB, Barbenel JC. Pressure sore prevention for the wheelchair-bound spinal injury patient. Paraplegia 1980; 18: 42–51. https://doi.org/10.1038/sc.1980.7
- Ferguson-Pell MW. Seat cushion selection. J Rehabil Res Dev Clin Suppl 1990; 2: 49–73.
- Edberg EL, Cerny K, Stauffer ES. Prevention and treatment of pressure sores. Phys Ther 1973; 53: 246–252. https://doi.org/10.1093/ptj/53.3.246
- Key AG, Manley MT, Wakefield E. Pressure redistribution in wheelchair cushion for paraplegics: its application and evaluation. Paraplegia 1979; 16: 403–412. https://doi.org/10.1038/sc.1978.74
- Crane B, Wininger M, Call E. Orthotic-style off-loading wheelchair seat cushion reduces interface pressure under Ischial tuberosities and sacrococcygeal regions. Arch Phys Med Rehabil 2016; 97: 1872–1879. https://doi.org/10.1016/j.apmr.2016.04.004
- Call E, Hetzel T, McLean C, Burton JN, Oberg C. Off loading wheelchair cushion provides best case reduction in tissue deformation as indicated by MRI. J Tissue Viability 2017; 26: 172–179. https://doi.org/10.1016/j.jtv.2017.05.002
- Gefen A. Tissue changes in patients following spinal cord injury and implications for wheelchair cushions and tissue loading: a literature review. Ostomy Wound Manage 2014; 60: 34–45.
- Sonenblum SE, Ma J, Sprigle SH, Hetzel TR, McKay Cathcart J. Measuring the impact of cushion design on buttocks tissue deformation: an MRI approach. J Tissue Viability 2018; 27: 162–172. https://doi.org/10.1016/j.jtv.2018.04.001
- Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil 2001; 82: 529–533. https://doi.org/10.1053/apmr.2001.21854
- Sonenblum SE, Vonk TE, Janssen TW, Sprigle SH. Effects of wheelchair cushions and pressure relief maneuvers on ischial interface pressure and blood flow in people with spinal cord injury. Arch Phys Med Rehabil 2014; 95: 1350–1357. https://doi.org/10.1016/j.apmr.2014.01.007
- Peko Cohen L, Gefen A. Deep tissue loads in the seated buttocks on an off-loading wheelchair cushion versus air-cell-based and foam cushions: finite element studies. Int Wound J 2017; 14: 1327–1334. https://doi.org/10.1111/iwj.12807
- Brienza D, Vallely J, Karg P, Akins J, Gefen A. An MRI investigation of the effects of user anatomy and wheelchair cushion type on tissue deformation. J Tissue Viability 2018; 27: 42–53. https://doi.org/10.1016/j.jtv.2017.04.001
- Kosiak M. Etiology and pathology of ischemic ulcers. Arch Phys Med Rehabil 1959; 40: 62–69.