CASE REPORT
ULTRASONOGRAPHIC PRESENTATION OF NODULAR CYSTIC FAT NECROSIS AFTER A LOW-VELOCITY TRAUMA: A CASE REPORT
Robin de WILDE, MD, Arne HAUTEKIET, MD2, Sybille GEERS, MD1, Luc VANDEN BOSSCHE, MD1, PHD and Martine de MUYNCK, MD1, PHD
From the 1Physical and Rehabilitation Medicine, Ghent University Hospital and 2Physical and Rehabilitation Medicine, Maria Middelares General Hospital, Ghent, Belgium
Objective: Morel-Lavallée lesion is a well-known entity after a high-energy, shearing trauma. Another form of lesion in the subcutaneous tissue is fat necrosis, presenting as a palpable mass. The most common presentation of fat necrosis is oil cysts, which occur mainly in the breast. However, in the lower extremities fat necrosis appears as nodular cystic fat necrosis. We report here a case of a patient with multiple injuries after a low-velocity trauma, who developed fat necrosis.
Results: Six months after the traumatic event the patient reported multiple subcutaneous lumps on the right knee. On ultrasonography, the probable diagnosis of post-traumatic fat necrosis with consequent development of nodular cystic fat necrosis was seen. The diagnosis was confirmed based on magnetic resonance imaging (MRI).
Discussion: Fat necrosis should be included in the differential diagnosis in cases of tissue injuries after a trauma. Fat necrosis can present months or years after the initial injury. It is a benign entity and is the result of an organized haemorrhage, swelling and oedema that progresses with fibrosis. There is no absolute need for surgical treatment.
LAY ABSTRACT
Nodular cystic fat necrosis presents as palpable lumps, most commonly on the lower extremities after a trauma. Patients may report these cystic structures many months after the trauma. This case report illustrates the ultrasonographic appearance of nodular cystic fat necrosis. This is a benign finding that does not require treatment or removal if no pain or aesthetic discomfort is present.
Key words: ultrasonography; trauma; fat necrosis; rehabilitation.
Citation: JRM-CC 2022; 5: jrmcc00083. DOI: https://doi.org/10.2340/jrmcc.v5.2237
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: May 13, 2022; Published: Sep 22, 2022
Correspondence address: Robin De Wilde, Physical and Rehabilitation Medicine, Ghent University Hospital, Corneel Heymanslaan 10, Ghent, Belgium. E-mail: robin.dewilde@uzgent.be
Morel-Lavallée lesion is a well-known entity after a high-energy shearing trauma. It is a closed degloving soft-tissue injury, in which the skin and subcutaneous tissues are separated from the fascia superficial to the underlying muscle plane. Shear injury disrupts perforating vessels and lymphatics, creating a potential space filled with serosanguinous fluid, blood and necrotic fat (1). Another type of lesion found in the subcutaneous tissue is fat necrosis, an isolated benign finding after a variable history of trauma, which presents as a palpable mass within the subcutaneous tissue (2). The best-known form of fat necrosis is oil cysts. These cysts are found mainly in the breast after injury to the fatty breast tissue. Findings of nodular cystic fat necrosis or encapsulated fat necrosis lesions in the extremities are rare (3).
We report here a case of a male patient who had had a low-velocity trauma with crush injury, multiple bone fractures and soft tissue injuries, who presented with distinctive lumps subcutaneously on the right knee joint several months after the initial injury.
CASE REPORT
A 46-year-old Caucasian man was admitted to our rehabilitation department at the Ghent University Hospital following a road traffic accident in which he was hit by a truck while he was cycling. On admission to the emergency department, the patient presented with the following injuries:
- left open trimalleolar fracture, for which he received an open reduction and internal fixation. Associated peripheral nerve injury of the peroneal nerve;
- medial femoral condyle fracture of the right knee, for which he received screw fixation;
- radial neck fracture of the right elbow, with conservative therapy;
- bilateral Morel-Lavallée lesion at the lateral hip regions.
Three weeks after the accident, he started intensive multidisciplinary rehabilitation in an inpatient rehabilitation centre. The patient was transferred to the Plastic Surgery Department for 1 week because there was a need for a free tissue transfer flap to cover the skin lesions of the left anterior ankle.
Six months after the traumatic event, the patient reported multiple subcutaneous lumps at the right knee joint. These nodules were not painful; there was no local heat or redness of the skin. The lumps had not been present at the start of rehabilitation and the patient reported that they were increasing in size.
Ultrasonography of the knee joint was performed, revealing intra-articular fluid and a Pellegrini-Stieda lesion of the medial collateral ligament. In the subcutaneous tissue, medially and laterally, anechogenic structures with a sharp, well-defined edge (Fig. 1) were observed with an associated posterior enhancement.
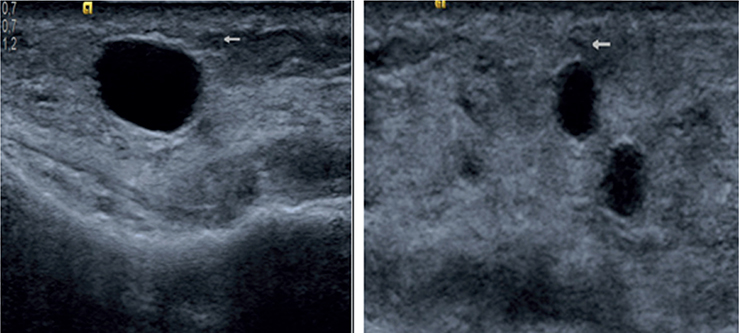
Fig. 1. Ultrasonography images of the medial right knee (14MHz transducer). The sonographic characteristics of these findings are well-defined oval structures with an anechogenic appearance and capsule (arrows). There was no angiogenesis present or oedema around the structures. Some through transmission is present on the left-hand image.
A probable diagnosis of post-traumatic fat necrosis with consequent development of nodular cystic fat necrosis was seen (Fig. 1). An additional magnetic resonance imaging (MRI) scan was performed, confirming the visualized cysts (Fig. 2). The patient was reassured that the findings were benign, and it was explained that no further treatment was necessary at present. Clinical follow-up 6 months later revealed a stable presentation with absence of pain.
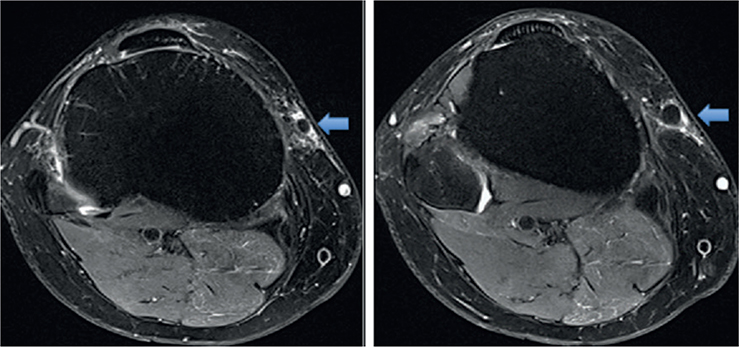
Fig. 2. Magnetic resonance imaging T2 TSE fat suppression transverse sequence of the right knee with nodular cystic fat necrosis (arrows).
DISCUSSION
Epidemiology
The incidence of peripheral fat necrosis after trauma is not well described, with few reports in the literature (4). The lesions usually occur in 2 distinct populations: adolescent boys and middle-aged women, with a predilection for the lower extremities. It can also be found on the upper extremities, trunk and hip (4).
Differential diagnosis of the fat necrosis lesion should include other post-traumatic injuries, such as the well-known Morel-Lavallée lesion, coagulopathy-related haematoma, and rarely, post-traumatic early-stage myositis ossificans with diffuse subcutaneous oedema.
The time between injury and observation of palpable lump deformity is most often prolonged (5). Morel-Lavallée is more commonly found in the primary hours to days after the trauma, but, in one-third of patients, it presents only months or years after the initial injury (1). The duration of the lesions varies in the literature from several weeks to approximately 3 years; however, cases of up to 10 years duration are described in case reports (6).
Pathophysiology
Fat necrosis is a benign entity, frequently described as a palpable mass within the subcutaneous tissue (2). Nodular cystic fat necrosis was first described by Przyjemski & Schuster (6). In comparison with the Morel-Lavallée lesion, there is almost always a prolonged interval between the injury and the initial observation and diagnosis.
The underlying pathophysiology of fat necrosis is not fully known; however, it is agreed by many authors that it is the result of an organized haemorrhage, vascular insufficiency, swelling and oedema, which progresses with fibrosis. This can result in soft-tissue deformity, either from palpable fullness or loss of subcutaneous fat volume (5). Approximately half of the lesions are mobile (4). In 1997 Tsai et al. (5) performed a retrospective cohort study with 13 patients, in which only 23% could recall the initial trauma.
The distinct form of fat necrosis in the breast is known as oil cysts, in which a macroscopic pool of oil develops, rimmed by a thin membrane. The transition of fat necrosis is classified into 4 phases, which describe the relationship between the broad spectrum of imaging characteristics and the underlying pathogenesis (7). In the first, hyperacute, phase vessel damage results in the initial inflammatory reaction, which is characterized by transient arteriolar vasoconstriction with a halo of oedema, caused by the fluid transudation on imaging. In the second phase, or inflammatory phase, the endothelial damage activates the coagulation cascade, which creates the fibrin meshwork, and deposition of granulation tissue and angiogenesis may occur. The third phase consists of the formation of the lipid cyst, which occurs as the local destruction of adipocytes by the release of lipases. This can form a fibrous capsule around the oily fatty acids. The final phase is characterized by a type of foreign-body or chronic granulomatous reaction, resulting in irregular fibrosis or calcification. This occurs only if there is no encapsulation present (7).
Technical investigations
The above-mentioned phases correlate with the different descriptions of these cysts in ultrasonography.
- Phase 1: the hyperacute inflammatory phase correlates with oedematous fat, which is indistinguishable from other aetiology.
- Phase 2: the acute inflammatory phase correlates with homogenous or heterogeneous hyperechoic masses or complex cysts. There may be vascularization with enhancement on power Doppler with granulation tissue, depending on the fibrous staging.
- Phase 3: the lipid cyst formation phase shows round or oval, smooth-bordered, hypo-or an-echoic masses, with variation in appearance depending on wall calcification. This wall calcification increases the hyperechoic border and acoustic shadowing.
- The final phase, when there is no capsulation, can give findings similar to both phases 2 and 3, as described above (8).
In 47.4% of all cases the fat necrosis in the breast presents as cystic masses without through transmission enhancement on ultrasonography (9). Other possible presentations are cystic lesion associated with mural nodules and cystic mass with enhanced through transmission (9). In a study by Walsh et al. in 2008 (2) 5 cases of isolated fat necrosis involving the torso or extremities were identified with a sonographic evaluation, and confirmed pathology reports were reviewed. They concluded 2 different presentations of isolated fat necrosis. One manifestation had a well-defined isoechoic mass with a surrounding hypoechoic halo. This represents the fibrous capsule (2, 8). The other manifestation was that of a poorly defined hyperechoic region in the subcutaneous fat, consistent with cellulitis (i.e. the inflammatory phase) (2).
MRI images also vary, correlating with the pathophysiological phases, and depending on the inflammatory reaction, the liquefied fat and the fibrosis, which determine the signals. The most common appearance is the lipid cyst with hypointense T1-weighted with fat saturation and hyperintense T1-weighted without fat saturation.
The “black hole sign” is also described, meaning a marked hypointensity on Short Tau Inversion Recovery (STIR) images compared with surrounding fat (3, 9).
Differential diagnosis
The differential diagnosis for these images consists of seroma, lipoma, angiomyolipoma (considered a vascular variant of lipoma), epidermal inclusion cyst and dermatofibrosarcoma protuberans (malignant skin tumour).
On ultrasound a seroma can often not be distinguished from an oil cyst. Additional MRI imaging facilitates the differentiation; seromas are hypointense on T1-weighted images (74%), and hyperintense on T2-weighted and STIR images (10).
A lipoma is oblong, with a variable echogenicity depending on the presence of interspersed fibrous tissue (which creates a hyperechoic appearance). The epidermal inclusion cyst should be kept in mind in the presence of increased posterior through-transmission (2).
Treatment
No surgical treatment is necessary for palpable areas of fat necrosis; they may remain unchanged, regress or resolve (3).
Aspiration or surgical excision are options if pain or aesthetic discomfort are present. A modest aspiration by using a syringe and a hypodermic 18-gauge needle is described for fat necrosis of the breast, mainly in the case of oily fluid and if the patient has discomfort (9). Depending on the size of the defect after excision, fat grafting or local tissue rearrangement may be necessary (3).
CONCLUSION
This case report shows a distinctive picture of fat necrosis, in the form of nodular cystic fat necrosis. This presentation is rare, in contrast to the typical lesion of oil cysts, described in the breast. It can manifest in the extremities months after the initial trauma. It is a benign entity that does not need further treatment and can present with a variable appearance during ultrasonography. The most common appearance of these cysts is a hypoechoic mass with smooth margins and without significant acoustic enhancement. The variable characteristics of fat necrosis on ultrasound correlate with the underlying pathophysiology, consisting of 4 phases, ranging from the hyperacute inflammatory phase to the chronic granulomatous reaction. MRI can be used to confirm the diagnosis, mainly through differentiation from seromas.
ACKNOWLEDGEMENTS
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No funding was received.
REFERENCES
- De Coninck T, Vanhoenacker F, Verstraete K. Imaging features of Morel-Lavallée lesions. J Belg Soc Radiol 2017; 101(suppl. 2).
- Walsh M, Jacobson JA, Kim SM, Lucas DR, Morag Y, Fessell DP. Sonography of fat necrosis involving the extremity and torso with magnetic resonance imaging and histologic correlation. J Ultrasonography Med 2008: 1751–1757.
- Vopat BG, Wong JE, Hazzard S, Golijanin P, Palmar WE, Asnis PD. Encapsulated fat necrosis lesion caused by Morel-Lavallée lesion in a professional ice hockey player. Am J Orthop (Belle Mead NJ) 2017: E144–E147.
- Lee SJ, Lee WC, Jang YH, Kim DW, Chung SL, Bae HI. Two cases of nodular cystic fat necrosis possibly related to previous trauma. Ann Dermatol 2004 Jan; 16(1): 19–22.
- Tsai TS, Evans HA, Donnelly LF, Bisset GS 3rd, Emery KH. Fat necrosis after trauma: a benign cause of palpable lumps in children. AJR Am J Roentgenol 1997 Jan; 16(1): 19–22.
- Oh CW, Kim KH. A case of nodular cystic fat necrosis: the end stage lesion showing calcification and lipomembranous changes. J Dermatol 1998: 616–621.
- Tayyab SJ, Adrada BE, Rauch GM, Yang WT. A pictorial review: multimodality imaging of benign and suspicious features of fat necrosis in the breast. Br J Radiol 2018 Dec; 91(1092): 20180213.
- Ganau S, Tortajada L, Escribano F, Andreu X, Sentís M. The great mimicker: fat necrosis of the breast – magnetic resonance mammography approach. Curr Probl Diagn Radiol 2009: 189–197.
- Vasei N, Shishegar A, Ghalkhani F, Darvishi M. Fat necrosis in the breast: a systematic review of clinical. Lipids Health Dis 2019; 18: 139.
- Davies AM, Hall AD, Strouhal PD, Evans N, Grimer RJ. The MR imaging appearances and natural history of seromas following excision of soft tissue tumours. Eur Radiol 2004: 1196–1202.