ORIGINAL REPORT
IMPACT OF STATIC PROGRESSIVE STRETCH ON RANGE OF MOTION AFTER TOTAL KNEE REPLACEMENT IN PATIENTS WITH HAEMOPHILIA
Borut POMPE, MD, PHD, Simona FILIPIDIS, MD and Petra DOVČ, PT
From the Clinic of Orthopaedic Surgery, Ljubljana University Medical Centre, Ljubljana, Slovenia
Background: Haemophilic arthropathy is often associated with a loss of range of motion. Total knee arthroplasty is an effective treatment option for patients with end-stage haemophilic arthropathy of the knee. However, even after arthroplasty, the range of motion sometimes remains insufficient.
Objective: To evaluate static progressive stretch as a treatment method for haemophilic patients with decreased range of motion after total knee arthroplasty.
Methods: Static progressive stretch was used to improve range of motion in patients with a postoperative extension lag of more than 10° and flexion of less than 80°. A total of 7 knees were treated for a mean of 21.7 weeks.
Results: Statistically significant increases in range of motion and in Knee Society Score were observed when comparing pre-treatment and post-treatment values.
Conclusions: Static progressive stretch using an orthotic device could be a successful adjuvant method for treating joint stiffness in patients with haemophilia after total knee arthroplasty.
LAY ABSTRACT
Haemophilic arthropathy often results in loss of range of motion. Total knee arthroplasty is an effective treatment option for patients with end-stage haemophilic arthropathy of the knee. However, despite arthroplasty, the range of motion is sometimes insufficient. Static progressive stretch using special knee orthoses is an adjunct technique to traditional physiotherapy, intending to restore functional range of motion and decrease knee stiffness and pain. The aim of this study was to evaluate static progressive stretch as a treatment method for haemophilic patients with decreased range of motion after total knee arthroplasty.
Key words: haemophilic arthropathy; joint contracture; total knee arthroplasty; static progressive stretch.
Citation: JRM-CC 2022; 5: jrmcc00081. DOI: https://doi.org/10.2340/jrmcc.v5.2285
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Mar 3, 2022; Published: Jun 22, 2022
Correspondence address: Borut Pompe, Clinic of Orthopaedic Surgery, Ljubljana University Medical Centre, Zaloška 9, SI-1000 Ljubljana, Slovenia. E-mail: borut.pompe@guest.arnes.si
Competing interests and funding: The authors have no conflicts of interest to declare.
Haemophilic arthropathy results in severe arthritic changes in the joints due to recurrent haemarthrosis. The most commonly affected joint is the knee. This condition is associated with decreased range of motion (ROM) and joint contractures. In the end-stage of the disease, ankyloses of the joint can occur. As a result, patients experience pain, swelling and functional impairment. Total knee arthroplasty (TKA) is an effective treatment option for patients with end-stage haemophilic arthropathy of the knee (1, 2). However, even after TKA, the range of motion sometimes remains insufficient. Several treatment options and conventional physiotherapy can improve the range of motion (3). Knee manipulation under anaesthesia and arthroscopic or open arthrolysis are most common (4). Pharmaceutical techniques have also been described, including high-dose steroids and intra-articular administration of anakinra (an interleukin (IL)-1R antagonist) (4, 5). The method of serial casting or extension orthoses has been described as a successful pre-surgical treatment technique for haemophilic arthropathy when knee contractures are present (6). The disadvantage of these methods is prolonged immobilization. Therefore, static progressive stretch using removable orthoses between treatment sessions is an adjunctive technique to traditional physiotherapy to restore functional ROM in stiff knees. Numerous studies have shown the efficacy of these orthoses (Joint Active Systems, Inc., Effingham, IL, USA (JAS)) for treating stiff knees in non-haemophilic patients after TKA (7, 8). The aim of this study was to evaluate static progressive stretch as a treatment method for haemophilic patients with decreased ROM after TKA (Fig. 1).

Fig. 1. Joint Active Systems, Inc., Effingham, IL, USA (JAS) knee device was used by patients 2-3 times per day in 30-min treatment sessions.
METHODS
Twenty-six consecutive haemophilic patients who had undergone TKA in our department from 2010 to 2018 were analysed. Some of them had been operated on bilaterally, and a total of 35 TKAs had been reviewed for inclusion in the study. The inclusion criterion for the study was insufficient ROM. The study group comprised patients whose active flexion was less than 80° or whose extension lag was more than 10°. Five patients (7 knees) were found to fulfil those criteria, and they were involved in the study for a mean of 65 months (range 16–190 months) after TKA. The mean age of the subjects was 54.2 years (standard deviation (SD) 8.8 years). Each patient had previously received standard physiotherapy. The patients were additionally treated with the JAS orthosis, which utilized the principles of static progressive stretch for a mean of 21.7 weeks (range 9–30 weeks). Patients were instructed on how to use the JAS orthosis (Fig. 1). All patients received custom-made orthoses based on their height, and thigh and shin diameters. The JAS orthosis is composed of thigh and shin units that are connected and can be adjusted from 50° of flexion to a maximum of 148° of flexion by rotating the therapy knob when the JAS flexion orthosis is used. When the JAS extension orthosis is used, the therapeutic arc of motion is from 48° of flexion to 38° of hyperextension; again, the therapy knob is used to adjust the angle. In the first step, the patient was instructed to rotate the therapy knob until a gentle, pain-free stretch was felt (level 2–3 on the stretch intensity scale, where 0 means no stretch and 10 means a painful stretch). Then, the patient held the stretch position for 5 min and the stretch level was re-assessed. If the stretch intensity decreased, the patient was instructed to rotate the knob until they felt a level 2–3 level stretch again. If the stretching intensity did not change, the patient remained in the same position for another 5 min. If the stretch intensity increased, the patient was instructed to rotate the knob in the opposite direction until a level 2–3 stretch was reached. The stretching sensation was re-assessed every 5 min for a total of 6 blocks (a 30-min therapy session). When the 30-min session was completed, the patient released the knob until the stretch was relieved and then removed the device. The JAS orthosis was used in 2 30-min self-treatment sessions per day.
Every week, the ROM was measured with a goniometer. In addition, the outcome was measured using the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Knee Society Score (KSS) before and after the course of treatment.
For statistical analysis, SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA) was used. Student’s t-test was performed, and the results were considered statistically significant when the p-value was less than 0.05.
The Medical Ethics Committee of Slovenia approved the study i.d. number: 0120-91/2018/4. The study conformed to the principles of the Declaration of Helsinki. Informed consent was obtained from all patients included in the study.
RESULTS
Comparison of pre- and post-treatment values showed that the ROM in the study group increased. Measurements of ROM for each knee are shown in Fig. 2. The mean extension lag decreased and the mean flexion of the knee increased. The changes were statistically significant (p < 0.05). The mean pre-treatment extension lag was 20° (range, 15–30°), and the mean post-treatment extension lag was 15° (range 10–20°); meanwhile, the mean pre-treatment flexion was 84° (range 55–100°), and the mean post-treatment flexion was 89° (range 65–110°) (Fig. 3). No statistically significant change was found between pre- and post-treatment KOOS values. A statistically significant improvement was found in the KSS between the pre-treatment and post-treatment time-points (p < 0.05). The mean pre-treatment KSS score was 64.8 points (range 55.5–77.5), whereas the mean post-treatment KSS score was 67.7 points (range 56.5–81). Clinical data are shown in Table I.
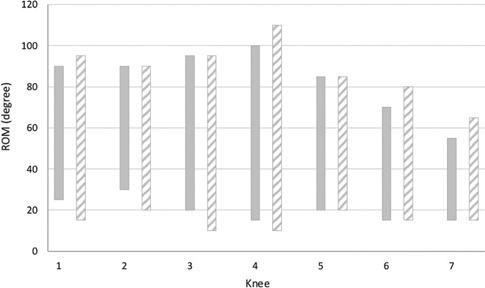
Fig. 2. Pre-treatment (grey) and post-treatment (pattern) value of the range of motion (ROM) for each examined knee.
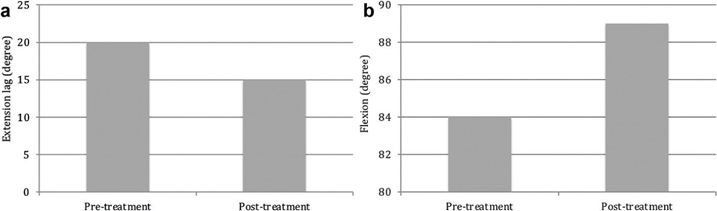
Fig. 3. (a) Mean pre-treatment and post-treatment extension lag. (b) Mean pre-treatment and post-treatment flexion.
| Knee | KOOS – Pain, pre–post-treatment | KOOS – Symptoms, pre–post-treatment | KOOS – FDL, pre–post-treatment | KOOS-FSR, pre–post-treatment | KOOS-QoL, pre–post-treatment | KSS*, pre–post-treatment |
| 1 | 77.8–77.8 | 71.4–64.3 | 92.6–82.3 | 20–20 | 87.5–87.5 | 59–64 |
| 2 | 69.4–77.8 | 64.3–64.2 | 72.1–76.5 | 10–0 | 87.5–87.5 | 59–59 |
| 3 | 100–100 | 71.4–71.4 | 100–72.1 | 20–20 | 31.2–37.5 | 64.5–65.5 |
| 4 | 85.7–97.2 | 100–67.9 | 95.6–100 | 20–20 | 75–81.2 | 74.5–79.5 |
| 5 | 85.7–97.2 | 100–67.8 | 95–100 | 20–20 | 75–81.2 | 77.5–81 |
| 6 | 88.9–88.9 | 57.1–57.1 | 52.9–52.9 | 0–0 | 0–0 | 55.5–56.5 |
| 7 | 80.6–72.2 | 39.3–42.9 | 83.8–73.5 | 0–0 | 62.5–56.2 | 63.5–68.5 |
| Mean | 84.0–87.3 | 71.9–62.2 | 84.6–79.6 | 12.8–11.4 | 59.8–61.6 | 64.8–67.7 |
| SD | 9.5–11.3 | 22–9.6 | 16.8–16.6 | 9.5–10.7 | 32.6–32.9 | 8.3–9.5 |
| FDL: Function in Daily Living; FSR: Function in Sport and Recreation; QoL: Quality of Life. *p < 0.05. | ||||||
DISCUSSION
The method of static progressive stretch using an orthotic device to treat insufficient ROM in haemophilic patients is very similar to that of serial plasters (6). The advantages of the method described here compared with the casting method are: (i) patients can control the intensity of the stretch; and (ii) the treatment is limited to 2 30-min sessions daily, whereas, in the traditional serial casting method, patients must wear the plaster cast for several weeks (6). Haemophilic patients often have a severely limited ROM due to preoperative haemophilic arthropathy. Therefore, it is crucial to correct contracture as much as possible during TKA. The goal is to achieve a functional ROM and correct flexion contracture to nearly 0° (9). It is well known that the degree of flexion is often decreased in haemophilic patients after TKA and that there is a correlation between preoperative and postoperative ROM (10, 11). In general, TKA has worse clinical outcomes in haemophilic patients than in non-haemophilic patients but can nevertheless improve the condition of the patient and the functional ROM of the joint (10).
Static progressive stretching using an orthotic device is a successful method for treating joint stiffness in non-haemophilic populations (7, 8). The current study also found improvements in ROM and increased KSS when comparing pre- and post-treatment values. However, the difference was not as prominent in these patients as it is reported to be in non-haemophilic stiff knees (7, 8). Most of the current patients reported reduced knee stiffness and improved joint function.
This study has several limitations. The analysis was performed in haemophilic patients 65 months (range 16–190 months) after TKA. This might contribute to the inferior clinical results in haemophilic compared with non-haemophilic populations. Therefore, it is possible that the results might be improved through the use of a modified treatment protocol for insufficient ROM after TKA. The study evaluated only 7 knees in 5 patients. Due to the small study group and the short observation period, further studies are necessary to assess the value of these results.
Nevertheless, this study supports the use of static progressive stretch orthoses as an effective treatment option for decreased ROM after TKA in patients with haemophilia.
ACKNOWLEDGEMENTS
We thank Peter M. Bonutti, MD, for support of this study. In addition, we thank the American Journal Expert group for their professional English language editing services.
REFERENCES
- Goddard NJ, Rodriguez-Merchan EC, Wiedel JD. Total knee replacement in haemophilia. Haemophilia 2002; 8: 382–386.
- Mortazavi SM, Haghpanah B, Ebrahiminasab MM, Baghdadi T, Toogeh G. Functional outcome of total knee arthroplasty in patients with haemophilia. Haemophilia 2016; 22: 919–924.
- Alrawashdeh W, Eschweiler J, Migliorini F, El Many Y, Tingart M, Rath B. Effectiveness of total knee arthroplasty rehabilitation programmes: a systematic review and meta-analysis. J Rehabil Med 2021; 53: jrm00200.
- Werner S, Jacofsky M, Kocisky S, Jacofsky D. A Standardized protocol for the treatment of early postoperative stiffness following total knee arthroplasty. J Knee Surg 2015; 28: 425–427.
- Brown CA, Toth AP, Magnussen B. Clinical benefits of intra-articular anakinra for arthrofibrosis. Orthopedics 2010; 33: 877.
- Fernandez-Palazzi F, Battistella LR. Non-operative treatment of flexion contracture of the knee in haemophilia. Haemophilia 1999; 5: S20–S24.
- Bonutti PM, Marulanda GA, McGrath MS, Mont MA, Zywiel MG. Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2010; 18: 194–199.
- Bonutti PM, McGrath MS, Ulrich SD, McKenzie SA, Seyler TM, Mont MA. Static progressive stretch for the treatment of knee stiffness. Knee 2008; 15: 272–276.
- Rodriguez-Merchan EC. Correction of fixed contractures during total knee arthroplasty in haemophiliacs. Haemophilia 1999: 5: S33–S38.
- Strauss AC, Schmolders J, Friedrich MJ, Pflugmacher R, Muller MC, et al. Outcome after total knee arthroplasty in haemophilic patients with stiff knees. Haemophilia 2015; 21: 300–305.
- Massin P, Petit A, Odri G, Ducellier F, Sabatier C, Lautridou C, et al. Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Orthop Traumatol Surg Res 2009; 95: S7–S12.