ORIGINAL REPORT
EFFECTS OF A SEMI-RIGID KNEE BRACE ON MOBILITY AND PAIN IN PEOPLE WITH KNEE OSTEOARTHRITIS
Tim DRIES, MSC1, Jan Willem VAN DER WINDT, MSC2, Wouter AKKERMAN, CPO3, Mari KLUIJTMANS, CPO4 AND Rob P. A. JANSSEN, MD PHD5–7
From 1Livit Orthopedie, Dordrecht, 2,3Livit Orthopedie, Amsterdam, 4Livit Orthopedie, Eindhoven, 5Department of Orthopaedic Surgery & Trauma, Máxima Medical Center, Eindhoven-Veldhoven, 6Orthopaedic Biomechanics, Department of Biomedical Engineering, Eindhoven University of Technology and 7Value-Based Health Care, Department of Paramedical Sciences, Fontys University of Applied Sciences, Eindhoven, The Netherlands
Objective: Osteoarthritis is one of the most common chronic conditions leading to disability among older people (age 60+ years). Knee osteoarthritis has a significant impact on daily functioning. Pain, stiffness, reduced strength, changes in posture, and reduced knee stability may result in reduced mobility. The aim of this study is to evaluate the short- and long-term effects of conservative therapeutic use of a semi-rigid knee brace for management of patients with knee osteoarthritis, using patient-reported outcomes.
Design: Patients with osteoarthritis using a semi-rigid knee brace were asked to complete a questionnaire about the effectiveness of the brace after wearing it for 3 weeks. The primary outcome measure was mobility, assessed using an ordinal scale with and without use of the knee brace. Secondary outcome measures were pain symptoms and overall daily functioning.
Results: A total of 381 patients completed the questionnaire. The results show considerably improved mobility while using a knee brace in different mobility groups. In the group of respondents who were limited to their home environment mobility decreased by 74% while using a knee brace. In the group of respondents who were able to walk to a nearby shop mobility increased by 50%, and the group experiencing no mobility restrictions increased from 3% without using a knee brace to 13% while using a knee brace. In addition, 54% of respondents reported a reduction in pain symptoms and 62% of respondents reported an improvement in overall daily functioning while using a knee brace.
Conclusion: The results of this large-scale patient-reported outcome measure (PROM) study show that the use of a semi-rigid knee brace appears to provide suitable joint support, offering pain relief and freedom of movement and should be considered a useful non-surgical treatment method for use in patients with knee osteoarthritis
Clinical trial: This study does not include a clinical trial.
LAY ABSTRACT
This study of patient-reported outcome measures regarding the use of stabilizing knee braces for knee osteoarthritis provides insight into the additional care and quality of life provided by the use of these orthopaedic aids. The aims of this study are to measure the effectiveness of knee braces in daily life and to validate the efficacy of using orthopeadic medical aids.In the study, 381 patients with knee Osteoarthritis were provided with knee braces and were asked about the effectiveness of the braces 3 weeks after they first started wearing them. This large-scale study found that the use of knee braces contributed to user-mobility, reduced pain, and increased the possibility to perform daily activities. Knee braces appear to serve as a suitable support for knee joints, providing pain relief and freedom of movement, and should be considered a useful non-surgical treatment method for knee Osteoarthritis.
Key words: osteoarthritis; arthritis; knee brace; orthotic device; unload.
Citation: JRM-CC 2022; 5: jrmcc00085. DOI: http://dx.doi.org/10.2340/jrmcc.v5.2483
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Apr 29, 2022; Published: Jul 5, 2022
Correspondence address: Jan Willem van der Windt, Kabelweg 40, 1014 BB Amsterdam, The Netherlands. E-mail: jwindt@livit.nl
Osteoarthritis (OA) is one of the most common chronic conditions leading to disability among older people (age 60+ years) (1–5). Knee OA has a significant impact on daily functioning. Pain, stiffness, reduced strength, changes in posture, and reduced knee stability may cause reduced mobility (6).
Usually, a stepped care treatment plan is implemented, whereby more complex treatments, e.g. surgical interventions, are considered only when lesser complex treatments are found unsuitable. According to the Osteoarthritis Research Society International (OARSI) in the USA and the UK National Institute for Health and Care Excellence (NICE) guidelines, conservative management comprises a combination of education for self-management, exercise therapy (aerobic and strength exercise), weight management, knee braces, and pain medication. Under the Dutch national Federation of Medical Specialists (FMS) guidelines, a valgus knee brace is prescribed for patients with symptomatic medial tibiofemoral OA, where the effectiveness of other conservative management options has proven insufficient. Use of a valgus knee brace aims to delay joint replacement surgery for as long as possible, especially in relatively young and active patients (6).
Several systematic reviews have quantified the effectiveness of unloader braces in improving clinical outcomes and mechanical leverage (6–8). However, to the best of our knowledge, there is a significant research gap in perception-based studies in understanding the short- and long-term consequences of these braces on the tissues in the knee joint, including the cartilage and ligaments. Current perception-based studies are based on relatively small population sizes (9–11), and further research is needed to advance our understanding of the effects of unloader braces experienced by patients with OA.
The objective of this perception-based evaluation study is to evaluate the short- and long-term effects of a semi-rigid knee brace in patients with knee OA.
METHODS
Measurement of perception-based outcomes among patients is used to evaluate health outcomes and quality of life and to provide insight into the value of patient care (12, 13). For this study, the patient-reported outcome measurement (PROM) toolbox of the Netherlands Healthcare Institute, and the Netherlands Federation of University Medical Centres (NFU) guidelines for the selection of Patient Reported Outcomes (PROs) and PROMs were used (14–16). An illness or condition often causes complaints and symptoms, such as pain, which relate to problems with daily functioning. Retrospective measurements provide insight into the effect a treatment has on a patient’s perceived health in terms of their physical well-being and/or functioning. In this study, subjects were questioned about symptoms, functional status, and perceived health. The following PROs were defined to determine the effectiveness of the knee braces:
- How has your general daily functioning changed since using your knee brace?
- How have your pain symptoms changed since using your knee brace?
- Please indicate how mobile you are with/without the knee brace?
Information about health prior to and after an intervention is needed to improve the effectiveness of using a knee brace. This study compared feedback from patients about function gained with and without a semi-rigid knee brace. There are no standard or target values that could be used in the study, as there are no comparable studies regarding the effectiveness of these orthopaedic aids. The PROM questions in the study were prepared based on the usual questionnaires used in orthopaedics (surgery), thus, adhering to scientifically accepted and validated PROM questions (13, 17).
Between October 2018 and December 2020, a total of 1,003 patients with OA who were provided with a knee brace (both new users and repeat users) were invited to complete a questionnaire about the effectiveness of the brace after wearing it for 3 weeks. Patients received their knee brace from a qualified certified prosthetist/orthotist (CPO) and were mostly referred to the CPO by medical doctors. The questionnaires were sent by e-mail, and patients were informed that responding to the questionnaire was voluntary. In addition, informed consent was given. The questionnaire contained questions related to pain perception and daily functioning, each with a qualitative ordinal scale (7-point scale ranging from “very deteriorated” to “improved significantly”). Using these questions, patients were encouraged to compare their pain perception and daily functioning at the time of the survey with their perceived perception and functioning 3 weeks earlier. Mobility was expressed in meters. The primary outcome measure was mobility assessed with and without using the semi-rigid knee brace. Secondary outcome measures were pain symptoms and overall daily functioning assessed with the 7-point ordinal scale. Age and sex were also documented.
Descriptive statistics were used as basic measures to describe the survey data. They consist of summary descriptions of frequency and percentage response distributions, and mode was used to measure the central tendency (18).
With a population size of 4,025 patients provided with a semi-rigid knee brace in the Netherlands during the study period and a 95%, confidence level, a margin of error of 5% was calculated. This expresses the amount of random sampling error in the results of this survey.
The diagnosis of OA was confirmed by a medical doctor (MD) for all patients. The diagnosis was mostly made based on X-rays and/or magnetic resonance imaging (MRI). Patients throughout the Netherlands in various institutions, ranging from university hospitals and rehabilitation centres to nursing homes, were eligible for this study if the MD recommended use of a knee brace. Patients with OA were randomly allocated to treatment with a conventional semi-rigid knee brace (Agillium Reactive®, Ottobock ,Duderstadt, Germany or Defiance®, DJO, Lewisville, TX, U.S.A (Fig. 1). Both braces were selected for their unloading capabilities, and were supplied to the patient by a qualified CPO.

Fig. 1. Types of knee brace used in this study.
RESULTS
A total of 381 out of 1,003 patients completed the outcome study questionnaire; a response rate of 38%. All responses were analysed and included in this study as acceptable data.
Table I shows the descriptive characteristics of the study population. In total, 63% of respondents were aged 60 years or over, and 30% were aged 70 years or over. This age range also matches the greatest prevalence and incidence rates of OA, where the majority of people over 55 years of age have radiological features of OA (19). The majority of respondents (60%) in this study were women.
Fig. 2 shows the results regarding the change in mobility for all respondents. Mobility while using a knee brace improved considerably in different mobility groups. The mobility of respondents who were limited to their home environment reduced by 74%. The mobility of the respondents who were able to walk to a nearby shop increased by 50%, and the group experiencing mobility restrictions increased from 3% without using a knee brace to 13% while using a knee brace. A total of 42% of respondents using a knee brace indicated that they could take a long walk again (18%) or go to the local shop (24%). 80% of mobility improvement is noted for the combined three higher mobility classes (d,e andf in Table II). Only 9% of patients were limited to their own living environment while using a knee brace.
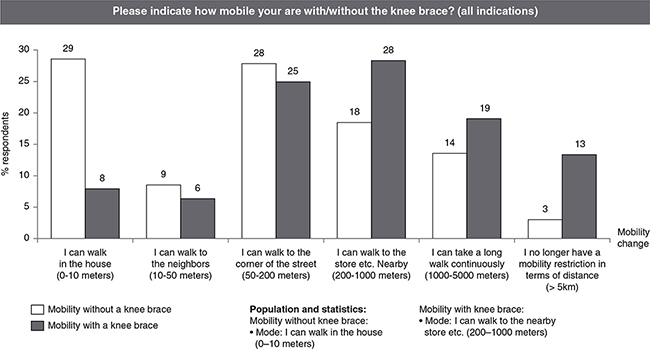
Fig. 2. Results for the question: “Please indicate how mobile you are with/without the knee brace?” (OA indication)
Fig. 3 shows the results for the reduction in pain symptoms. The group wearing a knee brace showed an improvement (reduction) in pain symptoms of 54%. Of the respondents, 29% reported that their pain symptoms were reduced significantly or very significantly, while 36% experienced no change. A small difference was noted between new users and repeat users; new users showed greater improvement (61% for new users and 44% for repeat users) and less deterioration (3% for new users and 16% for repeat users).
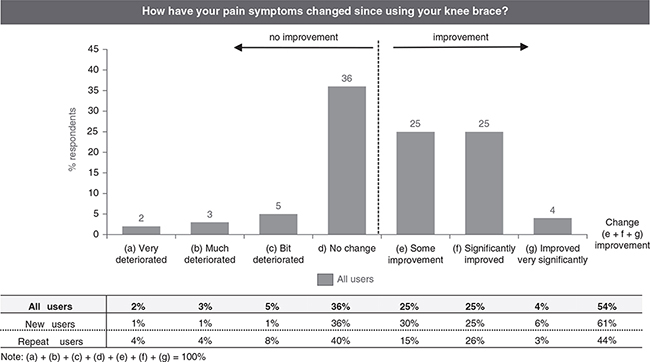
Fig. 3. Results for the question: “How have your pain symptoms changed since using your knee brace?”
Fig. 4 shows the results for change in overall daily functioning while using a knee brace. Sixty-two percent of respondents indicated that their general daily functioning improved after they started using a knee brace, 29% indicated that it improved significantly, and 7% very significantly. There was a small difference between the improvement in patients who started using a knee brace (new users indicate an improvement of 69%) and patients who continued the treatment with a knee brace (repeat users indicate an improvement of 60%). Nine percent of all respondents stated that their functioning deteriorated after using the knee brace.
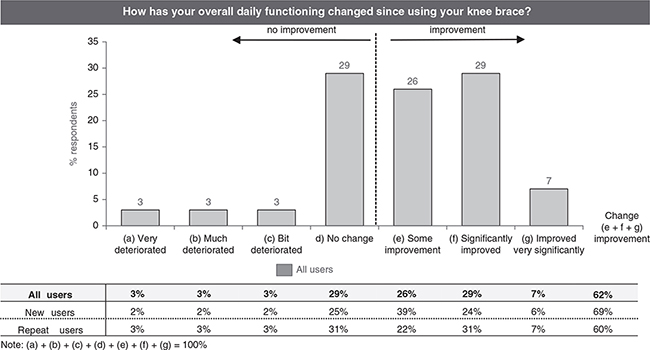
Fig. 4. Results for the question: “How has your overall daily functioning changed since using your knee brace?”
Table II shows the mobility results for both new and repeat users with or without using a knee brace. In the low mobility class (class a – I can walk in the house (0–10 meters), a difference was reported between repeat users (39% of respondents could walk 0–10 m without using a brace, and 10% with using a brace) and new users (24% of the respondents could walk 0–10 m without using a brace, and 6% with using a brace). In addition, a difference was also noted in the highest mobility class between repeat users (class f – I no longer have a mobility restriction in terms of distance (> 5 km) - is 5% for repeat users without using a brace and 17% with using a brace) and new users (class f is 0% without using a brace and 6% with using a brace). It can be concluded that the distribution of results is skewed more towards the extreme mobility classes (low and high) for repeat users than for new users.
Table III compares a combination of mobility classes with and without a knee brace. When combining the low mobility classes, the low mobility group (class a and b combined) of users without using a knee brace is predominated by repeat users compared to new users, as 45% of respondents who are repeat users are in this lowest mobility group compared with 30% for new users. When using a knee brace, the amount of users in the low mobility group was decreased with 60% for new users and 64% for repeat users. The amount of new users in the high mobility group (class e and f combined) increased by +192% when wearing a knee brace (35% of the new users indicated to be in the high mobility group when using a knee brace, compared to 12% when not using a knee brace). For repeat users the amount of users in the high mobility group was increased by +43%, comparing the amount of repeat users while use a knee brace (30%) with the amount of repeat users without using a knee brace (21%) in the same mobility group.
| Mobility without knee brace | Mobility with knee brace | *Change | |||||
| Low mobility classes | (a) 0–10 m | (b) 10–50 m | (a+b) Total | (c) 0–10 m | (d) 10–50 m | (c+d) Total | % |
| All users | 34% | 6% | 39% | 9% | 6% | 15% | –62 |
| New users | 24% | 6% | 30% | 6% | 6% | 12% | –60 |
| Repeat users | 39% | 6% | 45% | 10% | 6% | 16% | –64 |
| High mobility classes | (e) 1–5 km | (f) No restriction | (e+f) Total | (g) 1–5 km | (h) No restriction | (g+h) Total | % |
| All users | 15% | 3% | 17% | 18% | 13% | 31% | 82 |
| New users | 12% | 0% | 12% | 29% | 6% | 35% | 192 |
| Repeat users | 16% | 5% | 21% | 13% | 17% | 30% | 43 |
| *Change in mobility is expressed as % of the population | |||||||
DISCUSSION
This study measured the short- and long-term effects of use of a semi-rigid knee brace in patients with knee OA, using a perception-based evaluation. The results showed that 62% of all respondents indicated an improvement in daily functioning after starting using a knee brace. In a previous study comparing a braced patient group with a control group, in which patients received only conservative management without knee bracing, the patient group reported an improvement of 50% improvement in mobility, whereas the control group reported an improvement of 36% (20). Our study supports the findings that knee bracing improves daily functioning; we note an even higher improvement for patients using a knee brace based on a larger population (62%).
Gained mobility
The results of this study support the findings of a 2012 PROM study by Briggs et al. (7), which showed a significant improvement in quality of life using a 12-item Short Form health survey (SF-12) (p<0.05) and pain, stiffness, and function using Western Ontario and McMaster Universities Arthritis Index (WOMAC) (p<0.05) while using a brace, based on a study of 39 patients. The larger population size in the current study strengthens these findings; braces, specifically designed to unload the degenerative compartment of the knee, can be an effective treatment to decrease pain and maintain activity level.
This study builds on earlier perception-based studies in specifying the improved quality of life in gained mobility among mobility classes (21, 22). Whilst using a knee brace, 55% of respondents indicated that their mobility was improved; they could take a long walk again (24% of respondents), go to the local shop (18% of respondents), or no longer experienced any mobility restrictions (13% of respondents). The use of the knee brace increased mobility by 83% in these 3 groups combined. Furthermore, a 69% reduction in patients limited to their own living environment was found when comparing the group using a knee brace (8% of respondents) with the group not using a knee brace (29% of respondents). In the scope of this study, the authors are not aware of any previous research into the effect of knee bracing in different mobility classes.
Pain reduction
This study found that pain symptoms were reduced when using a knee brace. This finding is supported by previous studies, in which Briggs et al. reported a significant improvement in pain and function (7). They have also shown that most knee braces users (69%) found pain relief to be a very important reason to continue using the brace. This is supported by Kiel & Kaiser, showing that knee bracing resulted in a broader medial joint space when walking (23), while the medial joint space is presented as a major contributor to perceived pain symptoms.
The results of this study particularize the reduction in pain obtained with knee braces to an improvement in self-reported pain symptoms of 54% of respondents after using a knee brace. Thirty percent of the respondents reported that their pain symptoms changed significantly to very significantly. Briggs et al. have also shown that it is thought that the reduced pain experienced contributes to increased confidence in the knee and consequently improves the patient’s ability to maintain their general health (7).
Course of mobility limitations over time
The mobility level of patients in the mobility range greater than 50 m was high, with, on average, 85% of respondents indicating a high level of mobility when using the knee brace. When comparing new users (88%) with repeat users (84%), no significant difference was found. These results support the findings of Van Dijk et al. and Pisters et al., who showed that limitations in activities were fairly stable during the first 3 years of follow-up (24, 25).
However, the self-reported limitation in mobility when not using a knee brace was reported to be higher for the repeat users in the current study; Only 24% of new users reported a highly limited mobility level (only being able to move within their living environment), compared with 39% of repeat users. Self-reported mobility gain for patients with a knee brace who were in the mobility range greater than 50 m was shown to improve in 26% of new users and 53% of repeat users. These results support the findings of Holla et al. (26), showing that activity limitations decreased slightly after 2 years of follow-up.
Study limitations
Perception-based methods assess pain, function, and quality of life, which are the qualitative markers of disease progression. The quality of these methods depends on the disease condition, mood, physical activities, and ultimately the score provided by patients. Although these methods are well accepted by clinicians, it is not possible to use them to quantify morphological and biomechanical changes in the soft tissue regions. Therefore, one should be cautious about making assumptions regarding the predictive value of long- and short-term effects based on the overall physical activity of the subject.
Many patients compensate for knee instability by increasing muscle activation (co-contraction) around their knee joint. This provides a stable feeling, but also has a progressive effect on knee OA due to the increased pressure on the knee joint. Wearing a stabilizing rigid knee brace ensures a reduction in muscle co-contraction and pain (27). With a reported pain reduction of 54%, it is possible that users wearing knee braces in this study used less co-contraction, which might indicate reduced progression of knee OA. Further research is needed to confirm this finding.
The use of pain medications was not assessed in this study, and the use of analgesics could have influenced the results. Although it is expected that only a few patients use pain medication when using knee braces, further research should include this information to investigate the overall reduction in pain. In addition, 9% of patients did not experience any improvements when using a knee brace, or even experienced deterioration. While several factors, such as correct knee brace fitting, over-compensation of muscles, or additional injuries, could play a role in this, further research is required to understand these outcomes.
CONCLUSION
This large-scale PROM study of the effectiveness of use of semi-rigid knee braces in patients with knee OA shows that use of a brace contributes to general daily functioning, reduces pain, and increases the possibility to perform daily activities. For patients with OA, reduced pain enables increased mobility away from the home environment, resulting in a more active life and increased quality of life. Use of a knee brace appears to provide suitable joint support, offering pain relief and freedom of mobility.
REFERENCES
- Gohal C, Shanmugaraj A, Tate P, Horner NS, Bedi A, Adili A, et al. Effectiveness of valgus offloading knee braces in the treatment of medial compartment knee osteoarthritis: a systematic review. Sports Health: A Multidisciplinary Approach 2018; 10: 500–514.
- Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: Its prevalence and relationship to physical function. Arthrit Care Res 2004; 51: 941–946.
- Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil 2013; 21: 1145–1153.
- McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil 2014; 22: 363–388.
- Jeong HS, Lee SC, Jee H, Song JB, Chang HS, Lee SY. Proprioceptive training and outcomes of patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. J Athlet Train 2019; 54: 418–428.
- Richtlijnendatabase Federatie Medisch Specialisten. Conservatieve behandeling van artrose in heup of knie. [cited 2022 Mar 1]. Available from: https://richtlijnendatabase.nl/richtlijn/artrose_in_heup_of_knie/behandeling_heup-_of_knieartrose/kniebraces_en_voetortheses.html
- Briggs K, Matheny L, Steadman J. Improvement in quality of life with use of an unloader knee brace in active patients with OA: a prospective cohort study. J Knee Surg 2012; 25: 417–422.
- Thoumie P, Marty M, Avouac B, Pallez A, Vaumousse A, Pipet LPT, et al. Effect of unloading brace treatment on pain and function in patients with symptomatic knee osteoarthritis: the ROTOR randomized clinical trial. Sci Rep 2018; 8: 10519.
- Duivenvoorden T, Brouwer RW, van Raaij TM, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2015.
- Ostrander R v, Leddon CE, Hackel JG, O’Grady CP, Roth CA. Efficacy of unloader bracing in reducing symptoms of knee osteoarthritis. Am J Orthop (Belle Mead NJ) 2016; 45: 306–311.
- Richard Steadman J, Briggs KK, Pomeroy SM, Wijdicks CA. Current state of unloading braces for knee osteoarthritis. Knee Surgery, Sports Traumatology, Arthroscopy 2016; 24: 42–50.
- Smith AJ, Lloyd DG, Wood DJ. Pre-surgery knee joint loading patterns during walking predict the presence and severity of anterior knee pain after total knee arthroplasty. J Orthopaed Res 2004; 22: 260–266.
- Weldring T, Smith SMS. Article commentary: patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Services Insights 2013; 6: HSI.S11093.
- Zorginstuut Nederland. PROM-toolbox: PROM-wijzer en PROM-cyclus. 2021 [cited 2022 Apr 9]. Available from: https://www.zorginzicht.nl/ondersteuning/prom-toolbox-prom-wijzer-en-prom-cyclus
- Zorginzicht. PROM toolbox (summary in English). 2021 [cited 2022 Mar 15]. Available from: https://www.zorginzicht.nl/ondersteuning/prom-toolbox-summary-in-english
- Terwee CB, van der Wees PJ, Beurskens S. Handreiking voor de selectie van PROs en PROMs. [Guidelines for the selection of PROs and PROMs.] [Internet]. NFU-consortium Kwaliteit van Zorg [Dutch Federation of University Medical Centers-Syndicate Quality of Health]; 2015 [cited 2022 Mar 1]. (Guideline). Available from: https://nfukwaliteit.nl/pdf/1502.03_Handreiking_selectie_PROs_en_PROMs_definitief.pdf
- Parween R, Shriram D, Mohan RE, Lee YHD, Subburaj K. Methods for evaluating effects of unloader knee braces on joint health: a review. Biomed Eng Lett 2019; 9: 153–168.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research. Acad Med 2014; 89: 1245–1251.
- Nivel Zorgregistraties. Artrose – Prevalentie en aantal nieuwe gevallen van artrose – huisartsenpraktijk. [cited 2022 Mar 1]. Available from: https://www.vzinfo.nl/artrose/leeftijd-en-geslacht
- Nagai K, Yang S, Fu FH, Anderst W. Unloader knee brace increases medial compartment joint space during gait in knee osteoarthritis patients. Knee Surg Sports Traumatol Arthrosc 2019; 27: 2354–2360.
- Petersen W, Ellermann A, Zantop T, Rembitzki IV, Semsch H, Liebau C, et al. Biomechanical effect of unloader braces for medial osteoarthritis of the knee: a systematic review (CRD 42015026136). Arch Orthopaed Trauma Surg 2016; 136: 649–656.
- Petersen W, Ellermann A, Henning J, Nehrer S, Rembitzki IV, Fritz J, et al. Non-operative treatment of unicompartmental osteoarthritis of the knee: a prospective randomized trial with two different braces – ankle–foot orthosis versus knee unloader brace. Arch Orthopaed Trauma Surg 2019; 139: 155–166.
- Kiel J, Kaiser K. Patellofemoral arthritis. [Updated 2021 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513242/?report=classic
- van Dijk GM, Veenhof C, Spreeuwenberg P, Coene N, Burger BJ, van Schaardenburg D, et al. Prognosis of limitations in activities in osteoarthritis of the hip or knee: a 3-year cohort study. Arch Phys Med Rehabil 2010; 91: 58–66.
- Pisters MF, Veenhof C, van Dijk GM, Heymans MW, Twisk JWR, Dekker J. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: risk factors for future functional decline. Osteoarthr Cartil 2012; 20: 503–510.
- Holla JFM, Steultjens MPM, Roorda LD, Heymans MW, ten Wolde S, Dekker J. Prognostic factors for the two-year course of activity limitations in early osteoarthritis of the hip and/or knee. Arthrit Care Res 2010; 62: 1415–1425.
- Fantini Pagani CH, Willwacher S, Kleis B, Brüggemann GP. Influence of a valgus knee brace on muscle activation and co-contraction in patients with medial knee osteoarthritis. J Electromyogr Kinesiol 2013; 23: 490–500.