ORIGINAL REPORT
A BIONIC HAND VS. A REPLANTED HAND
Ulrika WIJK, PhD1, Anders BJÖRKMAN, Prof2, Ingela K CARLSSON, Assoc Prof1, Freyja KRISTJANSDOTTIR, MSc1, Ante MRKONJIC, PhD1, Birgitta ROSÉN, Assoc Prof1 and Christian ANTFOLK, Assoc Prof3
From the 1Department of Translational Medicine – Hand Surgery, Lund University, Skåne University Hospital, Malmö, Sweden, 2Department of Hand Surgery, Institute of Clinical Sciences, Sahlgrenska University Hospital, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 3Deptartment of Biomedical Engineering, Faculty of Engineering, Lund University, Lund, Sweden
Objective: Evaluation of the hand function affected when replacing a malfunctioning hand by a bionic hand.
Design: Case report.
Subjects: One individual that wished for a better quality of life after unsatisfying hand function following a replantation.
Methods: A quantitative and qualitative evaluation of body functions as well as activity performance and participation before and after a planned amputation and prosthetic fitting is presented.
Results: Improvements were seen in the patient-reported outcome measures (PROMs) that were used regarding activity (Disability of the Arm, Shoulder and Hand [DASH] and Canadian Occupational Performance Measure [COPM]), pain (Neuropathic Pain Symptom Inventory [NPSI], Brief Pain Inventory [BPI], Visual Analogue Scale [VAS]), cold intolerance (CISS) and health related quality of life (SF-36), as well as in the standardised grip function test, Southampton Hand Assessment Procedure (SHAP). No referred sensations were seen but the discriminative touch on the forearm was improved. In the qualitative interview, a relief of pain, a lack of cold intolerance, improved appearance, better grip function and overall emotional wellbeing were expressed.
Conclusions: The planned amputation and subsequent fitting and usage of a hand prosthesis were satisfying for the individual with positive effects on activity and participation.
Clinical relevance: When the hand function after a hand replantation does not reach satisfactory levels, a planned amputation and a prosthetic hand can be the right solution.
LAY ABSTRACT
Here we present a case report of 1 individual who wished for a better quality of life after over 20 years’ experience of unsatisfying hand function following a replantation. Evaluation of body functions as well as activity performance and participation before and after a planned amputation and prosthetic fitting is presented. Improvements were seen in the patient-reported outcome measures regarding activity, pain, cold intolerance, and health-related quality of life, as well as in grip function test. In the interview, a relief of pain, a lack of cold intolerance, improved appearance, better grip function and overall emotional wellbeing were expressed. The planned amputation and the subsequent fitting and usage of a hand prosthesis were satisfying for the individual with positive effects on activity and participation. When the hand function after a hand replantation is not satisfactory, planned amputation and prosthetic hand can be considered.
Key words: arm amputation; bionic limb; hand prosthesis; hand rehabilitation; hand replantation.
Citation: JRM-CC 2024; 7: jrmcc24854. DOI: https://doi.org/10.2340/jrmcc.v7.24854
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Submitted: Nov 11, 2023; Accepted: Dec 14, 2023; Published: Jan 18, 2024
Correspondence address: Ulrika Wijk, Department of Translational Medicine – Hand Surgery, Lund University, Skåne University Hospital, Malmö, Sweden. E-mail: ulrika.wijk@med.lu.se
Competing interests and funding: The authors have no conflicts of interest to declare.
After a substantial trauma to the hand, replantation is, if possible, preferable to amputation (1, 2). The goal is to achieve satisfying hand function, but also a satisfying appearance. Satisfying sensory and grip function is desirable, but full recovery is not to be expected (1), and the quality of life might be affected (3).
Reported survival rate of replanted hands is about 50% (2), but this is not necessarily equal to a functional success or the subjective satisfaction. Factors that are reported to influence the results are level of injury, ischaemia time, age, and smoking history (4). In addition, a replanted hand has changed appearance, because of intrinsic muscle atrophies with subsequent weakness and motor imbalances. Poor discriminative sensibility adds to a limited grip function and such functional limitations can also be amplified by pain and cold sensitivity (1, 4).
Elective amputation of a hand and bionic reconstruction have been done with functional improvements and satisfying results in cases of sequelae after critical soft tissue injuries (5). In a few cases of brachial plexus injuries (6, 7), and in 1 case with arthrogryposis multiplex congenita with severe deficits of the hands, planned amputation and replacement with hand prosthesis with satisfying results have been described (8). However, even if an amputation is wished for, it is irreversible with potential pain problems, and a life-changing decision. After amputation, a prosthetic hand can, to some degree, compensate for the functional loss (9). In addition, a hand prosthesis plays a significant role regarding body image, identity, participation and for health-related quality of life (9, 10).
Here we present a case of an individual who desired better hand function after over 20 years with unsatisfying function following a hand replantation. The patient wanted to get rid of the non-appealing hand and asked for an amputation and a prosthesis to enable better grip function, less pain and to get relief from cold intolerance. A trans-radial amputation was done and he was fitted with a myoelectric hand prosthesis. The objective was an evaluation of the hand function affected when replacing a malfunctioning hand by a bionic hand.
Research questions: How was the grip function affected when the malfunctioning hand was replaced by a bionic hand? How did touch thresholds, tactile gnosis and cold intolerance change in the residual arm? How was the perceived activities of daily living (ADL) and participation affected by the amputation?
MATERIAL AND METHODS
Patient description
A 28-year-old right-handed man sustained a trans-radial amputation of the left, non-dominant hand as a result of a work-place accident. A replantation was done followed by traditional hand rehabilitation. At age 51, he contacted a hand clinic (not the same where the replantation was performed) because he experienced the replanted hand as a hindrance in ADL and also aesthetically unappealing. He worked full-time as a courier driver. The patient specifically asked if his replanted left hand (Fig. 1) could be amputated and replaced by a hand prosthesis.

Fig. 1. The hands with markings on the left arm at the level of the planned amputation.
Presurgical procedure
Before the decision on surgery, the patient underwent assessments of hand function, and a psychosocial evaluation was done to assess whether there were psychological or emotional hesitations to an amputation. To determine the patient’s ability to control the planned myoelectric prosthetic hand, the muscle function proximal to the planned amputation was assessed with surface EMG (electromyography) electrodes (extensors and flexors). A myoelectric prosthetic hand built on an orthosis with an OttoBock Sensor Speed hand, was used at home for 6 months prior to the amputation (Fig. 2), as described by Aszmann (5, 6). This gave the patient the opportunity to get familiar with how to control the prosthesis and was also a strategy to give reasonable expectations regarding grip ability.
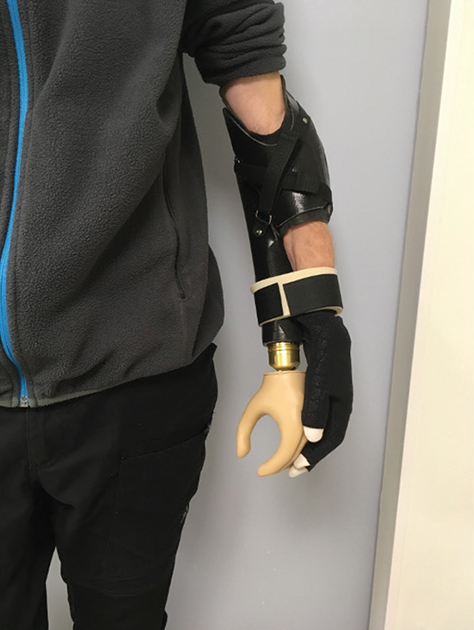
Fig. 2. The hybrid myoelectric prosthesis with a SensorSpeed hand (OttoBock) applied to the arm in the process before the amputation. This solution gave the patient the opportunity to get an idea of what he could expect from a hand prosthesis.
Assessments and patient-reported outcome measures
Body functions. Touch thresholds were assessed bilaterally with Semmes Weinstein monofilaments (SWM) (11) and tactile discrimination (2PD) (11). To assess the development of referred sensations, touch thresholds and tactile discrimination (on predefined points) were also tested on the forearm bilaterally, proximal to the level of injury and the planned level of amputation.
Grip strength was assessed with a Jamar dynamometer (Sammons Preston, Rolyon, Bolingbrook, IL, USA) (11) and pinch strength with a Pinch gauge dynamometer (B&L Engineering, CA, USA).
Function of intrinsic muscles was evaluated using Manual Muscle Strength Testing (MMST) (11).
Pain at rest was estimated on a Visual Analogue Scale (VAS) and 2 questionnaires were used: Brief Pain Inventory (BPI) Short Form (12) and the Neuropathic Pain Symptom Inventory (NPSI) (13).
For problems of cold intolerance, the self-administered questionnaire, CISS (Cold Intolerance Severity Score) was used (14).
The Southampton Hand Assessment Procedure (SHAP) (15, 16) and MiniSollerman (17) test were used for the assessment of grip function.
Body ownership was assessed with a Proprioceptive Pointing task (18). A ruler was placed on a screen, where the arm was hidden. The patient (blinded) was asked to mark on the ruler where the index finger on the replanted hand was experienced. A follow up 1 and 2 years after amputation, the test was made with and without the prosthetic hand, and the patient was asked to mark the location of the end of the residual arm, the experienced phantom index finger and the prosthetic index finger.
Activity. The Disability of the Arm, Shoulder and Hand (DASH) questionnaire (19), and the Canadian Occupational Performance Measure (COPM) (20) were used.
Health-related quality of life. For health-related quality of life, the patient completed the SF-36 (21) questionnaire.
Semi-structured interview. Before the elective amputation, the first author carried out a semi-structured interview (22), with focus on experiences regarding the hand. One year after the amputation, the patient was interviewed again with questions concerning experiences with the amputation and the prosthetic hand.
Surgical procedure
The amputation was performed under general anaesthesia and an axillary block by 2 specialists in hand surgery. The amputation was planned 17 cm distal to the radial epicondyle. The skin was incised creating a volar and a dorsal flap (fish-mouth). The muscles were transected, and the radius and ulna were divided with a power saw. The radial artery was ligated. The superficial branch of the radial nerve was divided 2 cm proximal of the osteotomy, and embedded in the musculature. The median nerve was macroscopically normal and divided approximately 4 cm proximal of the osteotomy and embedded in the musculature. The ulnar nerve was attached to the skin and had formed a large neuroma; the nerve was transected 4–5 cm proximal of the osteotomy and embedded in the musculature. The flexor and extensor muscles were secured with osteosutures on to the radius.
Prosthetic fitting
After healing of the skin, the prosthetic fitting process began with liner for compression and shaping the stump. After 3 months, the patient was equipped with a myoelectric hand prosthesis (Sensor Speed hand, Otto Bock). Five months post-surgery, the patient was equipped with a more advanced multiarticulated myoelectric prosthesis (BeBionic, Otto Bock) (Fig. 3).

Fig. 3. The patient fitted with the BeBionic hand prosthesis 6 months after amputation.
Follow ups
Assessments and patient-reported outcome measures (PROMs) were made prior to the elective amputation, and after 6, 12 and 24 months (Tables I and II).
| PRE | 6 months | 12 months | 24 months | |
| NPSI (Total) (0–1) | 0.27 | 0.23 | 0.19 | 0.08 |
| BPI-SF (median) (0–10) | 3 | 1 | 0 | 3,5* |
| Pain in rest (VAS) (0–10) | 4 | 5 | 2 | 1 |
| CISS (4–100) | 76 | 4 | 4 | 4 |
| SHAP (LIF score) (0–100) | 22.49 | 38.10 | 30.74 | - Pt declined |
| COPM (performance/satisfaction) (1–10) | 3.8/4 | 8.5/8.5 | 8.5/8.5 | 7/7.2 |
| DASH (0–100) | 46 | 21 | 15 | 13 |
| BPI: Brief Pain Inventory; CISS: Cold Intolerance Severity Score; COPM: Canadian Occupational Performance Measure; DASH: Disability of the Arm, Shoulder and Hand; NPSI: Neuropathic Pain Symptom Inventory; SHAP: Southampton Hand Assessment Procedure; VAS: Visual Analogue Scale. | ||||
| There are improvements in all assessments. In NPSI, BPI, VAS, CISS and DASH, a lower score indicates improvements and in SHAP and COPM, a higher score is better. IN SHAP normal hand function is regarded as equal or above 100 points, and in COPM maximum score is 10. | ||||
| *At 24 month follow up, the patient reported low back pain that affected the score in BPI. | ||||
| SF-36 (0–100) | Pre | 6 months | 12 months | 24 months |
| Physical functioning | 70 | 80 | 75 | 80 |
| Role limitations due to physical health | 0 | 0 | 50 | 75 |
| Role limitation due to emotional problems | 100 | 0 | 100 | 100 |
| Energy/fatigue | 30 | 80 | 60 | 50 |
| Emotional well-being | 64 | 92 | 85 | 80 |
| Social functioning | 75 | 100 | 87.5 | 87.5 |
| Pain | 55 | 80 | 90 | 57.5* |
| General health | 75 | 80 | 60 | 80 |
| Higher scores indicate better well-being. | ||||
| *At 24 month follow up, the patient reported low back pain that affected the score. | ||||
RESULTS
Pre-intervention assessments showed that touch thresholds were close to normal (11). Slightly increased touch thresholds (SWM 3.61) compared to normal touch thersholds in ulnar nerve innervated skin. In median nerve innervated areas the touch threshold was considered normal (SWM 2.83). Discriminative touch was poor (not measurable) with 2PD>15 mm at the index as well as the little finger. From preoperatively to 2 years follow up 2PD on the left forearm decreased from 40 mm to 15 mm, as compared to 50 mm to 30 mm on the right side. Touch thresholds were normal at the left forearm after 1 year and slightly increased after 2 years.
Preoperatively grip force was not measurable, and Manual Muscle Strength Test scored 0 as did the MiniSollerman test.
Pain decreased as showed in NPSI, BPI and VAS (see Table II). Cold intolerance was a large inconvenience with the replanted hand, and symptoms that were highly rated were pain, stiffness, reduced grip strength and ache (NRS range 1–8). A total relief of symptoms on cold exposure was seen after the amputation as well as the subsequent problems in daily life as seen in the total CISS score (Table I).
Body ownership test showed a telescoping phenomenon, meaning that the experienced phantom hand come closer to the residual arm. At the 1 year follow up, the phantom index finger was marked 27 cm distally from the olecranon compared to 16 cm at the 2 years follow up. The residual arm end was estimated to the correct length, and so was the index finger of the prosthetic hand. At the 2 years follow up, the arm length was estimated to 0.5 cm more distally than in reality and the index finger of the prosthetic hand 7 cm proximal of the actual length.
DASH-score improved with a steady improvement during the follow up period well exceeding the MCID of 11–15 (23), see Table I. COPM showed an improvement both regarding performance and satisfaction of the selected activities. SHAP showed improved grip function at 6 month and 12 months (Table I). At 2 years follow up, the patient declined to do the SHAP due to a lack of time.
The health-related quality of life assessed with SF-36 improved after the amputation, with the highest score at 2 years follow up (Table II).
In the interview, the individual expressed that the main reasons for wanting an amputation was pain, cold intolerance, weak grip function and the unappealing appearance of the hand. At one-year follow up, the satisfaction of the amputation and the bionic reconstruction was highly expressed. Pain relief, no cold intolerance, a stronger grip with the myoelectric hand prosthesis and satisfaction with the new appearance were expressed, both with and without the prosthetic hand. The quantitative assessments agreed well with the information from the interview (Table III).
DISCUSSION
The success rate after replantation is often reported in replant survival, but this is not the only adequate measure of success. In this case reported, the hand had survived but function and appearance were unsatisfying. The planned amputation more than 20 years after the replantation and the subsequent fitting and usage of a myoelectric hand prosthesis had highly positive effects on activity, participation and health-related quality of life.
The first choice when a hand is amputated is, if possible, always replantation. The delicate hand function and sensibility are impossible to fully replace with hand prostheses today, and a “bad hand” may be more functional than an amputation (24). A review (25) describes advantages of replantation, regarding functional results, satisfaction rate and quality of life, in comparison to prostheses. However, a replantation of a hand does not always reach the desired functional results. The level of injury, ischaemia time, age, smoking history, etc., influence the results (4). In addition, atrophies, and motor imbalances change the appearance of the hand. The benefits from replantation also depend on the individual coping abilities and possibility to return to daily living, work, and leisure activities (1, 26). The individual in this case described the grip function, as “non-existent.”
A hope for better grip function can be wished for, and sometimes there is too high expectations on what a prosthetic hand can provide. A hand prosthesis with limited mobility and no sensory feedback can never replace a well-functioning human hand (27, 28), and with this in mind, the very satisfying results in the case here presented are focused on improved activity and participation. Grip function in a prosthetic hand has its limits, even though it, in this case, was an advanced Bebionic hand (OttoBock). Nevertheless, hand prosthesis offered better grip function than a poorly functioning hand (5, 6, 8).
A good sensory function is vital for a useful grip function. After replantation, a substantial limited and misdirected axonal regeneration and reinnervation result in changes in afferent and efferent nerve signalling and thus adaptations in the primary somatosensory cortex and motor network in the brain. This was illustrated in the present case with close to normal touch thresholds in the replanted hand while discriminative touch was poor. This might be a result of the considerable cortical reorganisation that is a challenge for an adult person to handle in the sensory relearning (29).
Referred sensation, often following amputation, was not seen in the reported case after the planned amputation. Referred sensation is a common phantom phenomenon (30), but the cause is not fully understood, even if theories explain it by cortical reorganisation, and the neurones in the sensory cortex that were responsible for the hand prior to the amputation starts to respond to the forearm skin (31, 32). However, despite the lack of referred sensation, the discriminative touch on the forearm stump was improved. This is in line with previous results (31) and may be that the cortical area of the forearm expanded and engaged the prior hand area, and the sensibility improved.
Pain was described both before and after the amputation. With the replanted hand, the individual described the pain like tingling, stabbing, pressing or like a shooting pain inside the hand. He also experienced pain when the hand bumped against something. The NPSI questionnaire revealed diminishing pain levels at each follow-up. So did the BPI, except at the 2 years follow up, due to back pain. In the interview, the pain after the amputation is explained as something you can live with, and is not described as detailed as prior. Pain relief has previously been reported as a gain in elective arm amputations after critical soft tissue injuries (5), and in cases with brachial plexus injuries (6).
Another limiting factor that highly improved was cold intolerance. He liked outdoor activities which he could do only under limited time or not at all, depending on the pain that came with cold exposure or windy weather. Cold intolerance is common after hand injuries and almost all adults with replantation suffer from cold intolerance (33, 34). Cold intolerance affects engagement in meaningful activities, in all areas of life, (35), as for the individual in our report. After the amputation, the cold intolerance disappeared completely, which was expressed in the interview as well as shown in CISS. This, in combination with a grip function, made it possible for the patient to resume old hobbies, like kayaking and hunting, that he had not practised for over 20 years.
The appearance of the replanted hand was a very disturbing factor. He was ashamed and hid the hand in a glove or sleeve. The appearance plays a role for the self-confidence, which also affects societal participation (10, 33). Hands are important in activities of daily life, and have a significant role in gestures, body language and communication (28), and for our perceived body image and identity (36). The value of an appealing appearance in a bionic hand in addition to some grip function is emphasised in the results in this case (37). Appearance is a part of a conscious experience of ourselves and is crucial to feel body ownership, the experience of the body being one’s own (38). Even if the advanced myoelectric hand prosthesis did not have any sensory feedback system incorporated, the individual in our report expressed the experience of the prosthetic hand more as a part of the body than his own poorly functioning hand. In the proprioceptive pointing task, at the 2 years follow up the arm length was estimated closer to the actual armlength, which may indicate an improved body ownership of the prosthesis over time.
Emotional struggles were experienced preoperatively, and after the amputation a sense of relief was expressed. The individual expressed that he never had any doubts or regrets. This is also shown in the improved scores in SF-36 regarding health-related quality of life. Adjustment to prosthesis and activity restrictions has been used as a measure of emotional wellbeing, and a relationship between depression and anxiety has been reported to prosthetic adjustment and activity restrictions by extension (39). Emotional wellbeing is affected by body image anxiety, social discomfort and depression among amputees; but the individual in this case expressed an improved body image after the amputation, improved ability to perform daily activities, and was well adjusted to the prosthesis. An unsatisfactory appearance and body image can impact both emotional wellbeing and social participation in a negative way (40), and the effect is the opposite when the appearance is satisfactory.
Clinical take home message
Patients can experience unsatisfactory result following hand replantation or following major injuries in the arm rendering the hand more or less incapable of use. In such cases, the patient can wish for an amputation of the hand and subsequent fitting with a hand prosthesis, and sometimes the wish can be built on false hopes. When an elective amputation is considered, it is of high importance to provide reasonable expectations of the outcome regarding function, grip ability, aesthetics and the risk of pain. In this case, we let the individual use a hybrid prosthetic hand before deciding on amputation, which gave an experience both regarding controlling the prosthetic hand and the grip ability. Also, appearance, body image and body ownership and how these factors influence wellbeing and social participation, should be considered in the decision-making process and in rehabilitation.
When the hand function is poor and the hand is seen as useless, especially in combination with poor sensibility, an elective amputation may be a viable option. However, it is important to keep in mind that a prosthetic hand can add functions but it can never replace a non-injured hand.
ACKNOWLEDGEMENTS
This work was supported by the Promobilia Foundation, Stiftelsen för bistånd åt rörelsehindrade i Skåne and the Swedish Research Council (DNR 2019–05601) and The County Council of Skåne and Vårdakademin at Skåne University Hospital.
Ethics: The studies involving human participants were reviewed and approved by the Swedish Ethical Review Authority in Sweden. The patient provided written informed consent to participate in this study. Ethical approval Dnr 2020-06311.
REFERENCES
- Rosberg HE. Disability and health after replantation or revascularisation in the upper extremity in a population in southern Sweden – a retrospective long time follow up. BMC Musculoskel Disord 2014; 15: 73. https://doi.org/10.1186/1471-2474-15-73
- Billington AR, Ogden BW, Le NK, King KS, Rotatori RM, Kim RL, et al. A 17-year experience in hand and digit replantation at an academic center. Plast Reconstr Surg 2021; 148: 816–824. https://doi.org/10.1097/PRS.0000000000008314
- Syrko M, Jabłecki J. Quality of life-oriented evaluation of late functional results of hand replantation. Ortop Traumatol Rehabil 2010; 12: 19–27.
- Beris AE, Lykissas MG, Korompilias AV, Mitsionis GI, Vekris MD, Kostas-Agnantis IP. Digit and hand replantation. Arch Orthop Trauma Surg 2010; 130: 1141–1147. https://doi.org/10.1007/s00402-009-1021-7
- Aszmann OC, Vujaklija I, Roche AD, Salminger S, Herceg M, Sturma A, et al. Elective amputation and bionic substitution restore functional hand use after critical soft tissue injuries. Sci Rep 2016; 6: 34960. https://doi.org/10.1038/srep34960
- Aszmann OC, Roche AD, Salminger S, Paternostro-Sluga T, Herceg M, Sturma A, et al. Bionic reconstruction to restore hand function after brachial plexus injury: a case series of three patients. Lancet 2015; 385: 2183–2189. https://doi.org/10.1016/S0140-6736(14)61776-1
- Hruby LA, Gstoettner C, Sturma A, Salminger S, Mayer JA, Aszmann OC. Bionic upper limb reconstruction: a valuable alternative in global brachial plexus avulsion injuries – a case series. J Clin Med 2019; 9(1): 23. https://doi.org/10.3390/jcm9010023
- Salminger S, Roche AD, Sturma A, Hruby LA, Aszmann OC. Improving arm function by prosthetic limb replacement in a patient with severe arthrogryposis multiplex congenita. J Rehabil Med 2016; 48: 725–728. https://doi.org/10.2340/16501977-2123
- Murray C. Amputation, prosthesis use, and phantom limb pain. An interdisciplinary perspective. New York, NY: Springer; 2010.
- Kristjansdottir F, Dahlin LB, Rosberg HE, Carlsson IK. Social participation in persons with upper limb amputation receiving an esthetic prosthesis. J Hand Ther 2020; 33: 520–527. https://doi.org/10.1016/j.jht.2019.03.010
- ASHT. American Society of Hand Therapists Clinical Assessment Recommendations. 3rd Ed. Mount Laurel, NJ: American Society of Hand Therapist: 2015
- Jumbo SU, MacDermid JC, Kalu ME, Packham TL, Athwal GS, Faber KJ. Measurement properties of the Brief Pain Inventory-Short Form (BPI-SF) and Revised Short McGill Pain Questionnaire Version-2 (SF-MPQ-2) in pain-related musculoskeletal conditions: a systematic review. Clin J Pain 2021; 37: 454–474. https://doi.org/10.1097/AJP.0000000000000933
- Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, et al. Development and validation of the Neuropathic Pain Symptom Inventory. Pain 2004; 108: 248–257. https://doi.org/10.1016/j.pain.2003.12.024
- Carlsson I, Cederlund R, Höglund P, Lundborg G, Rosén B. Hand injuries and cold sensitivity: reliability and validityof cold sensitivity questionnaires. Disabil Rehabil 2008; 30: 1920–1928. https://doi.org/10.1080/09638280701679705
- Burgerhof JG, Vasluian E, Dijkstra PU, Bongers RM, van der Sluis CK. The Southampton Hand Assessment Procedure revisited: A transparent linear scoring system, applied to data of experienced prosthetic users. J Hand Ther 2017; 30: 49–57. https://doi.org/10.1016/j.jht.2016.05.001
- Resnik L, Borgia M, Cancio JM, Delikat J, Ni P. Psychometric evaluation of the Southampton hand assessment procedure (SHAP) in a sample of upper limb prosthesis users. J Hand Ther 2023; 36(1): 110–120. https://doi.org/10.1016/j.jht.2021.07.003
- Rosén B, Lundborg G. A new model instrument for outcome after nerve repair. Hand Clin 2003; 19: 463–470. https://doi.org/10.1016/S0749-0712(03)00003-9
- Wijk U, Carlsson IK, Antfolk C, Björkman A, Rosén B. Sensory feedback in hand prostheses: a prospective study of everyday use. Front Neurosci 2020; 14: 663. https://doi.org/10.3389/fnins.2020.00663
- Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand 2000; 71: 613–618. https://doi.org/10.1080/000164700317362262
- Wressle E, Marcusson J, Henriksson C. Clinical utility of the Canadian Occupational Performance Measure – Swedish version. Can J Occup Ther 2002; 69: 40–48. https://doi.org/10.1177/000841740206900104
- Sullivan M, Karlsson J, Ware JE, Jr. The Swedish SF-36 Health Survey – I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995; 41: 1349–1358. https://doi.org/10.1016/0277-9536(95)00125-Q
- Moser A, Korstjens I. Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur J Gen Pract 2018; 24: 9–18. https://doi.org/10.1080/13814788.2017.1375091
- Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther 2014; 44: 30–39. https://doi.org/10.2519/jospt.2014.4893
- Tintle SM, Baechler MF, Nanos GP, 3rd, Forsberg JA, Potter BK. Traumatic and trauma-related amputations: Part II: Upper extremity and future directions. J Bone Joint Surg Am 2010; 92(18): 2934–2945. https://doi.org/10.2106/JBJS.J.00258
- Otto IA, Kon M, Schuurman AH, van Minnen LP. Replantation versus prosthetic fitting in traumatic arm amputations: a systematic review. PLoS One 2015; 10: e0137729. https://doi.org/10.1371/journal.pone.0137729
- Sherman R. To reconstruct or not to reconstruct? N Engl J Med 2002; 347: 1906–1907. https://doi.org/10.1056/NEJMp020150
- Wijk U, Carlsson I. Forearm amputees’ views of prosthesis use and sensory feedback. J Hand Ther 2015; 28: 269–277. https://doi.org/10.1016/j.jht.2015.01.013
- Lundborg G. Tomorrow’s artificial hand. Scand J Plast Reconstruct Surg Hand Surg 2000; 34: 97–100. https://doi.org/10.1080/02844310050159927
- Björkman A, Waites A, Rosén B, Lundborg G, Larsson EM. Cortical sensory and motor response in a patient whose hand has been replanted: one-year follow up with functional magnetic resonance imaging. Scand J Plast Reconstruct Surg Hand Surg 2007; 41: 70–76. https://doi.org/10.1080/02844310601140956
- Ehrsson HH, Rosen B, Stockselius A, Ragnö C, Kohler P, Lundborg G. Upper limb amputees can be induced to experience a rubber hand as their own. Brain 2008; 131: 3443–3452. https://doi.org/10.1093/brain/awn297
- Björkman A, Wijk U, Antfolk C, Bjorkman-Burtscher I, Rosen B. Sensory qualities of the phantom hand map in the residual forearm of amputees. J Rehabil Med 2016; 48: 365–370. https://doi.org/10.2340/16501977-2074
- Björkman A, Weibull A, Olsrud J, Ehrsson HH, Rosen B, Bjorkman-Burtscher IM. Phantom digit somatotopy: a functional magnetic resonance imaging study in forearm amputees. Euro J Neurosci 2012; 36: 2098–2106. https://doi.org/10.1111/j.1460-9568.2012.08099.x
- Rosberg H-E, Dahlin LD, Carlsson IK. A qualitative study of long-term censequences and adaptation in daily life after erplantation surgery at a young age. Hand Ther 2022; 27: 112–122.
- Vaksvik T, Hetland K, Røkkum M, Holm I. Cold hypersensitivity 6 to 10 years after replantation or revascularisation of fingers: consequences for work and leisure activities. J Hand Surg Euro 2009; 34: 12–17. https://doi.org/10.1177/1753193408094440
- Carlsson IK, Edberg AK, Wann-Hansson C. Hand-injured patients’ experiences of cold sensitivity and the consequences and adaptation for daily life: a qualitative study. J Hand Ther 2010; 23: 53–61. https://doi.org/10.1016/j.jht.2009.07.008
- Murray CD, Forshaw MJ. The experience of amputation and prosthesis use for adults: a metasynthesis. Disabil Rehabil 2013; 35: 1133–1142. https://doi.org/10.3109/09638288.2012.723790
- Sturma A, Hruby LA, Boesendorfer A, Pittermann A, Salminger S, Gstoettner C, et al. Prosthetic embodiment and body image changes in patients undergoing bionic reconstruction following brachial plexus injury. Front Neurorobot 2021; 15: 645261. https://doi.org/10.3389/fnbot.2021.645261
- Tsakiris M, Schutz-Bosbach S, Gallagher S. On agency and body-ownership: phenomenological and neurocognitive reflections. Conscious Cogn 2007; 16: 645–660. https://doi.org/10.1016/j.concog.2007.05.012
- Desteli EE, İmren Y, Erdoğan M, Sarısoy G, Coşgun S. Comparison of upper limb amputees and lower limb amputees: a psychosocial perspective. Eur J Trauma Emerg Surg 2014; 40: 735–739. https://doi.org/10.1007/s00068-014-0418-3
- Verma CV, Vora T, Thatte M, Yardi S. Patient perception after traumatic brachial plexus injury – a qualitative case report. J Hand Ther 2020; 33: 593–597. https://doi.org/10.1016/j.jht.2019.03.007