ORIGINAL REPORT
REHABILITATION OUTCOMES IN PATIENTS WITH LOWER LIMB AMPUTATION RECEIVING HAEMODIALYSIS: A RETROSPECTIVE COHORT STUDY
Yoshitaka WADA, MD, PhD, Yohei OTAKA, MD, PhD, Yuki SENJU, MD, PhD, Hiroshi HOSOKAWA, MD, Takamichi TOHYAMA, MD, PhD, Hirofumi MAEDA, MD, PhD, Masahiko MUKAINO, MD, PhD, Seiko SHIBATA, MD, PhD and Satoshi HIRANO, MD, PhD
From the Department of Rehabilitation Medicine I, School of Medicine, Fujita Health University, Japan
Objective: To compare the functional outcomes of patients with lower limb amputations receiving haemodialysis and those not receiving haemodialysis.
Design: A retrospective cohort study.
Patients: Patients with lower limb amputation who were admitted to a convalescent rehabilitation ward between January 2018 and December 2021.
Methods: The primary outcome was the effectiveness of the Functional Independence Measure (FIM) during hospitalisation in the ward. Secondary outcomes included the total and subtotal (motor/cognitive) FIM scores at discharge, gain in the total and subtotal (motor/cognitive) FIM scores, K-level at discharge, length of hospital stay in the ward, rehabilitation time, and discharge destination. Outcomes were compared between the non-haemodialysis and haemodialysis groups.
Results: A total of 28 patients (mean [standard deviation] age, 67.0 [11.9] years; men, 20) were enrolled in this study. Among them, 11 patients underwent haemodialysis. The FIM effectiveness was significantly higher in the non-haemodialysis group than in the haemodialysis group (median [interquartile range], 0.78 [0.72 – 0.81] vs 0.65 [0.28 – 0.75], p = 0.038). The amount of rehabilitation and all secondary outcomes were not significantly different between the groups (p > 0.05).
Conclusion: Patients with lower limb amputation who were receiving haemodialysis had poorer FIM effectiveness than those not receiving haemodialysis.
LAY ABSTRACT
Chronic kidney disease is a risk factor for foot ulcers and lower limb amputation. Thus, patients with lower limb amputation often require maintenance dialysis. However, there is a lack of knowledge on whether patients with lower limb amputation receiving haemodialysis can achieve functional outcomes comparable to those not receiving haemodialysis. This study aimed to compare functional outcomes between patients with lower limb amputations receiving haemodialysis and those not receiving haemodialysis. This retrospective cohort study enrolled 28 patients who underwent amputation surgery and were admitted to a rehabilitation ward, including 11 patients undergoing haemodialysis (8 with diabetic nephropathy, 1 with chronic glomerulonephritis, 1 with rapidly progressive glomerulonephritis, and 1 with acute kidney injury). Although the amount of rehabilitation did not differ between groups, the improvement in the activities of daily living was significantly better in the non-haemodialysis group than in the haemodialysis group. Thus, even the same amount of rehabilitation for patients with lower limb amputations receiving haemodialysis may not lead to functional outcomes comparable to those without haemodialysis.
Key words: activities of daily living; comorbidity; amputation; renal dialysis; rehabilitation; haemodialysis; lower limb amputation.
Citation: JRM-CC 2022; 5: jrmcc00088. DOI: http://dx.doi.org/10.2340/jrmcc.v5.2525
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Oct 3, 2022; Published: Nov 24, 2022
Correspondence address: Yohei Otaka, Department of Rehabilitation Medicine I, School of Medicine, Fujita Health University, 1-98 Dengakugakubo, Kutsukake, Toyoake, Aichi 470-1192, Japan, Tel: +81-562-93-2167, Fax: +81-562-95-2906. E-mail: otaka119@mac.com
Competing interests and funding: The authors have no conflicts of interest to declare.
This research received no specific grants from any funding agency in the public, commercial, or not-for-profit sectors.
The number of patients receiving haemodialysis is increasing globally (1). Patients with chronic kidney disease (CKD) are at high risk of foot ulceration (2). In particular, CKD stages 4–5 or haemodialysis has been reported to be an independent risk factor for foot ulceration and lower limb amputation compared to CKD stage 3 (3). The prevalence of lower limb amputation in patients undergoing haemodialysis ranges from 1.7 to 13.4% (4). Patients receiving haemodialysis are characterised by a high rate of muscle protein degradation accompanied by impaired protein synthesis (5) and may not be able to achieve sufficient muscle mass gain because of increased catabolism. The prevalence of sarcopenia is high in patients undergoing haemodialysis (6, 7). In addition, patients receiving haemodialysis should spend a large amount of time in bed, which could lead to inactivity and deprive them of the opportunity to receive rehabilitative interventions. The presence of haemodialysis may therefore affect the outcomes of rehabilitation.
There are few reports on rehabilitation outcomes in patients with lower limb amputation undergoing haemodialysis (8–11). A retrospective cohort study (11) revealed that the Functional Independence Measure (FIM) score (12, 13) was higher in the non-end-stage kidney disease (ESKD) group at discharge than in the ESKD group, whereas another retrospective cohort study (9) showed that the total FIM score at discharge and FIM gain were not significantly different between patients with lower limb amputation receiving haemodialysis and those who were not receiving haemodialysis. The mixed findings prevent the conclusion of how haemodialysis affects the functional outcomes of rehabilitation in patients with lower limb amputation. Furthermore, previous studies (8–11) have not clarified whether the amount of rehabilitation is equivalent in ESKD and non-ESKD groups, which may influence the outcomes.
The purpose of this study was to compare the functional outcomes of patients with lower limb amputations receiving haemodialysis and those not receiving haemodialysis. We hypothesised that haemodialysis patients might not respond to rehabilitation as well as non-haemodialysis patients and might not receive the same amount of rehabilitation as non-haemodialysis patients, and thus might not achieve the same functional outcomes as non-haemodialysis patients.
METHODS
Study design and patients
In this retrospective cohort study, consecutive patients with lower limb amputation who were admitted to a 60-bed convalescent inpatient rehabilitation ward in a university hospital between January 2018 and December 2021 were included. Patients who were not fitted with a prosthesis were also included. Patients who discontinued rehabilitation because of transfer to acute care wards or death during hospitalisation were excluded.
The convalescent inpatient rehabilitation ward was established in April 2000 in Japan and specialises in rehabilitation. In the case of lower limb amputation, patients can stay in the ward for up to 150 days after amputation, and they can undergo a maximum of 3 h of physical therapy and occupational therapy per day. The rehabilitation program was tailored to the specific needs of each patient, focusing on range-of-motion training, muscle strengthening training, gait training, and training for activities of daily living.
Ethics statements
This study was approved by the ethics committee of Fujita Health University (reference number: HM21303) and was conducted in accordance with the STROBE guidelines (14). The requirement for informed consent was waived because of the retrospective study design, and individuals who did not opt out were included.
Outcomes
The primary outcome was the FIM effectiveness (15) during hospitalisation in the ward. Secondary outcomes were the total FIM score, subtotal FIM motor items score, subtotal FIM cognitive items score, gain in the total and the subtotal (motor/cognitive) FIM scores (15), gait ability scored by the K-level (16) at discharge, length of stay (days) in the rehabilitation ward, amount of rehabilitation, average rehabilitation time per day, and discharge destination. As for FIM scores, each FIM item at admission and discharge was also investigated. These outcomes and patient characteristics, including age, sex, cause of amputation, amputation side, amputation level, Charlson Comorbidity Index (17), and number of days from amputation to admission to the ward were collected retrospectively from patients’ medical records.
The FIM is a rating scale for activities of daily living consisting of 13 motor items and 5 cognitive items (12, 13). The total FIM score ranges from 18 to 126, subtotal FIM motor items score ranges from 13 to 91, and subtotal FIM cognitive items score ranges from 5 to 35. A higher score indicates better activities of daily living. The validity and reliability of this scale have been confirmed (18). The FIM effectiveness was calculated as follows: (FIM score at discharge – FIM score on admission)/(126 – FIM score on admission) (15). The FIM gain is the total FIM score at discharge minus the total FIM score at admission (15). The FIM score was recorded on admission and at discharge by therapists who were well-trained in scoring with the FIM and in charge of the patients.
The K-level (19) is an index of gait ability in patients with lower limb amputation. K0 indicates inability to walk, K1 means able to walk only at home (very low activity), K2 indicated ability to walk outdoors with some limitations (low activity), K3 means able to walk outdoors without limitations (medium activity), and K4 indicates a high activity level such as an athlete (high activity). K-levels were determined by a physiatrist from the findings at the time of discharge.
The Charlson Comorbidity Index (17) scores comorbidities and evaluates 19 conditions related to chronic diseases. Its validity has been confirmed (17), and it has been used to evaluate comorbidities in ESKD (20).
The length of ward stay was defined as the number of days from admission to discharge from the rehabilitation ward. The timing of discharge was determined when the rehabilitation team judged that the patient had reached a plateau in activities of daily living.
The total rehabilitation time (h) was the total time of rehabilitation during hospitalisation in the convalescent rehabilitation ward.
Statistical analysis
Patients’ characteristics were compared between the haemodialysis and non-haemodialysis groups using the unpaired t-test, Mann–Whitney U test, or χ2 test depending on the type of variable. The primary outcome, the FIM effectiveness, was compared between the haemodialysis and non-haemodialysis groups using the Mann–Whitney U test. For comparisons of secondary outcomes between groups, the unpaired t-test, Mann–Whitney U test, or χ2 test was used depending on the type of variable. Furthermore, within-group comparisons between admission and discharge and between-group comparisons at admission and discharge for each FIM item were performed with the Wilcoxon signed-rank test and the Wilcoxon rank sum test, respectively. The effect size (ES) was calculated for each comparison of functional outcomes. The ES of the unpaired t-test was calculated using the Cohen D value from the mean and standard deviation (SD). The ES of the Mann–Whitney U test was calculated by dividing the Z-score by the square root of the total number of participants: ES=Z/sqrt (N). The ES of the χ2 test was calculated by dividing the χ2 value by the number of scores and taking the square root. Any p-values less than 0.05 were considered statistically significant. R (version 4.1.0 [2021-05-18], The R Project for Statistical Computing, Vienna, Austria) was used to perform all statistical analyses.
RESULTS
A total of 33 patients with lower limb amputation were admitted to the ward during the study period. Four patients were transferred to other acute care wards, and 1 patient died during hospitalisation in the ward. Therefore, 28 patients were included in the analysis (Fig. 1).
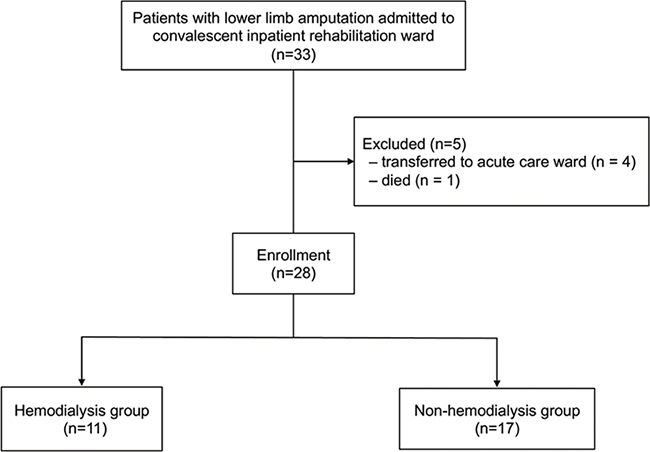
Fig. 1. Flow diagram of patient selection.
The participant characteristics are presented in Table I. The mean age of all patients was 67.0 (SD, 11.9; range 39–86) years (men, 20), and 11 of 28 patients were receiving haemodialysis. The causes of haemodialysis were as follows: diabetic nephropathy (n=8), chronic glomerulonephritis (n=1), rapidly progressive glomerulonephritis (n=1), and acute kidney injury because of hypovolemic shock (n=1). Of the 28 patients, 26 had prostheses. One patient from each of the haemodialysis and non-haemodialysis groups was not fitted with a prosthesis. Patient characteristics, except for the Charlson Comorbidity Index, were not significantly different between the groups (Table I). The total Charlson Comorbidity Index score was significantly higher in the haemodialysis group than in the non-haemodialysis group (median [interquartile range], 6 [4–7] vs 3 [1–6], p = 0.036). Among the subitems, “renal disease” was more prevalent in the haemodialysis group than in the non-haemodialysis group (11 [100%] vs 4 [23.5%], p = 0.002). One patient in the non-haemodialysis group had a history of stroke, but showed no obvious signs of paresis.
The FIM effectiveness was significantly higher in the non-haemodialysis group than in the haemodialysis group (median [interquartile range (IQR)], 0.78 [0.72 – 0.81] vs 0.65 [0.28 – 0.75], p=0.038, ES=0.55). As for the subtotal score, the FIM effectiveness for motor items was significantly higher in the non-haemodialysis group than in the haemodialysis group (median [IQR], 0.76 [0.68 – 0.80] vs 0.23 [0.70–0.76], p=0.020). The rest of the secondary outcomes were not significantly different between the groups (all, p>0.05) (Table II).
Regarding each FIM item score (Table III), the scores in transfer (bed, chair, wheelchair), transfer (tub, shower), walk/wheelchair, and stairs were significantly higher at discharge than on admission in both groups. In the non-haemodialysis group, grooming, upper body dressing, lower body dressing, and toileting were also significantly higher at discharge than on admission. Bathing, transfer (tub, shower), walk/wheelchair, comprehension, expression, and social interaction at discharge were significantly higher in the non-haemodialysis group than in the haemodialysis group, whereas there was no significant difference between groups on admission.
DISCUSSION
This study revealed that the FIM effectiveness of patients with lower limb amputations receiving haemodialysis was significantly poorer than those of patients not receiving haemodialysis in the study sample, although the amount of rehabilitation provided was not significantly different between the groups.
In a retrospective cohort study from the United States, the total FIM score and FIM gain did not show a significant difference on admission and at discharge between patients with lower limb amputation with ESKD on haemodialysis and those without ESKD (9). Another retrospective cohort study conducted in the United States revealed that patients with lower limb amputation on haemodialysis had a significantly longer hospital stay and a lower total FIM score at discharge than patients without ESKD (11). However, in the previous study (11), the FIM score at the time of admission was not described, and we could not confirm that there were no differences at baseline. In general, the amount of rehabilitation is related to functional outcomes (21, 22). However, these previous studies (9, 11) have not reported the amount of rehabilitation. Regarding the rehabilitation of patients receiving haemodialysis, exercise restrictions on the day of haemodialysis may become inhibiting factors, and we considered the possibility that sufficient rehabilitation was not provided. Therefore, we clarified the amount of rehabilitation in both groups, and it did not differ between the groups. Our findings revealed that even patients on haemodialysis underwent the same amount of rehabilitation as those without haemodialysis; however, this same amount of rehabilitation did not lead to the same functional outcomes between the groups. Unlike previous studies (9, 11), we did not use the total FIM score or FIM gain at discharge as the primary outcome. Patients with amputation cannot achieve the maximal score in several FIM items even when they can perform activities of daily living by themselves because of the use of functional aids such as prostheses. Furthermore, patients with lower limb amputation in this study had relatively high FIM scores. Therefore, we used FIM effectiveness as the primary outcome, which aimed to avoid ceiling effects. The FIM score at discharge and FIM gain are not sufficient to show a difference because of the high FIM score at admission in patients with lower limb amputation. In our study, all the indexes of FIM scores including the subtotal of cognitive/motor items at admission/discharge tended to be poorer in haemodialysis patients than in non-haemodialysis patients, and their ES range from 0.3 to 0.9, although not statistically significant. These findings indicate that patients with lower limb amputation on haemodialysis had poorer functional status throughout inpatient rehabilitation than those without haemodialysis, with poorer functional improvement.
This study showed each FIM item score in haemodialysis and non-haemodialysis groups, while previous studies (9, 11) showed only the total FIM score and did not show the score of each item. Motor items, which are main targets for the rehabilitation of patients with amputation, transfer, and mobility, were significantly improved from admission to discharge in both the groups. Furthermore, the scores for bathing, transfer (tub, shower), and walk/wheelchair at discharge were significantly higher in the non-haemodialysis group than in the haemodialysis group. It is of note that between-group differences were observed in both prosthetic-related items (walk/wheelchair) and non-prosthetic-related items such as bathing and transfer (tub, shower). This indicates that receiving haemodialysis might influence overall rehabilitation effectiveness.
There are 4 possible reasons for this. First, even with the same amount of rehabilitation, the haemodialysis group may have undergone a lower intensity of rehabilitation because of fatigue and declining exercise capacity (23, 24). Second, a decrease in physical activity outside of rehabilitation may have affected functional outcomes (25, 26). Third, haemodialysis has been proposed to be catabolic. Exercise therapy is an effective intervention for patients with haemodialysis; however, its effect remains controversial. A randomized controlled trial of resistance training, which included 2 sets of 10 exercises at a high intensity, 3 times per week for 12 weeks during haemodialysis, showed no significant improvement in thigh muscle quantity or quality (27). In addition, another randomized controlled trial revealed that aerobic exercise training in intradialytic-exercise patients trained 3 times per week for 6 months on a cycle ergometer showed no significant improvement in the 6-min walking test (28). Increased catabolism may result in inadequate improvement in physical function. Thus, haemodialysis may be a barrier to rehabilitation. Lastly, other factors could influence the outcomes. The total FIM cognitive items score on admission was lower and the length of stay in the rehabilitation ward was shorter in the haemodialysis group than in the non-haemodialysis group, although they were not significantly different. For the cognitive domain, statistical differences were observed in some items at discharge. This finding might be mostly attributed to the baseline difference between groups, in that the cognitive item scores tended to be better in the non-haemodialysis group. These factors could have affected the functional outcomes at discharge.
The clinical implications of this study are that even the same amount of rehabilitation for patients with lower limb amputations receiving haemodialysis may not lead to functional outcomes comparable to those without haemodialysis. Several solutions can be proposed. The first simple approach is to further increase rehabilitation time. However, this may not be practical given the time of dialysis and intervention costs. A more feasible approach is to increase rehabilitation intensity without increasing the amount of time required. To increase the intensity of rehabilitation, it may be necessary to increase the frequency of interventions to minimise fatigue. The third approach is to establish a more comprehensive programme that includes enhancing physical activity (25, 26) other than rehabilitative training, and improving nutritional status (29). Future studies with various frequencies, intensities, amounts of time, and types of rehabilitation will provide insights into developing better intervention strategies.
This study has a few limitations. First, this was a single-centre, retrospective study conducted in Japan. Therefore, we believe that the generalisability of this study’s findings to different regions and healthcare systems is limited. Second, the FIM score might not fully elucidate the differences in outcomes between the 2 groups because of its ceiling effect and coarseness of the scoring. More focused outcome measures for patients with lower limb amputation such as indexes of walking ability may be more sensitive in exploring the differences in outcomes between the groups. Third, the sample size was not large enough, although it was similar to the sample sizes in previous studies (8–11). Despite such limitations, there are few reports of rehabilitation for patients with lower limb amputations receiving haemodialysis. We believe that a report with even a small number of patients can provide valuable clinical insights, contribute to future studies through further case accumulation, and lead to important findings on the rehabilitation of patients with lower limb amputation on haemodialysis. Future research is needed to examine other aspects of functional outcomes including walking ability, long-term functional outcome, quality of life, and satisfaction of patients with lower limb amputations undergoing rehabilitation and receiving haemodialysis.
In conclusion, patients with lower limb amputation who were receiving haemodialysis in convalescent rehabilitation ward had poorer FIM effectiveness than those not receiving haemodialysis in this study, even after receiving the same amount of inpatient rehabilitation.
REFERENCES
- Thomas B, Wulf S, Bikbov B, Perico N, Cortinovis M, Courville de Vaccaro K, et al. Maintenance dialysis throughout the world in years 1990 and 2010. J Am Soc Nephrol 2015; 26: 2621–2633. https://doi.org/10.1681/ASN.2014101017
- Kaminski M, Frescos N, Tucker S. Prevalence of risk factors for foot ulceration in patients with end-stage renal disease on haemodialysis. Intern Med J 2012; 42: e120–e128. https://doi.org/10.1111/j.1445-5994.2011.02605.x
- Otte J, van Netten JJ, Woittiez AJ. The association of chronic kidney disease and dialysis treatment with foot ulceration and major amputation. J Vasc Surg 2015; 62: 406–411. https://doi.org/10.1016/j.jvs.2015.02.051
- Gilhotra RA, Rodrigues BT, Vangaveti VN, Malabu UH. Prevalence and risk factors of lower limb amputation in patients with end-stage renal failure on dialysis: a systematic review. Int J Nephrol 2016; 2016: 4870749. https://doi.org/10.1155/2016/4870749
- van Vliet S, Skinner SK, Beals JW, Pagni BA, Fang HY, Ulanov AV, et al. Dysregulated handling of dietary protein and muscle protein synthesis after mixed-meal ingestion in maintenance hemodialysis patients. Kidney Int Rep 2018; 3: 1403–1415. https://doi.org/10.1016/j.ekir.2018.08.001
- Kim JK, Choi SR, Choi MJ, Kim SG, Lee YK, Noh JW, et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr 2014; 33: 64–68. https://doi.org/10.1016/j.clnu.2013.04.002
- Isoyama N, Qureshi AR, Avesani CM, Lindholm B, Barany P, Heimburger O, et al. Comparative associations of muscle mass and muscle strength with mortality in dialysis patients. Clin J Am Soc Nephrol 2014; 9: 1720–1728. https://doi.org/10.2215/CJN.10261013
- Greenspun B, Harmon RL. Rehabilitation of patients with end-stage renal failure after lower extremity amputation. Arch Phys Med Rehabil 1986; 67: 336–338.
- Czyrny JJ, Merrill A. Rehabilitation of amputees with end-stage renal disease. Functional outcome and cost. Am J Phys Med Rehabil 1994; 73: 353–357. https://doi.org/10.1097/00002060-199409000-00009
- Sioson ER, Kerfoot S, Ziat LM. Rehabilitation outcome of older patients with end-stage renal disease and lower extremity amputation. J Am Geriatr Soc 1993; 41: 667–668. https://doi.org/10.1111/j.1532-5415.1993.tb06742.x
- Arneja AS, Tamiji J, Hiebert BM, Tappia PS, Galimova L. Functional outcomes of patients with amputation receiving chronic dialysis for end-stage renal disease. Am J Phys Med Rehabil 2015; 94: 257–268. https://doi.org/10.1097/PHM.0000000000000259
- Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil 1987; 1: 6–18.
- Data management service of the Uniform Data System for Medical Rehabilitation and the Center for Functional Assessment Research: Guide for use of the Uniform Data Set for Medical Rehabilitation. version 3.1. Buffalo: State University of New York at Buffalo; 1990.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806–808. https://doi.org/10.1136/bmj.39335.541782.AD
- Koh GC, Chen CH, Petrella R, Thind A. Rehabilitation impact indices and their independent predictors: a systematic review. BMJ Open 2013; 3: e003483. https://doi.org/10.1136/bmjopen-2013-003483
- Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, et al. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee’s ability to ambulate. Arch Phys Med Rehabil 2002; 83: 613–627. https://doi.org/10.1053/apmr.2002.32309
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. https://doi.org/10.1016/0021-9681(87)90171-8
- Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure (FIM). Scand J Rehabil Med 1994; 26: 115–119.
- HCFA Common Procedure Coding System HCPCS 2001. Washington, DC: US Government Printing Office; 2001.
- Hemmelgarn BR, Manns BJ, Quan H, Ghali WA. Adapting the Charlson comorbidity index for use in patients with ESRD. Am J Kidney Dis 2003; 42: 125–132. https://doi.org/10.1016/S0272-6386(03)00415-3
- Kwakkel G, Wagenaar RC, Koelman TW, Lankhorst GJ, Koetsier JC. Effects of intensity of rehabilitation after stroke. A research synthesis. Stroke 1997; 28: 1550–1556. https://doi.org/10.1161/01.STR.28.8.1550
- Clark B, Whitall J, Kwakkel G, Mehrholz J, Ewings S, Burridge J. The effect of time spent in rehabilitation on activity limitation and impairment after stroke. Cochrane Database Syst Rev 2021; 10: CD012612. https://doi.org/10.1002/14651858.CD012612.pub2
- Sietsema KE, Hiatt WR, Esler A, Adler S, Amato A, Brass EP. Clinical and demographic predictors of exercise capacity in end-stage renal disease. Am J Kidney Dis 2002; 39: 76–85. https://doi.org/10.1053/ajkd.2002.29884
- Painter P. Physical functioning in end-stage renal disease patients: update 2005. Hemodial Int 2005; 9: 218–235. https://doi.org/10.1111/j.1492-7535.2005.01136.x
- Johansen KL, Chertow GM, Ng AV, Mulligan K, Carey S, Schoenfeld PY, et al. Physical activity levels in patients on hemodialysis and healthy sedentary controls. Kidney Int 2000; 57: 2564–2570. https://doi.org/10.1046/j.1523-1755.2000.00116.x
- Avesani CM, Trolonge S, Deleaval P, Baria F, Mafra D, Faxen-Irving G, et al. Physical activity and energy expenditure in haemodialysis patients: an international survey. Nephrol Dial Transplant 2012; 27: 2430–2434. https://doi.org/10.1093/ndt/gfr692
- Cheema B, Abas H, Smith B, O’Sullivan A, Chan M, Patwardhan A, et al. Progressive exercise for anabolism in kidney disease (PEAK): a randomized, controlled trial of resistance training during hemodialysis. J Am Soc Nephrol 2007; 18: 1594–1601. https://doi.org/10.1681/ASN.2006121329
- Koh KP, Fassett RG, Sharman JE, Coombes JS, Williams AD. Effect of intradialytic versus home-based aerobic exercise training on physical function and vascular parameters in hemodialysis patients: a randomized pilot study. Am J Kidney Dis 2010; 55: 88–99. https://doi.org/10.1053/j.ajkd.2009.09.025
- Maraj M, Kusnierz-Cabala B, Dumnicka P, Gala-Bladzinska A, Gawlik K, Pawlica-Gosiewska D, et al. Malnutrition, inflammation, atherosclerosis syndrome (MIA) and diet recommendations among end-stage renal disease patients treated with maintenance hemodialysis. Nutrients 2018; 10: 69. https://doi.org/10.3390/nu10010069