CASE REPORT
RARE CASE OF HIP PAIN DUE TO ILIOPSOAS TENDON RUPTURE; A CASE REPORT AND REVIEW OF THE LITERATURE
Alpha ANDERS, MD1 and Kenneth VITALE, MD, FACSM, FAAPMR2
From 1Louisiana State University School of Medicine, New Orleans, Lousiana, United States and 2Department of Orthopaedic Surgery, University of California School of Medicine, La Jolla, California, United States
Objective: Hip pain is common in patients of advanced age and has a very broad differential. Of the potential aetiologies, iliopsoas tendon ruptures are rare. Consequently, there is a paucity of literature on iliopsoas rupture in the older adult population, and its rarity can lead to a delay in its diagnosis. When iliopsoas ruptures do occur, they are typically secondary to trauma; however, they can occur spontaneously. Iliopsoas injuries can be disabling, but they respond well to conservative management. We report here a case of a 70-year-old woman who presented to an unaffiliated emergency department with left anterior hip pain 2 weeks after a fall from standing height.
Results: Initial X-ray and computed tomography were negative for fracture, and the patient was discharged with home health physical therapy. Her symptoms persisted. At a subsequent emergency department visit several weeks later, magnetic resonance imaging revealed a complete left iliopsoas tendon rupture with retraction. She was treated conservatively and made a complete recovery after physical therapy.
Discussion: This paper reviews the literature related to iliopsoas injuries, highlights the importance of iliopsoas tendon injuries among the differential for acute hip pain, and provides management recommendations for this rare, but probably underdiagnosed, injury. This treatable condition warrants further attention, as delay in diagnosis can prolong morbidity.
LAY ABSTRACT
Hip pain is common in the elderly population and has many causes. Of the potential sources of hip pain, a complete tear of the iliopsoas, or hip flexor, tendon is rare. When iliopsoas tears do occur, it is typically after trauma, such as a fall. However, tears can happen spontaneously. Diagnosis is best made using magnetic resonance imaging (MRI), but can be made with ultrasound. These injuries can be disabling, but respond well to conservative management consisting of rest and pain management principles, followed by physical therapy active rehabilitation. This paper reviews the literature on iliopsoas tears, provides management recommendations for this rare, but probably underdiagnosed, injury, and reports a case of a 70-year-old woman who experienced a complete iliopsoas tear after a fall from standing height. The diagnosis was missed on initial evaluation, and was subsequently made using MRI. The patient made a full recovery after conservative management.
Key words: iliopsoas; tendon; rupture; pain; rehabilitation; physical therapy.
Citation: JRM-CC 2022; 5: jrmcc00082. DOI: https://doi.org/10.2340/jrmcc.v5.2541
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: May 17, 2022; Published: Aug 18, 2022
Correspondence address: Alpha Anders, 1542 Tulane Avenue, Room 433, New Orleans, Louisiana 70112. E-mail: atanders99@gmail.com
Competing interests and funding: The authors have no conflicts of interest to declare. The authors received no funding, grants or equipment for the project from any source. There are no financial benefits to any author. There are no other presentations, manuscripts, or abstracts of any form.
Hip pain is a common symptom in elderly patients presenting to the emergency department and has a very broad differential (1, 2). Of the potential aetiologies, iliopsoas tendon injuries are extremely uncommon, with an estimated prevalence of 0.66% (3). These tendinous injuries can range from strains and partial tears to complete tears. Iliopsoas injuries are typically secondary to trauma, especially in young athletes. However, complete iliopsoas ruptures can occur even from minor trauma, such as a minor fall from standing height. A few spontaneous injuries have even been reported (3–8). There is a paucity of literature on iliopsoas rupture in the older adult population, and the true incidence of iliopsoas tears is therefore probably under-reported. The rarity of iliopsoas tears can lead to a delay in its diagnosis, and warrants further attention. We present a case of iliopsoas rupture in an older adult, which was missed on initial presentation, and review the available literature on this rare condition.
CASE REPORT
A 70 year old woman with a past medical history of chronic low back pain, lumbar spine surgery, spinal cord stimulator implantation, neck pain, cervical spine fusion, Parkinson’s disease, deep brain stimulator implantation, chronic anaemia, hypertension, and unsteady gait necessitating walker use for ambulation presented to the emergency department with persistent subacute left-sided groin pain. At baseline she had been independent, able to walk safely without pain or weakness using a walker, performed all activities of daily living independently, and lived in a single-storey house. While she was walking in the bathroom, she felt lightheaded and fell, without head trauma, loss of consciousness, or apparent musculoskeletal injury. On further discussion, she admitted to falling approximately 3 times, all from standing height, while using a walker. Two weeks after her falls, she was initially evaluated at an unafilliated emergency department. Syncopal work-up was unremarkable. X-ray and left-hip computed tomography (CT) scan ruled out a fracture. She was discharged home and treated by home health physical therapy.
The patient’s continued hip pain and difficulty walking prompted her presentation to our emergency department 2 weeks later. On examination, she had appreciable swelling of her left anterior thigh, with dependent oedema extending down to the calf, left anterior hip tenderness to palpation, limited hip flexion active range-of-motion (ROM), and 3/5 hip flexor strength. X-ray of the hip demonstrated degenerative changes without any acute osseous findings at the lesser trochanter (Fig. 1). Magnetic resonance imaging (MRI) of the left hip was recommended due to suspicion of further injury not appreciated on prior work-up. The MRI demonstrated a complete tear of the left iliopsoas tendon at the lesser tuberosity insertion, tendon retraction of approximately 5 cm (Fig. 2) with associated oedema and muscle oedema/strain of iliacus and psoas major (Fig. 3). Incidentally, there was additional mild oedema of the left proximal hamstring myotendinous junction and obturator internus, reflecting low-grade associated injury, and overall mild tendinosis of the left hamstring origin.
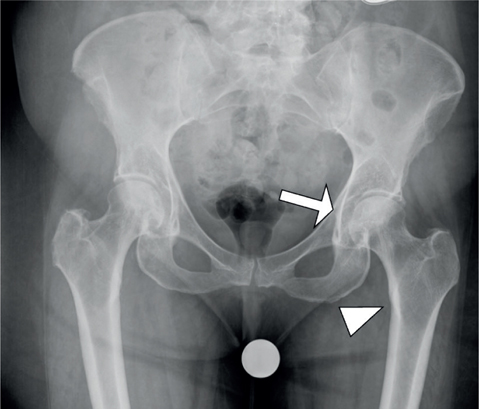
Fig. 1. Anteroposterior (AP) X-ray of the hips demonstrating degenerative changes at the femoracetabular joint (arrow). There are no acute findings at the lesser trochanter (arrow head).
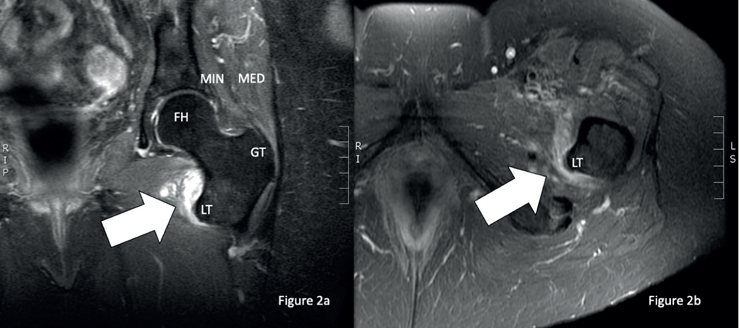
Fig. 2. Complete tear of the left iliopsoas tendon. (a) Coronal T2 fat-saturdated magnetic resonance imaging (MRI) of the left hip demonstrating the absence of the left iliopsoas tendon (arrow) at the lesser trochanter (LT) of the femur and presence of hyperintense oedema. The gluteus minimums (MIN) and gluteus medius (MED) can be seen in the coronal image attaching to the greater trochanter of the femur. The femoral head (FH) is visualized. (b) Axial T2 fat-saturated MRI view of the left hip demonstrates the absence of the iliopsoas tendon (white arrow) from the lesser trochanter (LT) of the femur.
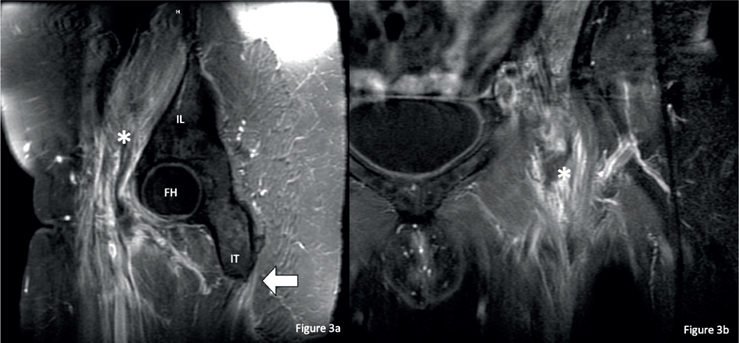
Fig. 3. Left iliopsoas oedema tracking proximally. (a) Sagittal T2 magnetic resonance imaging (MRI) image of the left hip demonstrating hyperintense oedema in the left iliopsoas (asterisk) muscle tracking proximally. The iliacus originates at the ilium (IL) and courses ventral to the femoral head (FH) towards its insertion site at the lesser trochanter. There is hyperintense mild oedema of the left proximal hamstring myotendinous junction near the origination site of the ischial tuberosity (IT) reflecting mild tendinosis of the left hamstring origin. (b) Coronal T2 Fat-saturated MRI of the left hip demonstrating hyperintense oedema (asterisk) in the left iliopsoas muscle tracking proximally.
The patient was treated conservatively with a period of rest and activity modification, and pain management. She was instructed to become weight-bearing as tolerated, ambulate with a walker, and begin physical therapy. Guidance on ROM was recommended to progress from active, active-assisted, and passive as tolerated by pain, and only to progress to resistance exercises after achieving pain-free active ROM. At 8 weeks after injury, she could perform active straight leg raise while supine to 15° (active-assisted to 45°) and could actively flex her hip to 45° while standing. At 12 weeks after injury she reported no hip pain and began to have improved step length with active hip flexion symmetrical with the opposite leg. At 3.5 months after initial injury, she had improved remarkably since the initial evaluation, was able to walk without any assistive device, perform squats independently, could lunge walk, and even walk backwards engaging the hip flexors well. She was able to get up off the floor, put on socks, and put on shoes easier and without any assistance.
DISCUSSION
Iliopsoas tendon injuries are most common in the athletic population, seen most often in younger individuals and in team sports involving activities such as kicking and rowing (9, 10). In youth athletes with open apophyses, iliopsoas injuries can result in an avulsion fracture of the lesser trochanter (11). In adults, an iliopsoas avulsion fracture is highly consistent with metastatic disease (5). While there have been a few cases of non-malignant avulsion fractures reported, these are typically associated with predisposing chronic diseases, such as diabetes mellitus, end-stage-renal disease, and systemic lupus erythematosus as primary risk factors (8). Complete iliopsoas tendon ruptures (without avulsion) have also occasionally been seen in patients with total hip arthroplasties (12, 13). A complete iliopsoas tendon rupture in an adult without a history of hip arthroplasty (as in this case study) is extremely rare (3). Of the few reported cases, a delay in diagnosis is relatively common (7, 14).
Diagnosis of iliopsoas tears is best made using MRI. A small study of 19 military subjects demonstrated that MRI was 100% accurate in delineating the aetiology of acute hip pain, including iliopsoas tear injuries, in young endurance athletes (15). Although the participants in this study were of a young and athletic population, multiple case studies have demonstrated the ability of MRI to diagnose iliopsoas tears in the older adult population (3, 4, 6, 8, 13, 14). Findings of abnormal signal intensity on T1 and T2-weighted images, proximal muscle thickening, mass effect on the anterior hip joint, and interruption of the psoas tendon with preserved lateral iliacus muscle insertion fibres are consistent with a rupture of the distal iliopsoas tendon (4)..
With the recent advent of diagnostic musculoskeletal ultrasound, a skilled ultrasonographer may be able to diagnose this solely by ultrasound (16, 17). Findings include hypoechoic signal and irregularity/partial disruption of the tendon’s fibrillar pattern in partial tears, and discontinuity, often with haematoma, in complete tears. Traditionally the iliopsoas tendon can be examined in its long-axis, although newer techniques utilizing the flexion-abduction-external rotation (FABER) position have been described that may increase diagnostic yield and accuracy of visualizing the distal iliopsoas tendon (16). However, due to the depth of the iliopsoas tendon and associated haematoma, which may obscure the ultrasound signal, the authors consider that MRI remains the gold standard to diagnose this injury. A protocol-driven approach when evaluating groin pain with ultrasound is recommended to avoid potential pitfalls (18).
The true incidence of iliopsoas ruptures may be under-reported. The best estimate of iliopsoas injury prevalence is from a retrospective study of 4,862 consecutive MRI examinations of the hips and pelvis (3). They identified 32 patients (16 cases over the age of 65 years and 16 cases under 65 years) with iliopsoas injuries, resulting in a 0.66% prevalence. In this study, the injuries were graded as muscle strain, incomplete tear, and complete tear. In patients under 65 years of age, the most common injuries were muscle strains and partial tendon tears, often secondary to an athletic injury. Conversely, patients over 65 years of age most frequently experienced complete tears. Of the 16 patients over 65 years of age with an iliopsoas injury, only 2 of them were spontaneous. The study estimated the overall prevalence of complete tears to be 0.16%, and complete tears were exclusively noted in women between the 7th and 10th decades (3). These numbers are probably an underestimate, as a delay in diagnosis is common (7, 14) and can be missed initially, as in the current case report.
Treatment for strains and partial tears is usually conservative, including physical therapy and pain management (6). There is a paucity of literature on iliopsoas rupture treatment, including surgical management. Evidence from relevant case reports suggests that complete iliopsoas tears can also be treated conservatively without surgical intervention (3, 4, 6–8, 12, 14). In younger populations, athletes, and in cases of avulsion fractures, surgery can be considered if there is significant displacement (19). With conservative treatment the prognosis is favourable, usually with a significant improvement in symptoms and overall function.
This case highlights the importance of including iliopsoas rupture in the differential diagnosis of hip pain, and the utility of MRI in making the diagnosis when initial work-up is negative. Based on the available literature, with consideration of risk stratification, a female patient and age above 65 years are the 2 largest non-modifiable risk factors for a complete iliopsoas rupture. Furthermore, this case illustrates how even minor trauma, such as a simple minor fall from standing height, may also result in iliopsoas rupture. An argument could be made that this was a spontaneous rupture in the absence of clear major trauma; however, given the extreme rarity of spontaneous ruptures, a fall was probably the inciting event. Interestingly, the CT scan failed to accurately diagnose the injury (if it did occur at initial presentation), therefore it is possible that the previous falls may have triggered a subclinical injury that spontaneously ruptured later (as she did not report an additional fall at subsequent visits). Nevertheless, the patient’s injury remained undiagnosed for 1 month despite work-up. Therefore providers should be aware of this diagnosis and have a high index of suspicion for iliopsoas injury, lowering their threshold for ordering advanced imaging.
CONCLUSION
We report here a case of a 70-year-old patient who experienced a rare complete iliopsoas tendon rupture, probably secondary to a simple minor fall. She remained misdiagnosed for a month, despite having been evaluated shortly after injury. While iliopsoas injures, in general, are uncommon, complete iliopsoas tendon ruptures are extremely rare. As a result, they may be underdiagnosed or missed, as in this case. The true incidence is probably under-reported, highlighting the need for heightened awareness of this injury, especially in females over the age of 65 years with any history of injury, even a minor injury or incidental fall. Diagnosis can be made with MRI, or by skilled use of musculoskeletal ultrasound. Treatment is generally conservative, involving dedicated physical therapy, assistive devices for ambulation, and pain management. Despite being a severe injury, they typically have favourable outcomes with appropriate treatment, enabling patients to return to their previous level of function.
REFERENCES
- Kohaus H, Peters P, Strunk E. Rupture of the iliopsoas muscle. Symptoms and differential diagnosis (author’s transl). Unfallheilkunde 1980; 83: 127–129.
- Christmas C, Crespo CJ, Franckowiak SC, Bathon JM, Bartlett SJ, Andersen RE. How common is hip pain among older adults? Results from the third national health and nutrition examination survey. J Fam Pract 2002; 51: 345–348.
- Bui KL, Ilaslan H, Recht M, Sundaram M. Iliopsoas injury: an MRI study of patterns and prevalence correlated with clinical findings. Skeletal Radiol 2008; 37: 245–249. doi: 10.1007/s00256-007-0414-3
- Lecouvet FE, Demondion X, Leemrijse T, Vande Berg BC, Devogelaer J, Malghem J. Spontaneous rupture of the distal iliopsoas tendon: clinical and imaging findings, with anatomic correlations. Eur Radiol 2005; 15: 2341–2346. doi: 10.1007/s00330-005-2811-0
- James SLJ, Davies AM. Atraumatic avulsion of the lesser trochanter as an indicator of tumour infiltration. Eur Radiol 2006; 16: 512–514. doi: 10.1007/s00330-005-2675-3
- Stark J. Spontaneous iliopsoas tendon rupture: a case report and brief review. Arch Orthop Trauma Surg 2021; 141: 1633–1637. doi: 10.1007/s00402-020-03523-2
- Emam M, Farmakidis C, Lee SW, Wainapel SF. Spontaneous iliopsoas tendon rupture: an uncommon cause of hip pain in elderly patients. PM R 2016; 8: 75–77. doi: 10.1016/j.pmrj.2015.07.007
- DePasse JM, Varner K, Cosculluela P, Incavo S. Atraumatic avulsion of the distal iliopsoas tendon: an unusual cause of hip pain. Orthopedics 2010; 33: 8. doi: 10.3928/01477447-20100625-25
- Bouvard M, Roger B, Laffond J, Lippa A, Tassery F. Iliopsoas muscle injuries. In: Muscle injuries in sport athletes. Springer, Cham, Switzerland; 2017, p. 245–259. doi: 10.1007/978-3-319-43344-8_15
- Fredberg U, Hansen LB, Kissmeyer-Nielsen P, Torntoft EB. Iliopsoas tendinitis in athletes. Diagnosis and treatment. Ugeskr Laeger 1995; 157: 4031–4033.
- Theologis TN, Epps H, Latz K, Cole WG. Isolated fractures of the lesser trochanter in children. Injury 1997; 28: 363–364. doi: 10.1016/S0020-1383(97)00017-X
- Piggott RP, Doody O, Quinlan JF. Iliopsoas tendon rupture: a new differential for atraumatic groin pain post-total hip arthroplasty. BMJ Case Rep 2015. doi: 10.1136/bcr-2014-208518
- Maheshwari AV, Malhotra R, Kumar D, Pitcher JD. Rupture of the ilio-psoas tendon after a total hip arthroplasty: an unusual cause of radio-lucency of the lesser trochanter simulating a malignancy. J Orthop Surg Res 2010; 5: 6. doi: 10.1186/1749-799X-5-6
- Freire V, Bureau NJ, Deslandes M, Moser T. Iliopsoas tendon tear: clinical and imaging findings in 4 elderly patients. Can Assoc Radiol J 2013; 64: 187–192. doi: 10.1016/j.carj.2012.05.003
- Shin AY, Morin WD, Gorman JD, Jones SB, Lapinsky AS. The superiority of magnetic resonance imaging in differentiating the cause of hip pain in endurance athletes. Am J Sports Med 1996; 24: 168–176. doi: 10.1177/036354659602400209
- Balius R, Pedret C, Blasi M, et al. Sonographic evaluation of the distal iliopsoas tendon using a new approach. J Ultrasound Med 2014; 33: 2021–2030. doi: 10.7863/ultra.33.11.2021
- Dawes ARL, Seidenberg PH. Sonography of sports injuries of the hip. Sports Health 2014; 6: 531–538. doi: 10.1177/1941738114552801
- Jacobson JA, Khoury V, Brandon CJ. Ultrasound of the groin: techniques, pathology, and pitfalls. AJR Am J Roentgenol 2015; 205: 513–523. doi: 10.2214/AJR.15.14523
- Eberbach H, Hohloch L, Feucht MJ, Konstantinidis L, Südkamp NP, Zwingmann J. Operative versus conservative treatment of apophyseal avulsion fractures of the pelvis in the adolescents: a systematic review with meta-analysis of clinical outcome and return to sports. BMC Musculoskelet Disord 2017; 18: 162. doi: 10.1186/s12891-017-1527-z