CASE REPORT
OSTEOCHONDROSES IN CHILDREN’S SPORTS PRACTICE – A RARE CASE OF VAN NECK–ODELBERG DISEASE
João P. FONSECA, MD1, Pedro FIGUEIREDO, MD1,2 and João P. PINHEIRO, MD, PhD1,2
From 1Department of Physical and Rehabilitation Medicine, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal and 2Faculty of Medicine, University of Coimbra, Coimbra, Portugal
Background: Osteochondroses are a set of conditions concerning the ossification of the developing bone. Higher intensity in sports activities can increase its occurrence in children. There is no consensus on its etiology, with multiple factors being involved. Van Neck–Odelberg disease is a rare osteochondrosis located in ischiopubic synchondrosis. Treatment is mainly conservative, with activity suspension. Addressing and correcting the predisposing factors is crucial to these injuries.
Case report: We present a case of a 6-year-old futsal player who experienced mechanical inguinal moderate pain during sports practice. After performing physical examination, laboratory tests, and radiographic evaluation, the patient was diagnosed with Van Neck–Odelberg disease. Sports activities were suspended while a conservative treatment was performed, with subsequent follow-up over 3.5 years. No symptom recurrence was reported.
Conclusion: Increased intensity of sports activities is associated with overuse injuries in children, especially before completing the ossification process. Preventive measures must remain the primary concern in children’s sports practice.
LAY ABSTRACT
Osteochondroses are a group of disorders that affect normal bone growth. The cause for these disorders is not well understood, involving different factors. Osteochondroses can occur in children’s sports practice, affecting performance or even leading to its abandonment. Van Neck–Odelberg disease is one of these disorders that affects a temporary joint located in the inguinal area and that only exists during childhood. This paper presents a case and respective follow-up of a 6-year-old futsal player diagnosed with Van Neck–Odelberg disease. This paper also reviews the possible contributing factors, differential diagnoses, treatment options, and preventive measures.
Key words: osteochondrosis; sports, overuse injury; childhood; rehabilitation.
Citation: JRM-CC 2022; 5: jrmcc00090. DOI: https://doi.org/10.2340/jrmcc.v5.4593
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Oct 28, 2022; Published: Dec 9, 2022
Correspondence address: João P. Fonseca, Department of Physical Medicine and Rehabilitation, Centro Hospitalar e Universitário de Coimbra, Praceta Mota Pinto 3004-561, Coimbra. E-mail: joaopfonseca58653@gmail.com
Osteochondroses are a group of disorders that affect normal bone growth, involving primarily conjugation cartilages or centres of ossification. Although unrelated to each other, they share some common features such as preferential involvement of immature skeleton in epiphyses or apophyses. The radiographic aspect is dominated by bone fragmentation, collapse, sclerosis or reossification (1–3).
The pathogenesis of osteochondroses is not fully understood. However, aseptic necrosis of a previously normal epiphysis is prevalent because of repeated trauma, vascular or macrotraumatic events. There are several classifications to identify these injuries. The most used is Siffert classification, based on anatomic location (1, 2). Osteochondroses can occur in children sports practice, especially during rapid growth, changes in external training load, technical gestures, equipment or field differences. They affect performance or even cause the athletes to stop sports practice.
In this paper, we present a clinical report and follow-up of a child futsal player who has Van Neck–Odelberg disease (VNOD).
CASE REPORT
A 6-year-old boy, overweight, futsal player with 1 h of training volume, 4 times a week. Referred in August 2017 to the Pediatric Rehabilitation consultation at the Physical Medicine and Rehabilitation Department because of mechanical right inguinal pain as well as limp, during sports practice, especially during running activities. Pain was classified as moderate (Numeric Rating Pain Scale 5/10). Sports practice interruption and 10 mg/kg of ibuprofen provided symptomatic relief. There was a previous history of right hip synovitis 1 year before and bronchoreactive symptoms. No other complaints were reported such as fever, weight loss or major trauma.
Clinical examination revealed dynamic flat foot and bilaterally valgus knee. On palpation, pain was located on the right ischiopubic area and adductor muscles. Resisted contraction of adductors and hamstrings was not painful. On passive mobilization, limitation of range of motion (ROM) on the right hip joint was evident, especially in abduction and lateral and medial rotation. Strength of the right adductor and rotator muscles was slightly reduced. Gait analysis revealed right limb claudication, decreased speed and increased cycle duration. No other findings were present.
Laboratory tests revealed normal values in red and white cell count, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Radiographic evaluation revealed right ischiopubic synchondrosis hypertrophy, with focal areas of bone demineralization (Fig. 1). Considering these findings, VNOD was hypothesized. The patient was recommended with relative rest, suspension of sports practice for 6 weeks and moderation in running activities. Reassessment consultation was scheduled in 8 weeks (Figs. 1 and 2).
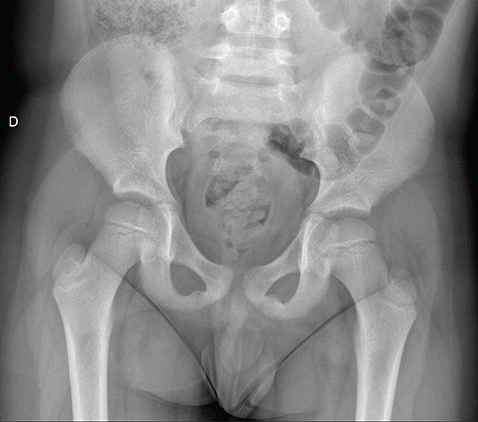
Fig. 1. Anteroposterior pelvis radiographs showing hypertrophy and demineralization of the right ischiopubic synchondrosis.
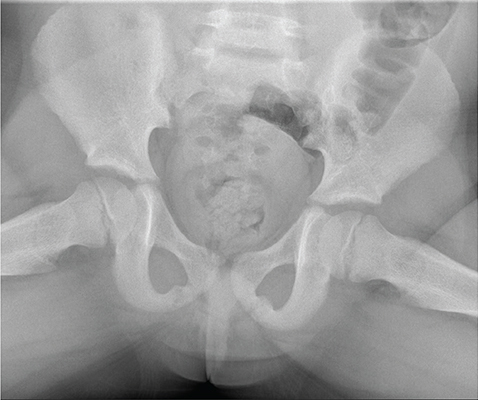
Fig. 2. Anteroposterior pelvis radiographs showing hypertrophy and demineralization of the right ischiopubic synchondrosis.
Despite recommendations, the patient resumed futsal practice just 2 weeks after the consultation, with similar training intensity. This led to symptom recurrence and impairment. For these reasons, the patient stopped sports practice.
In reassessment appointment, despite a slight improvement, the patient still reported pain on the right groin region, with a slight limp when walking. For this reason, a rehabilitation programme was prescribed, with load adjustment on the right ischiopubic muscle insertion, muscle strengthening exercises, proprioceptive training and neuromotor coordination. Considering clear radiographic findings, magnetic resonance imaging (MRI) was not requested.
Reassessment after 6 months revealed total absence of pain, symmetrical hamstring flexibility, functional neuromotor and proprioceptive control. Gait evaluation revealed complete improvement, without limping or changes in speed or cadence. Despite the complete resolution of the clinical picture, the patient ended up abandoning the practice of futsal. The patient was discharged 3.5 years later without any symptom recurrence.
DISCUSSION
The term osteochondrosis refers to a heterogeneous group of disorders that affect the epiphysis or its equivalent of immature skeletal segments. The terminology used in the literature remains a confounding factor. The terms “osteochondrosis,” “osteochondritis” and “apophysitis” are still used indiscriminately. This lack of uniformity creates problems in the scientific debate (2). Osteochondrosis can be epiphyseal, physeal or apophyseal, depending on the affected site. Although there is no consensus on the etiology of osteochondrosis, injuries involving the apophyses may have a traumatic origin, because of the asymmetrical growth of bone and myotendinous structures, resulting in traction injuries. The etiology of epiphyseal lesions is less consensual, involving one or more factors, including genetic, traumatic, vascular as well as rapid growth (1).
VNOD is a rare osteochondrosis located in ischiopubic synchondrosis, a temporary joint that only exists in childhood. It originates from 2 ossification centres located in the ischiopubic region, divided by a thin fibrocartilaginous lamina (4). The ossification process starts in early childhood and ends before puberty (5). The presence of ischiopubic synchondrosis occurs, mostly, between 4 and 16 years, being more prevalent in younger age groups (6). Before completing the ossification process and during the growth period, ischiopubic synchondrosis may increase in size because of asymmetric mechanical stress mainly caused by the adductor muscles and hamstrings (7). Consequently, synchondrosis remains under constant dynamic stress, leading to an inflammatory reaction. This entire process delays the union of cartilages and ossification centres (5). Asymmetry is characteristic of this process and may be inversely correlated with limb dominance. The explanation may come from the abnormal distribution of ground reactive forces applied to the load-bearing limb, compared to the dominant one (8). There are several factors that influence this process. Sports practice is one of them, especially when unequal physical efforts are performed such as kicking, jumping or running (6).
The diagnosis is essentially clinical and characterized by mechanical pain in the inguinal region, contracture in the surrounding muscles with associated limp in gait. No suggestive laboratory alterations are identified. Conventional radiography presents the characteristic image of increased volume of ischiopubic synchondrosis, with focal areas of bone demineralization. Differential diagnosis includes stress fractures, post-traumatic osteolysis, osteomyelitis or malignancy. When necessary, MRI can help in diagnosis. On MRI, the ischiopubic region exhibits a hyperintense signal on T2, fat saturation or STIR and a hypointense signal on T1. In addition, fusiform edema and fibrous bridge can be observed with altered signal from the surrounding tissue (6).
Although rare, this is a benign disorder. Treatment is essentially conservative with rest and anti-inflammatory therapy. The clinical and functional prognosis is excellent, as demonstrated in the clinical case, as well as in the various reports found in the literature (4, 5, 7, 9–15). In most cases, there is normalization of imaging findings, something that was not proven in this clinical case because of the absence of symptoms that could justify further study. Synchondrosis ossification is in most cases asymptomatic, and it is accepted that radiographic synchondrosis anomalies may occur as part of normal bone maturation. When these changes become symptomatic, the debate remains whether it is a pathological process or a variant of normal ossification (7). A recent retrospective study proposed the use of a clinical follow-up algorithm to reduce the use of diagnostic exams (16).
The increase in the intensity of sports activities, associated with greater demand in terms of performance, increases the occurrence of overuse injuries in children (1). These lesions are located mainly in the epiphyseal cartilage and can lead to osteochondroses. Most overuse injuries involve the lower limbs, especially the knees, ankles and feet. However, they all have excessive overload as a common element.
When considering a child’s sports activities, we cannot limit to the number of hours spent each week, but also the number of recreational physical activities in and out of school. Thus, on the one hand, there are several children who are physically overloaded, which can result in overuse injuries. On the other hand, the decrease in children’s daily physical activity, and replacement with sedentary activities, leads to a lower baseline fitness level in children. This creates the perfect environment for an increase in overuse injuries (1).
Preventive treatment must remain the main objective so that children can resume their physical activities as quickly and completely as possible under optimal conditions. It is also important to better understand this problem to improve our understanding of why these injuries occur. First, it is important to assess and maintain healthy lifestyles. Likewise, the identification of age-appropriate sports equipment is crucial (1).
The child’s puberty stage must be considered. In addition to somatic growth, there is also a process of neuromotor maturation. This creates windows of opportunity for the development of different physical abilities. Bone maturation and growth rates are related to growth plate injuries (17). Overuse injuries can be precipitated by parents or trainers who are unaware of the fragility of the cartilage structure before the age of 12 years. In most cases, team sports training is done with children of the same age group. However, this is a chronological age. As the age of puberty onset varies, the type and load of training must be adapted to the degree of maturation. Despite the difficult practical application, the teacher or coach must be aware of this problem to better adapt to the load and reduce the risk of injuries and under penalty of increasing sports abandonment, even if it is not in a competitive environment, as occurred in the clinical case presented. Facing an injury of this type, the “10% rule” can be generally applied (1).
The level of a child’s fitness is also important. Flexibility training contributes to athletic performance, especially before peak growth begins. Stiffness is a significant factor in overuse injuries, which need to be fought during the entire rapid limb growth phase, even in the absence of pain. Finally, the child needs to be involved in the entire process. The child athlete must learn to pay attention to their body so they can slow down, change or stop a painful movement. The family and the coach should also be involved in this process.
Conflicts of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
There were no external funding sources for the realization of this paper.
Consent for Publication
Consent for publication was obtained.
Confidentiality of Data
The authors declare that they have followed the protocols of their work centre on the publication of patient data.
REFERENCES
- Launay F. Sports-related overuse injuries in children. Orthop Traumatol Surg Res. 2015; 101 1 Suppl: S139–S147. https://doi.org/10.1016/j.otsr.2014.06.030
- Danger F, Wasyliw C, Varich C. Osteochondroses. Semin Musculoskelet Radiol 2018; 22(1): 118–124. https://doi.org/10.1055/s-0038-1627094
- West EY, Jaramillo D. Imaging of osteochondrosis. Pediatr Radiol. 2019; 49(12): 1610–1616. https://doi.org/10.1007/s00247-019-04556-5
- Ceri L, Sperati G. Van Neck-Odelberg disease in a 8-year-old children: a rare case report. Acta Biomed 2020; 91(4-S): 238–240. https://doi.org/10.23750/abm.v91i4-S.9608
- Chaudhari AP, Shah G, Patil SS, Ghodke AB, Kelkar SB. Van Neck-Odelberg disease: a rare case report. J Orthop Case Rep 2017; 7(1): 24–27. https://doi.org/10.13107/jocr.2250-0685.672
- Herneth AM, Trattnig S, Bader TR, Ba-Ssalamah A, Ponhold W, Wandl-Vergesslich K, et al. MR imaging of the ischiopubic synchondrosis. Magnetic Resonance Imaging 2000; 18(5): 519–524. https://doi.org/10.1016/S0730-725X(00)00138-7
- Wait A, Gaskill T, Sarwar Z, Busch M. Van neck disease: osteochondrosis of the ischiopubic synchondrosis. J Pediatr Orthop 2011; 31(5): 520–524. https://doi.org/10.1097/BPO.0b013e31821f9040
- Herneth AM, Philipp MO, Pretterklieber ML, Balassy C, Winkelbauer FW, Beaulieu CF. Asymmetric closure of ischiopubic synchondrosis in pediatric patients: correlation with foot dominance. AJR Am J Roentgenol 2004; 182(2): 361–365. https://doi.org/10.2214/ajr.182.2.1820361
- Macarini L, Lallo T, Milillo P, Muscarella S, Vinci R, Stoppino LP. Case report: multimodality imaging of van Neck-Odelberg disease. Indian J Radiol Imaging 2011; 21(2): 107–110. https://doi.org/10.4103/0971-3026.82286
- Narayanan SA, Chandy LJ, Kandathil JC. Van Neck disease: a rare case. Case Rep Orthop Res 2021; 4(1): 39–42. https://doi.org/10.1159/000512076
- Iqbal M, Naeem M, Imran MB, Afzal MS, Akhtar MS. Ischio-pubic osteochondritis (Van Neck-Odelberg disease): a case report. Eur J Med Case Rep 2017; 1(3): 144–147. https://doi.org/10.24911/ejmcr/1/34
- Sabir N, Çakmak P, Yılmaz N, Yüksel S. Osteochondrosis of ischiopubic synchondrosis: Van Neck-Odelberg disease. J Pediatr 2021; 229: 307–308. https://doi.org/10.1016/j.jpeds.2020.09.027
- Beyitler I, Kavukcu S. A case of van Neck-Odelberg disease and intermittent overuse injury. Arch Rheumatol 2016; 31(4): 381–383. https://doi.org/10.5606/ArchRheumatol.2016.6009
- Camacho DAH, Bernal P, Cifuentes L, Rivero O. Van Neck-Odelberg disease: a rare cause of pain in pediatric pelvis. World J Nucl Med 2020; 19(4): 435–437. https://doi.org/10.4103/wjnm.WJNM_67_19
- Stormacq S, Gauquier N, Gilliaux O. Un cas d’osteochondrose ischiopubienne revelee par une “synovite aigue transitoire de hanche” atypique. Arch Pediatr 2017; 24(11): 1111–1114. https://doi.org/10.1016/j.arcped.2017.08.022
- Schneider KN, Lampe LP, Gosheger G, Theil C, Masthoff M, Rödl R, et al. Invasive diagnostic and therapeutic measures are unnecessary in patients with symptomatic van Neck–Odelberg disease (ischiopubic synchondrosis): a retrospective single-center study of 21 patients with median follow-up of 5 years. Acta Orthop 2021; 92(3): 347–351. https://doi.org/10.1080/17453674.2021.1882237
- Wik EH, Martínez-Silván D, Farooq A, Cardinale M, Johnson A, Bahr R. Skeletal maturation and growth rates are related to bone and growth plate injuries in adolescent athletics. Scand J Med Sci Sports. 2020; 30(5): 894–903. https://doi.org/10.1111/sms.13635