ORIGINAL REPORT
QUALITY OF LIFE AFTER CORONAVIRUS DISEASE 2019 HOSPITALIZATION AND REHABILITATION NEEDS
Nikolaos KINTRILIS, MD, MSc, PhD1, Antonis KONTAXAKIS, MD, FEBPRM2, Athanasia PAPALAMPIDOU, MD2, Prokopios MANTHOS, MD, MSc, FEBPRM3, Zaira SIMEONIDOU, MD, MSc, FEBPRM2, Aggeliki STAVRIANOU, MD, MSc, FEBPRM4, Eleni MOUMTZI-NAKKA, MD, MSc, FEBPRM2, Iosif GALINOS, MD1 and Christina A. RAPIDI, MD, MSc, LFEBPRM3
From the 1Infectious Disease Unit, 401 General Military Hospital of Athens, Athens, 2Physical and Rehabilitation Medicine Department, 414 Military Hospital of Special Diseases, Penteli, 3Physical and Rehabilitation Medicine Department, General Hospital of Athens, “Gennimatas”, Athens and 4Physical and Rehabilitation Medicine Center, General Hospital of Florina “Elena Dimitriou”, Florina, Greece
Introduction: During the current pandemic, there has been a paucity of Greek data in terms of recording the general long-term functional status of patients after coronavirus disease 2019 (COVID-19) hospitalizations, as well as very little information regarding rehabilitation services nationwide and their utilization.
Objective-design: This is a prospective cohort study, including 92 adults discharged from the Infectious Disease Unit of a third-level hospital in Greece after hospitalization with COVID-19. Demographics and disease severity data was collected upon admission and symptoms at discharge, 4 months and 1 year. Following rating of 12 common symptoms on a Likert scale, quality-of-life data and accessibility to rehabilitation services were compared among the 3 time points.
Results: At discharge, the most prevalent complaints were fatigue, exertional dyspnoea and difficulty walking. At 4 months, these 3 remained among the most prevalent symptoms, while pain and memory/loss concentration remained at high numbers as well. Finally, at the 1-year mark, the percentages of patients reporting fatigue, exertional dyspnoea and pain were the highest. At the 4-month follow-up, only 4.3% of the study participants had visited a rehabilitation facility of any kind, whereas at the 1-year mark the percentage rose to 10.9%.
Conclusion: A clinically relevant number of participants experienced at least one post-COVID-19 hospitalization symptom. Quality of life was markedly affected by the longer-term effects of the disease. The percentage of people finally attending any kind of rehabilitation service was poor. With thousands more being infected and needing hospitalization nationwide daily, the need for the inclusion of relevant rehabilitation programmes in the Greek healthcare system appears imminent.
LAY ABSTRACT
For this research paper, we studied 92 adults discharged from the Infectious Disease Unit of a third-level hospital after hospitalization with COVID-19, examining their quality of life and accessibility to rehabilitation services among 3 time points: discharge, 4 months and 1 year afterwards. At discharge, the most prevalent complaints were fatigue, exertional dyspnoea and difficulty walking. At 4 months, these 3 remained among the most prevalent symptoms, while pain and memory/loss concentration remained at high numbers as well. Finally, at the 1-year mark, the percentages of patients reporting fatigue, exertional dyspnoea and pain were the highest. Quality of life was markedly affected by the longer-term effects of the disease. The percentage of people finally attending any kind of rehabilitation service was poor. Without a doubt, the need for inclusion of rehabilitation programmes in the healthcare systems is imminent in order to face the continued pandemic challenge.
Key words: SARS-CoV-2; COVID-19; hospitalization; quality of life; post-COVID-19 condition; rehabilitation.
Citation: JRM-CC 2023; 6: jrmcc00091. DOI: http://dx.doi.org/10.2340/jrmcc.v6.5327
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Nov 24, 2022; Published: Jan 8, 2023
Correspondence address: Nikolaos Kintrilis, Infectious Diseases Unit, 401 General Military Hospital of Athens, P. Kanellopoulou Avenue 1, Athens, 115 25, Greece. E-mail: nikoskint@hotmail.com
Competing interests and funding: The authors have no conflicts of interest to declare.
None declared.
While these lines are being written, the ongoing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has already been in our lives for close to 3 years, first recognized in the province of Wuhan, China, in late 2019 in a cluster of patients presenting with respiratory system symptoms of unknown origin (1). As of early November 2022, more than 624 million infections had been confirmed, with more than 6.5 million deaths having occurred because of the novel coronavirus and related sequelae worldwide, according to the World Health Organization epidemiological updates (2). Upon emergence of the virus, the initial public health response focused exclusively on providing medical treatment to the sufferers of the coronavirus disease 2019 (COVID-19), the respiratory syndrome caused by SARS-CoV-2. Shortly afterwards, however, it became apparent that SARS-CoV-2 infection and COVID-19 may lead to a plethora of short-, middle- and long-term physical and mental health complications, which can be notoriously difficult to recognize, let alone treat effectively (3). Western national healthcare systems have been more and more concerned with implementing post-COVID functional assessment of patients and rehabilitation services so that individuals can recover in a holistic way and return to society (4). Fatigue, dyspnoea, muscle weakness, arthralgia, as well as anxiety and depression appear to present with increased prevalence among patients, while a systematic review and meta-analysis of 1-year follow-up studies concluded that women and more severe cases are affected with a higher frequency (5–7). What remains non-negotiable, though, is the fact that Post Acute Covid Syndrome (PACS) stems from the complexity and diversity of the SARS-CoV-2 infection, thus requiring a multidisciplinary approach from specialists for its prompt and effective management (8).
At the same time, based on WHO reports, the SARS-CoV-2 pandemic has caused 5,135,200 confirmed cases within the Greek borders, costing the lives of 33,574 individuals (9). Moreover, the lack of national primary healthcare services – characteristically, one- to two-thirds of patients attending a third-level hospital emergency department (ED), has a medical problem that could be effectively managed at the primary healthcare level – whereupon infected patients could seek initial assessment led to a congestion of large hospitals (10). Apart from recording infection rates and relevant statistics interpretation, there has up to this point in time been a shortage in Greek national data regarding post-COVID consequences, let alone follow-up, assessment, and referral of infected patients to rehabilitation services. Of note, the scene of rehabilitation services in Greece remains unchanged through the last years, with the needs of people with disability often being neglected by the official state, leading people suffering from chronic disease or living with a permanent disability to seek private help (11).
In order to efficiently allocate national healthcare resources towards the direction of facing the condition known as PACS, there is a need to not only define which of the longer-term physical and mental health consequences of the pandemic burden the Greek population, but also what can be done for each affected individual. In the present prospective cohort study of COVID-19 patients discharged from a third-level Greek hospital at the time of discharge as well as on 4-month and 1-year follow-up visits, we aimed to examine their general status and post-COVID findings at various points in time.
PATIENTS AND METHODS
Study design and participants
The current prospective longitudinal cohort study included participants from the general population who were diagnosed with PCR-confirmed SARS-CoV-2 infection and had to be hospitalized because of COVID-19 pneumonia, being discharged from a third-level Greek hospital through the period of 1 January 2021–31 May 2021. Patients who were invited to participate in the study were recruited from the Infectious Diseases Unit of a single-centre, the 401 General Military Hospital of Athens, Greece. All PCR-assay confirmatory tests were performed at the outpatient department of the same hospital, and all patients invited to participate in the study had a positive test within 7 days of their admission to the Infectious Diseases Unit. Eligibility criteria for participation in the study were aged 18 years or older, being able to understand and follow study procedures in the Greek language and having been officially discharged from the hospital during the above-mentioned time period. Written informed consent was received from all participants upon enrolment to the study on the day of their discharge from the hospital. All participants of the study were then invited via telephone at the 4-month and 1-year points after their discharge for the two planned follow-ups.
Study procedure
A patient was classified as having severe COVID-19 if, upon presentation at the ED, they had proof of one of the following: oxygen saturation (SpO2) less than 94% on room air at sea level, partial oxygen pressure (pO2) less than 60 mmHg on arterial blood gas (ABG) analysis, fraction of inspired oxygen (PaO2/FiO2 ratio) less than 300 mmHg, respiratory rate greater than 30 breaths per minute or lung infiltrates covering an area greater than 50% of the lung parenchyma on chest X-ray or computed tomography scan. Similarly, a patient was classified as having critical COVID-19 if upon presentation at the ED they required admission to an ICU.
Immediately afterwards, patients were asked upon their current health status, placing emphasis on existence of 12 different symptoms, namely fatigue, resting dyspnoea, exertional dyspnoea, pain, walking difficulty, inability to execute personal hygiene routines, stress, depression, sleep disorders, taste and/or olfactory disorders, difficulty swallowing and memory/concentration impairment. Each of the 12 clinical conditions was rated on a Likert scale of 1–5, where 1 signified absence, 2 mild occurrence, 3 moderate occurrence, 4 severe occurrence and 5 maximum occurrence of the respective symptom. Health-Related Quality of Life (HR-QoL) and general performance status were evaluated using the standardized EuroQoL 5-dimensional-5-levels (EQ 5D-5L) questionnaire, including a subjective perspective of current HR-QoL on a scale of 1–100. EQ 5D-5L includes 5 parameters, namely mobility, self-care, usual activities, pain and depression/anxiety, each one being rated on a scale of 5 degrees, as follows: no problem, slight problems, moderate problems, severe problems and extreme problems/total disability (12).
The study participants were then followed up by telephone at the 4-month and 1-year mark after their discharge from the hospital. During the 2 follow-up interviews, they were asked to report the occurrence of the aforementioned 12 symptoms and, once more, answer the EQ 5D-5L questionnaire.
Data analysis
Descriptive statistics was used to analyse participant demographics and disease severity, with continuous variables being reported as mean±standard deviation and categorical variables as absolute number and/or percentage. A Student t-test was implemented to compare the means of continuous variables and a Pearson’s χ2 test of independence to compare categorical values between different groups of study participants. Primarily, we focused on comparing the prevalence and level of each of the 12 symptoms for each and every one of the 3 time points, after which we aimed to present changes in EQ 5D-5L values and a subjective HR-QoL rating within the observation period. A p < 0.05 was considered statistically significant for the purposes of this study. All statistical analyses were performed using SPSS Statistics version 28.0 (IBM, Armonk, NY, USA).
RESULTS
Study population
A total of 188 patients were discharged from the Infectious Diseases Unit during the studied time period, 178 of whom were eligible and invited to participate in this study. A total of 145 patients accepted the invitation and 92 returned for the 4-month follow-up and the second follow-up visit (48.9% of all discharges, 63.4% of patients who accepted and 91.1% of first follow-up responders) at the 1-year point and these individuals comprised the final study population. Table I summarizes the demographics and disease severity of the study participants. The mean patient age was 50.8±13.5 years (minimum age 19 years and maximum age 90 years) and 68 patients (73.9%) were male. More than half of the patients, specifically 52 individuals (56.5%), had a free medical history up to contracting the infection, while the mean length hospitalization was 6.5±5.7 days, ranging from 1 to 43 days. The 2 most prevalent comorbidities were cardiovascular disease and chronic lung disease [18 (19.6%) and 11 patients (12.0%), respectively]. Regarding disease severity, approximately one-half of the patients, specifically 48 individuals (52.2%), presented with mild to moderate disease, 43 patients (46.7%) had severe disease and 1 patient (1.1%) was in critical condition upon arrival at the ER.
Prevalence of studied symptomatology, EQ 5D-5L assessment and rehabilitation service demand
Table II and Fig. 1 depict the presence of each of the 12 studied symptoms along with the 3 time points included. At the time of discharge, 3 symptoms were present in more than half of the patients, specifically fatigue (75 patients, 81.5%), exertional dyspnoea (57 patients, 62.0%) and difficulty walking (55 patients, 59.8%). The next more prevalent symptoms completing the top 5 were stress (42 patients, 45.7%) and pain (35 patients, 38.0%). At the first follow-up visit, the prevalence of all 12 symptoms was significantly reduced, as summarized in Table II, with the top 3 problems being fatigue (25 patients, 27.2%), pain (16 patients, 17.4%) and exertional dyspnoea (14 patients, 15.2%). At the second follow-up visit, prevalence was still significantly reduced compared to discharge day, but no significant changes had occurred since the first follow-up (Table II). Additionally, top 3 problems remained the same as in the first follow-up visit. Table IV summarizes the mean scoring for each of the EQ 5D-5L variables. At the time of discharge, patients rated their wellness at 63.0 ± 22.9, a score that increased significantly (p < 0.001) to 91.6 ± 10.4 4 months later and slightly dropped (p = 0.566) to 90.6 ± 12.1 at the second follow-up visit. All of the 5 other variables were also scored significantly lower at the 4-month point compared to discharge time.
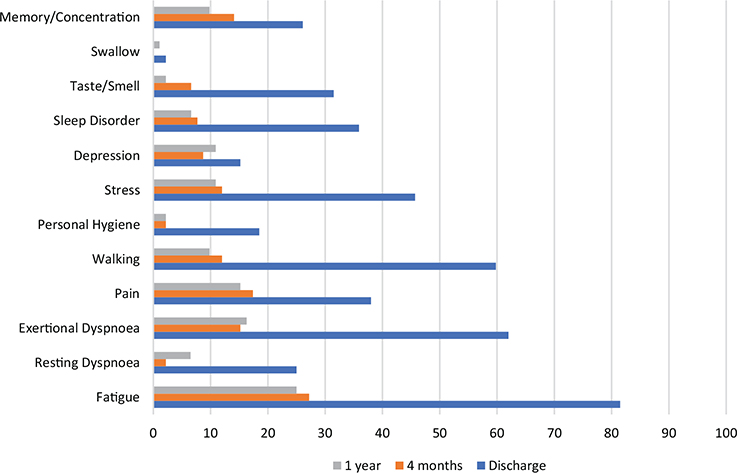
Fig. 1. Percentage of patients mentioning each symptom.
As shown in Fig. 2, when we divided patients into asymptomatic vs symptomatic at the 1-year mark, a worse score on all EQ-5D-5L domains was observed among the former compared to the latter group along all 3 study timestamps. More specifically, reported EQ-5D-5L VAS scores were 96.0 ± 6.1 vs 80.5 ± 13.7, respectively.
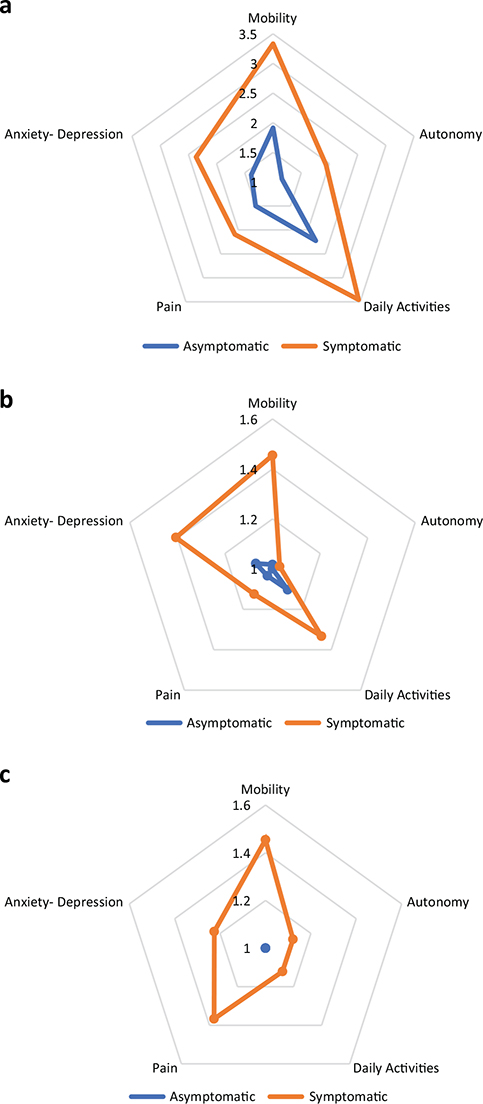
Fig. 2. Each domain of EQ-5D-5L score in asymptomatic and symptomatic patients at 1 year. (a) Mean score at discharge in asymptomatic (blue) vs symptomatic (orange) patients at 1 year. (b) Mean score at 4 months in asymptomatic (blue) vs symptomatic (orange) patients at 1 year. (c) Mean score at 1 year in asymptomatic (blue) vs symptomatic (orange) patients at 1 year.
Regarding utilization of rehabilitation services, at the 4-month follow-up only 4.3% of the study participants had been assessed by a rehabilitation specialist, while at the 1-year mark, the percentage rose slightly to 10.9%. Even among the symptomatic group, the percentage of who reached out to rehabilitation services was scarce, and mainly included physiotherapy interventions.
Effect of age, disease severity and sex
Supplementary Table SI depicts differences among the studied subsets of patients at discharge time. Patients older than 50 years had greater difficulties walking and reported more taste and/or olfactory disorders compared to patients younger than 50 years. Patients with severe or critical disease had more fatigue, resting and exertional dyspnoea, walking difficulties, stress, sleep disorders and memory/concentration impairment than patients with mild or moderate disease. Mobility, self-care, usual activities and pain were more frequently reported by older patients and the subjective wellness rating was also significantly lower. Female patients had worse scores in all categories with the sole exception of swallowing difficulties.
Supplementary Table SII depicts differences among the studied subsets of patients at the first follow-up. Patients older than 50 years had greater difficulties walking, while the rest of the variables compared were similar. Patients with mild/moderate and severe/critical disease did not differ in any category. Female patients scored worse on fatigue, pain, stress, depression, sleep disorders, memory/concentration impairment, anxiety, as well as their subjective health rating.
Supplementary Table SIII depicts differences among the studied subsets of patients at the second follow-up. Patients older than 50 years had more fatigue and more mobility problems compared to patients younger than 50 years. Patients with severe/critical disease only reported more difficulties walking than patients with mild/moderate disease. Female patients still reported greater fatigue, pain, stress, depression, sleep disorders and memory/concentration impairment levels. Furthermore, they again scored worse on mobility, usual activity, anxiety as well as subjective wellness scale levels.
Finally, Table III depicts the number and percentage of patients that seeked rehabilitation services at the two time points of the study, as well as the type of discipline they opted for. The percentage of participants reaching out to rehabilitation specialists was extremely poor, both within the asymptomatic as well as within the symptomatic groups of patients.
DISCUSSION
To our knowledge, this is the first Greek study reporting on the longer-term effects of COVID-19 pneumonia on hospitalized patients, as well as their knowledge and utilization of post-COVID-19 condition facilities and rehabilitation services in the Greek region. Recently, there has been an ever-expanding array of medical research focusing on post-COVID-19 condition symptomatology, with estimates of 31%–69% COVID-19 pneumonia patients suffering from the syndrome (13) and clinical findings including fatigue, muscle pain, cardiac complications, dyspnoea at rest and/or exertion, anxiety and stress or depression (14). However, evaluation and management of the syndrome still remains extremely challenging in the medical setting and requires a multidisciplinary approach by different specialists and scientific guidelines based on each individual’s needs (15–17).
In a much larger Chinese study (5), patients of a similar age group to ours who were evaluated after COVID-19 hospitalization based on the EQ 5D-5L questionnaire reported similar symptoms, on the one hand, but quite lower subjective assessment scores than the Greek patients, a difference that may partially be explained by differences on disease severity, as a higher proportion of Chinese patients presented with severe/critical disease and required ICU management. Indeed, our study confirmed disease severity as a predictor for worse post-COVID symptomatology and EQ 5D-5L scoring, along with older age and female sex.
The second leg of our study focused on examining the very scarce field of rehabilitation services within the Athenian borders. Some countries have undeniably taken important steps in implementing rehabilitation services in the management of COVID-19 patients around the globe. Awareness was raised early on with physical medicine and rehabilitation recommendations, in an effort to minimize disability, improve QoL and ensure the quickest return to everyday life (18, 19). However, a recent large-scale nationwide study from the United States concluded that use of rehabilitation services was associated with race, although the incidence of post-COVID symptoms was no different, with black and Latino patients being underrepresented in the group of people seeking post-COVID help (20). A Latino American study revealed a heterogeneous pattern of rehabilitation provision within the region, with most of the programmes focusing on physiotherapy (21).
Another interesting concept that has to be considered from our point of view is the implementation of telemedicine and telehealth practices in the rehabilitation scheme, especially in countries with variable structures and infrastructures such as Greece. Telemedicine and telerehabilitation services in the coronavirus era can foster easier delivery of assessment and rehabilitation services across areas or patients who are difficult to reach otherwise as well as serve them from the comfort of their home while they are still in recovery (22, 23). Unfortunately, the field of telemedicine remains very much underdeveloped across Greece, a country with large parts of the population residing in rural areas that could very well benefit from it (24); however, this is an idea that could be implemented to better meet the needs of such populations.
CONCLUSION
What is more than evident is that, although the acute curve of the pandemic seems to head towards flattening, nonetheless, owing to the efficiency of the currently available vaccines and therapeutic measures, the SARS-CoV-2 virus is here to stay, with all the particularities and exceptions in its management. Considering the plethora of post-disease manifestations and sequelae, as well as the ever-growing number of people being infected worldwide, it is likely that the official end of the pandemic will leave us with a large part of the population presenting with post-COVID symptomatology, be it a simple post-infectious cough or a longer, persistent symptom. In order to better meet the needs of this population and provide efficient post-COVID status assessment and rehabilitation, our healthcare system will inevitably have to adapt and create specialist teams and outpatient or even at-home settings. We believe a holistic approach of the syndrome, from the moment of discharge and up to later stages of patient follow-up, will lead to a smoother recovery and a shorter but safer reintroduction of post-COVID patients into their everyday lives and routines.
LIMITATIONS
Our data comes from a single centre in Athens and only includes a small number of patients, compromising the generalizability of the results. Furthermore, comparison of symptom occurrence along the 3 time points may be compromised by the physiological process of ageing or advances in the participants’ comorbidities. Finally, a selection bias might exist, as patients unable to return for any reason to the follow-up visits (for example, if a patient is hospitalized or bedridden in the meantime) were inevitably lost and not included in the participating population.
ACKNOWLEDGEMENTS
We thank all doctors who contributed to data collection, as well as all patients who participated in this study.
Authors’ contributions
AK: conceptualization and design, data collection. NK: data analysis, first draft and corrections.
All authors read and approved the final manuscript.
Availability of data and materials
The datasets used and/or analysed during this study are available from the corresponding author upon request.
Declarations
Patients or their proxies signed a written informed consent to participate in the study. The study protocol was approved by the 401 General Military Hospital of Athens Ethics and Bioethics Committee.
Disclosure statement
The authors have declared no conflicts of interest.
REFERENCES
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382(8): 727–733. https://doi.org/10.1056/nejmoa2001017
- Coronavirus disease (COVID-19) situation reports [Internet]. Who.int [cited 2022 Nov 23]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ 2020; 370: m3026. https://doi.org/10.1136/bmj.m3026
- Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, Petraroli A, et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res 2020; 48(8): 030006052094838. https://doi.org/10.1177/0300060520948382
- Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021; 397(10270): 220–232. https://doi.org/10.1016/s0140-6736(20)32656-8
- Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open 2021; 4(2): e210830. https://doi.org/10.1001/jamanetworkopen.2021.0830
- Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens 2022; 11(2): 269. https://doi.org/10.3390/pathogens11020269
- Agostini F, Mangone M, Ruiu P, Paolucci T, Santilli V, Bernetti A. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med 2021; 53(1): jrm00141. https://doi.org/10.2340/16501977-2776
- Greece [Internet]. Who.int. [cited 2022 Nov 23]. Available from: https://www.who.int/countries/grc
- Giannopoulou I, Tsobanoglou GO. COVID-19 pandemic: challenges and opportunities for the Greek health care system. Irish J Psychol Med 2020; 37(3): 226–230. https://doi.org/10.1017/ipm.2020.35
- Dimitriadis V, Kousoulis AA, Markaki A, Sgantzos MN, Hadjipavlou A, Lionis C. Quality assessment systems in rehabilitation services for people with a disability in Greece: a critical review. Disabil Health J 2013; 6(3): 157–164. https://doi.org/10.1016/j.dhjo.2013.01.005
- Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011; 20(10): 1727–1736. https://doi.org/10.1007/s11136-011-9903-x
- Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-Coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis 2022; 226(9): 1593–1607. https://doi.org/10.1093/infdis/jiac136
- Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021; 38(101019): 101019. https://doi.org/10.1016/j.eclinm.2021.101019
- Koc HC, Xiao J, Liu W, Li Y, Chen G. Long COVID and its management. Int J Biol Sci 2022; 18(12): 4768–4780. https://doi.org/10.7150/ijbs.75056
- Nurek M, Rayner C, Freyer A, Taylor S, Järte L, MacDermott N, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. Br J Gen Pract 2021; 71(712): e815–e825. https://doi.org/10.3399/BJGP.2021.0265
- Negrini S, Borg K, Cusick A, Ferriero G, Frontera WR, Gross DP, et al. Global statements to produce and implement evidence in the post-COVID-era provide a path forward for rehabilitation – A joint initiative of Cochrane Rehabilitation and the leading journals in the field. J Rehabil Med 2022; 54: jrm00345. https://doi.org/10.2340/jrm.v54.4858
- Wang TJ, Chau B, Lui M, Lam G-T, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil 2020; 99(9): 769–774. https://doi.org/10.1097/phm.0000000000001505
- Barker-Davies RM, O’Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 2020; 54(16): 949–959. https://doi.org/10.1136/bjsports-2020-102596
- Hentschel CB, Abramoff BA, Dillingham TR, Pezzin LE. Race, ethnicity, and utilization of outpatient rehabilitation for treatment of post COVID-19 condition. PM&R 2022; 14(11): 1315–1324. https://doi.org/10.1002/pmrj.12869
- Benavides-Cordoba V, Barros-Poblete M, Vieira RP, Mazzucco G, Fregonezi G, Torres-Castro R. Provision of pulmonary rehabilitation in Latin America 18 months after the COVID-19 pandemic: a survey of the Latin American Thoracic Association. Chron Respir Dis 2022; 19: 147997312211041. https://doi.org/10.1177/14799731221104102
- Falvey JR, Ferrante LE. Flattening the disability curve: rehabilitation and recovery after COVID-19 infection. Heart Lung 2020; 49(5): 440–441. https://doi.org/10.1016/j.hrtlng.2020.05.001
- Kim SY, Daley K, Pruski AD, AlFarra T, Azola A, Gonzalez Fernandez M, et al. Implementation of a framework for telerehabilitation in clinical care across the continuum during COVID-19 and beyond. Am J Phys Med Rehabil 2022; 101(1): 53–60. https://doi.org/10.1097/phm.0000000000001904
- Tsirintani M. Strategic procedures and revisions for implementing telemedicine and telecare in Greece. Appl Clin Inform 2012; 03(01): 14–23. https://doi.org/10.4338/aci-2011-08-r-0048