SHORT COMMUNICATION
FEASIBILITY OF INSPIRATORY MUSCLE TRAINING FOR PATIENTS WITH PERSISTENT DYSPNOEA AFTER COVID-19 INFECTION: A PILOT STUDY
Romain COLLET, MSc1, Maarten VAN EGMOND, PhD1,2,3, Marike VAN DER SCHAAF, PhD2,4,5 and Mel MAJOR, PhD1,2,
From the 1Faculty of Health, Department of Physical Therapy, Amsterdam University of Applied Sciences, 2Faculty of Health, Center of Expertise Urban Vitality, Amsterdam University of Applied Sciences, 3Faculty of Health, European School of Physiotherapy, Amsterdam University of Applied Sciences, 4Amsterdam UMC location University of Amsterdam, Rehabilitation Medicine, Meibergdreef 9 and 5Amsterdam Movement Sciences, Ageing and Vitality, Amsterdam, The Netherlands
Objective: This study investigates the feasibility of delivering inspiratory muscle training as part of the physical therapy treatment for patients with post-COVID dyspnoea.
Design: Mixed-methods pilot study.
Subjects/patients: Patients with complaints of dyspnoea after COVID-19 infection and their physical therapists.
Methods: The Amsterdam University of Applied Sciences and the Amsterdam University Medical Centers conducted this study. Participants performed daily inspiratory muscle training at home for 6 weeks, consisting of 30 repetitions against a pre-set resistance. The primary outcome was feasibility assessed as acceptability, safety, adherence and patient- and professional experience obtained through diaries and semi-structured interviews. The secondary outcome was maximal inspiratory pressure.
Results: Sixteen patients participated. Nine patients and 2 physical therapists partook in semi-structured interviews. Two patients dropped out before initiating the training. Adherence was 73.7%, and no adverse events occurred. Protocol deviations occurred in 29.7% of the sessions. Maximal inspiratory pressure changed from 84.7% of predicted at baseline to 111.3% at follow-up. Qualitative analysis identified barriers to training: ‘Getting acquainted with the training material’ and ‘Finding the right schedule’. Facilitators were: ‘Support from physical therapists’ and ‘Experiencing improvements’.
Conclusion: Delivering inspiratory muscle training to patients with post-COVID dyspnoea seems feasible. Patients valued the simplicity of the intervention and reported perceived improvements. However, the intervention should be carefully supervised, and training parameters adjusted to individual needs and capacity.
LAY ABSTRACT
Many people who have recovered from a COVID-19 infection develop persistent shortness of breath, fatigue and difficulties with memories, learning new things or making decisions. This condition affects their daily life and is called post-COVID syndrome. Inspiratory muscle training is a technique that aims to help people to breathe more easily by strengthening and improving the coordination of breathing muscles. We undertook this study to determine if performing such training was possible for these patients. We interviewed 2 physiotherapists who provided the training and 9 of their patients. In addition, we looked into the diaries 16 patients kept about their training to learn about their experiences or unexpected (medical) problems they might have had with the training. We found that the training seemed reasonable since patients and their physiotherapists found it simple, and no negative experiences happened. However, patients said it helped if the physiotherapist supervised them during the training.
Key words: COVID-19; dyspnoea; maximal inspiratory pressures; physical therapy modalities.
Citation: JRM-CC 2023; 6: jrmcc6507. DOI: https://doi.org/10.2340/jrmcc.v6.6507
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: May 9, 2023; Published: June 5, 2023
Correspondence address: Mel Major, Department of Physical Therapy, Faculty of Health, Amsterdam University of Applied Sciences, Tafelbergweg 51, Postbus 2120 1000 CC Amsterdam, The Netherlands. E-mail: m.major@hva.nl
Competing interests and funding: The authors have no conflicts of interest to declare.
Patients recovering from coronavirus disease 2019 (COVID-19) often experience prolonged symptoms such as dyspnoea, fatigue, cognitive impairment and exercise intolerance, collectively known as post-COVID syndrome (1, 2). Dyspnoea is one of the most debilitating symptoms of post-COVID syndrome, associated with poorer quality of life (QoL) and potentially caused by an autonomic dysfunction resulting in impaired breathing coordination and hyperventilation (3, 4).
Inspiratory muscle training (IMT) effectively decreases dyspnoea in patients with chronic obstructive pulmonary disease and in patients who have undergone abdominal or thoracic surgery and can potentially improve autonomic control (5–7). In addition, a recent study evaluating the effects of IMT in patients recovering from COVID-19 found that IMT could reduce dyspnoea in these patients (8). During IMT, the individual breathes through a hand-held device, restricting airflow to stimulate and strengthen inspiratory muscles. Such training can be performed independently at home. Furthermore, home-based exercise training programs have been shown to improve health outcomes in other respiratory conditions and offer people for whom traveling to a rehabilitation centre or physical therapy (PT) practice is difficult the possibility to rehabilitate from home (9–11).
In the Netherlands, the Royal Dutch Society for Physiotherapy (KNGF) recommends IMT as part of the treatment for patients with persistent dyspnoea after COVID-19. However, for COVID treatment guidelines, data on the feasibility of IMT and recommendations for frequency and intensity of the training are lacking. Therefore, this study investigated the feasibility of a home-based IMT training protocol as part of the COVID-19 PT program.
METHODS
The Amsterdam University of Applied Sciences and the Amsterdam University Medical Centers (AUMC, location AMC) conducted a mixed-method pilot study in collaboration with a primary care PT clinic delivering post-COVID rehabilitation interventions according to Dutch clinical practice recommendations. The Medical Ethics Committee of the AUMC provided a waiver for this study (METC W21_373 #21.413).
Patients and their PTs were participants in this study. Patients were eligible if they: (i) had dyspnoea, assessed by PTs with the Medical Research Council dyspnoea scale (12) as one of the main complaints of post-COVID syndrome, (ii) were 18 years or older and (iii) were able to communicate in Dutch or English. Eligible patients were informed of the study by the PTs and contacted by the researchers if they provided consent for participation.
Intervention
IMT was performed with the Powerbreathe© Medic, a threshold IMT device manufactured by POWERbreathe International Limited. The intervention followed a protocol similar to the one used in a published trial investigating the effect of IMT on respiratory muscle strength after lung cancer surgery (13). Patients were seated upright with relaxed shoulders and feet flat on the ground and performed 30 inhalations against a pre-set resistance once daily (Fig. 1). PTs regularly reviewed the performance of the patients and could adjust the protocol if they deemed it necessary. The starting intensity was set at 30% of the maximal inspiratory pressure (MIP) and could be modified per the PT’s instruction. Patients performed the training at home for 6 weeks. All patients received additional weekly PT interventions aimed at increasing exercise capacity.
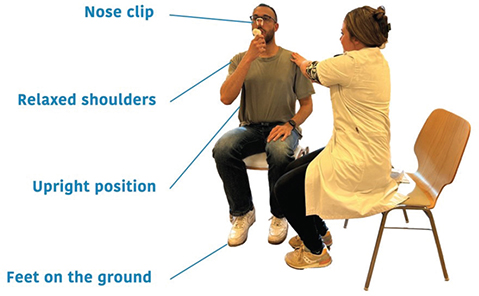
Fig. 1. Picture illustrating the correct use of the Powerbreathe©.
Data collection
Data on the primary outcome – feasibility – assessed as acceptability, safety, adherence and patient- and professional experience were retrospectively collected through patient-reported information from anonymized diaries and (telephonic) interviews. Data on the primary outcome were collected after the 6-week intervention was completed due to the retrospective character of our study. Patient diaries included data on the total number of completed sessions, repetitions per session and reasons for protocol deviations. Secondary outcome data were obtained with voluntary MIP measurements using MicroRPM™, according to the protocol from a recently published study investigating the course of recovery of respiratory muscle strength among survivors of critical illness (14). The maximum of 3 MIP measurements was recorded twice: before the start of the training and after 6 weeks. In addition, the patient’s age, gender, date of first COVID-19 infection, hospital and ICU length of stay (LOS), duration of mechanical ventilation or non-invasive oxygen therapy and medical history were retrieved from the electronic PT files.
Semi-structured interviews were conducted telephonically or at the PT clinic. Separate topic guides were developed for patient and PT interviews. Topics included: (i) previous and recent experience with IMT and the training equipment, (ii) perceived effect of the training, (iii) role of the PT and (iv) recommendations for improvements (supplemental file). The research assistants who performed the interviews were unknown to the patients. Interviews were audio recorded, transcribed verbatim and anonymized.
Data analysis
We used IBM SPSS version 28 and NVIVO 2022 for quantitative and qualitative data analysis, respectively (15, 16).
Quantitative data
Patient demographic and medical data, the number of completed IMT sessions and the number and nature of protocol deviations were summarized and reported in percentages. First, MIP outcomes were reported in medians and interquartile ranges (IQR). Next, individual MIP values were converted into a percentage of predictive values, adjusted for age and gender (17).
Qualitative data
A phenomenological approach was chosen to capture the essence of patients’ and PTs’ experiences regarding barriers and facilitators related to the IMT protocol. Interview transcriptions were coded line-by-line and organized in a code list. Meaningful categories were determined from the code list and discussed in 2 reflexivity meetings to identify themes (18).
RESULTS
Population characteristics
Two PTs (1 male and 1 female) participated in an interview. Sixteen patients (female: 75% with a median (IQR) age of 51 (19.5) received the intervention and 9 patients (56.3%) were interviewed (Fig. 2). Four participants (25%) received COVID-19 treatment while being admitted to a hospital, including 1 patient (6.3%) who stayed 14 days in the ICU with mechanical ventilation for 5 days. Hospital LOS ranged from 5 to 30 days (median [IQR] 5 [18.8]). Five participants (31%) received non-invasive oxygen therapy for 2–10 days (median [IQR] 4 [4.5]) (Table I).
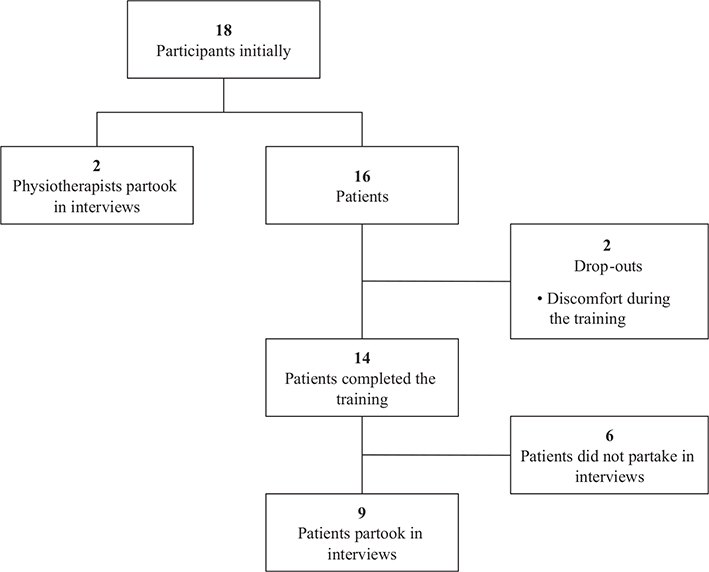
Fig. 2. Flowchart illustrating participant inclusion.
Adherence, protocol deviations and safety
Two participants (12.5%) discontinued the IMT in the first week due to discomfort experienced during training. No adverse events related to the IMT were observed (Table II).
Participants completed 495 out of a potential 672 sessions of IMT, corresponding to a protocol adherence of 73.7%. Reasons for non-adherence were perceived discomfort with the Powerbreathe©, fatigue, illness, being away from home or forgetting to do the training. Protocol deviations were observed in 29.7% (SD±33.4%) of the performed sessions and consisted of performing IMT more than once a day (n = 3, 18.8%) or not being able to reach 30 repetitions in a single set (n = 7, 43.8%). In the latter case, the PTs adjusted the protocol to 3 sets of 10 or 2 sets of 15 repetitions, dependent on the patient’s capacity.
Maximal inspiratory pressure
Baseline and follow-up data on MIP were obtained from 14 patients (87.5%). When compared to normative values, the median (IQR) MIP was 84.7% (34%) at baseline and increased to 111.3% (66%) 6 weeks later.
The following barriers and facilitators to compliance with the protocol (Fig. 3) were identified from qualitative analysis:
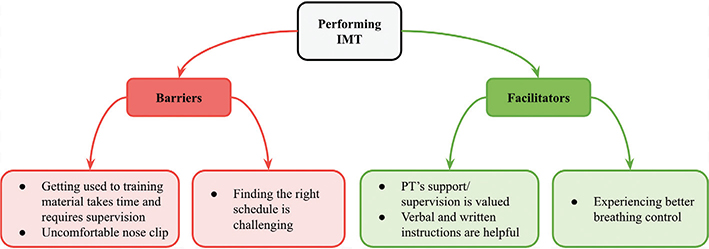
Fig. 3. Qualitative analysis – Barriers and facilitators identified
Barriers: getting acquainted with the training material and finding the right schedule
Participants were satisfied with the device as they described it as user-friendly, safe and easy to use. However, the nose clip was found to be uncomfortable. Participants mentioned that it took time to become acquainted with the training material and experienced that their PTs had to correct them frequently. PTs also acknowledged the importance of (initial) supervision of the IMT regime to apply corrections when necessary (Table III). Establishing a daily routine to perform the training was challenging, especially in the beginning. As a result, some participants forgot training sessions or chose to train 2–3 times a day. Ultimately, all participants managed to integrate IMT into their daily routines.
Facilitators: support from PTs and experiencing improvements
During the entire duration of the intervention, participants felt supported by their PTs. They particularly valued the verbal and written instructions they received at the start of the training and indicated that professional advice was needed to find the correct training intensity. Patients mentioned that throughout the weeks, they achieved independence in the IMT. PTs agreed with the importance of instructions on the correct device usage and regular supervision during the first weeks of the training. Both patients and PTs suggested that an instructional video might facilitate the correct utilization of the Powerbreathe©.
Experiencing improvement, observed by being able to increase the resistance on the device, was perceived as highly motivating to patients. Additionally, some participants perceived easier breathing during their PT program or independent training such as running or walking. PTs confirmed that patients developed better breathing control throughout the IMT program.
DISCUSSION
IMT seems feasible and has the potential to facilitate the rehabilitation of patients suffering from persistent dyspnoea after COVID-19. Patients and PTs perceived improvements in breathing control, suggesting a relationship between IMT and decreased symptoms of dyspnoea. These findings are consistent with a recent publication indicating that IMT might reduce dyspnoea and represent an essential home-based intervention as part of COVID-19 rehabilitative strategies (19). Yet, further research is needed to investigate potential relationships between IMT and improved outcomes for patients with persistent dyspnoea after COVID-19.
Though IMT seems feasible, PT supervision is essential, as 12.5% of the participants experienced discomfort with the intervention and needed assistance. In addition, the training protocol we used primarily targeted muscle endurance and coordination, as the number of repetitions was high and the training load was relatively low. Our findings suggest, however, that adjustment and individualization of the IMT protocol are needed, as 44% of our participants could not manage 30 repetitions at 30% of their MIP without rest intervals.
A qualitative study examining the perceptions of patients recovering from COVID-19 on IMT also found that the training needed individualization as it was challenging for patients experiencing fatigue due to their condition (20). Together with our findings, this implies that post-COVID syndrome is a complex condition involving various symptoms that must be recognized and considered when delivering IMT as a home-based intervention. Furthermore, another recent trial found that combining IMT with manual diaphragm release was more effective than IMT alone in reducing dyspnoea (21). Therefore, an investigation of the optimal delivery mode of IMT, including dose, intensity and training components among patients with post-COVID dyspnoea, is required.
Limitations
Feasibility data were retrospectively collected through patient-reported information, potentially impacting the reliability of reported results on adherence. Additionally, important contextual information such as pre-COVID functioning, co-morbidities or previous experience with IMT is lacking. Finally, retrieving data on baseline and follow-up measurements of dyspnoea and correlating the IMT with the improvement of dyspnoea might have provided further insights into the feasibility of the training.
CONCLUSION
This pilot study shows that IMT seems feasible for patients with persistent dyspnoea after COVID, as long as it is performed under the supervision and integrated into a PT program. While evidence on optimal training parameters for IMT among this population is lacking, this short communication provides recommendations for implementing IMT in clinical practice and directions for further research.
ACKNOWLEDGMENTS
Brenda Pronk and Caspar Hattink, who provided the physical therapy training during this pilot study, are acknowledged for their valuable contribution. Hanna van Gerven and Lucia Jonova are acknowledged for their support in conducting and transcribing telephonic interviews.
REFERENCES
- Cabrera Martimbianco AL, Pacheco RL, Bagattini ÂM, Riera R. Frequency, signs and symptoms, and criteria adopted for long COVID- 19: a systematic review. Int J Clin Prac 2021; 75: e14357. https://doi.org/10.1111/ijcp.14357
- Centers for Disease Control and Prevention. Post-COVID conditions: overview for healthcare providers [homepage on the Internet]. 2021 [cited 2022 Sep 01]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020; 34: 101623. https://doi.org/10.1016/j.tmaid.2020.101623
- Wirth KJ, Scheibenbogen C. Dyspnea in post-COVID syndrome following mild acute COVID-19 infections: potential causes and consequences for a therapeutic approach. Medicina 2022; 58: 419. https://doi.org/10.3390/medicina58030419
- de Abreu RM, Rehder-Santos P, Minatel V, Dos Santos GL, Catai AM. Effects of inspiratory muscle training on cardiovascular autonomic control: a systematic review. Autonom Neurosci 2017; 208: 29–35. https://doi.org/10.1016/j.autneu.2017.09.002
- Mans CM, Reeve JC, Elkins MR. Postoperative outcomes following preoperative inspiratory muscle training in patients undergoing cardiothoracic or upper abdominal surgery: a systematic review and meta analysis. Clin Rehabil 2015; 29: 426–438. https://doi.org/10.1177/0269215514545350
- Neves LF, Reis MH, Plentz RD, Matte DL, Coronel CC, Sbruzzi G. Expiratory and expiratory plus inspiratory muscle training improves respiratory muscle strength in subjects with COPD: systematic review. Respir Care 2014; 59: 1381–1388. https://doi.org/10.4187/respcare.02793
- Abodonya AM, Abdelbasset WK, Awad EA, Elalfy IE, Salem HA, Elsayed SH. Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: a pilot control clinical study. Medicine 2021; 100: 25339. https://doi.org/10.1097/MD.0000000000025339
- Lu Y, Li P, Li N, Wang Z, Li J, Liu X, et al. Effects of home-based breathing exercises in subjects with COPD. Respir Care 2020; 65: 377–387.
- Uzzaman MN, Agarwal D, Chan SC, Engkasan JP, Habib GM, Hanafi NS, et al. Effectiveness of home-based pulmonary rehabilitation: systematic review and meta-analysis. Eur Respir Rev 2022; 31: 220076. https://doi.org/10.4187/respcare.07121
- Wuytack F, Devane D, Stovold E, McDonnell M, Casey M, McDonnell TJ, et al. Comparison of outpatient and home-based exercise training programmes for COPD: a systematic review and meta- analysis. Respirology 2018; 23: 272–283. https://doi.org/10.1111/resp.13224
- Fletcher C. Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis (MRC breathlessness score). BMJ 1960; 2: 1665.
- Brocki BC, Andreasen JJ, Langer D, Souza DSR, Westerdahl E. Postoperative inspiratory muscle training in addition to breathing exercises and early mobilization improves oxygenation in high-risk patients after lung cancer surgery: a randomized controlled trial. Eur J Cardio-Thor Surg 2015; 49: 1483–1491. https://doi.org/10.1093/ejcts/ezv359
- Major M, van Egmond M, Dettling-Ihnenfeldt D, Ramaekers S, Engelbert R, van der Schaaf M. Course of recovery of respiratory muscle strength and its associations with exercise capacity and handgrip strength: a prospective cohort study among survivors of critical illness. PLoS One 2023; 18: e0284097. https://doi.org/10.1371/journal.pone.0284097
- IBM SPSS Statistics for Macintosh, Version 28.0.; 2021; Armonk, NY: IBM Corp; 2021.
- NVivo. QSR International Pty Ltd. 2020. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care 2009; 54: 1348–1359.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. https://doi.org/10.1186/1471-2288-8-45
- McNarry MA, Berg RMG, Shelley J, Hudson J, Saynor ZL, Duckers J, et al. Inspiratory muscle training enhances recovery post COVID-19: a randomised controlled trial. Eur Respir J 2022; 60: 2103101. https://doi.org/10.1183/13993003.03101-2021
- Shelley J, Hudson J, Mackintosh KA, Saynor ZL, Duckers J, Lewis K, et al. Perceptions of inspiratory muscle training in adults recovering from COVID-19. PLoS One 2022; 17: e0270620. https://doi.org/10.1371/journal.pone.0270620
- Nagy EN, Elimy DA, Ali AY, Ezzelregal HG, Elsayed MM. Influence of manual diaphragm release technique combined with inspiratory muscle training on selected persistent symptoms in men with post-Covid-19 syndrome: a randomized controlled trial. J Rehabil Med 2022; 54: jrm00330-jrm. https://doi.org/10.2340/jrm.v54.3972