ORIGINAL REPORT
CLINICAL AND HEALTHCARE IMPACTS OF PORTABLE ULTRASONOGRAPHY IN AMBULATORY CARE MUSCULOSKELETAL REHABILITATION CONSULTATIONS
Jose M. DE LA LAMA, MD, MBA, PHD1, Manuel MORALES, MD2, Juan DE NICOLAS, MD2, Andrea UCIN, MD2 and Antonio GALVAN, MD2
From the 1Physical Medicine and Rehabilitation Service, Internal Medicine Department, La Merced Hospital, Osuna, Spain, 2Physical Medicine and Rehabilitation Service, Virgen del Rocio University Hospital, Sevilla, Spain
Objective: We evaluated the impact of Point-of-care ultrasound (POCUS) in musculoskeletal consultations out of hospital using a Philips Lumify portable ultrasound device. We aimed to determine the impact of POCUS on the number of hospital referrals for injections as well as on the number of injections performed in consultation.
Design: Retrospective case study comparing 2 periods: June to September 2021 (pre-POCUS) and November 2021 to February 2022 (POCUS). Statistical comparisons were performed using the χ2. In both periods, 21 medical consultations were performed. In the pre-POCUS period, 470 patients were assessed, with an average of 1.29 hospital referrals made per day of consultation for hospital injections and an average of 2.05 injections performed per day of medical consultation. In the POCUS period, 589 patients were assessed, with an average of 0.1 hospital referrals per day (−92.6%; p < 0.00001) and an average of 2.76 injections performed per day (+34.9%; p < 0.00001). The introduction of POCUS at our practice reduced the number of hospital referrals made for injections and increased the number of injections performed every day of consultation.
Conclusion: This suggests that POCUS is of great clinical value in out-of-hospital musculoskeletal rehabilitation consultations.
Lay Abstract
This study provides insight into the clinical impact of portable ultrasound in rehabilitation consultations performed out of the Hospital in a Primary care center. The aims of this study are to measure the number of hospital referrals for therapeutic injections as well as on the number of injections performed in every consultation. In this study, 2 periods were compared. It was found that the introduction of POCUS at our practice reduced the number of hospital referrals to perform challenging injections and increased the number of injections performed during consultations. Portable ultrasound appears to be of clinical value in musculoskeletal rehabilitation consultations performed out of hospital settings.
Key words: access to health services; musculoskeletal diseases; rehabilitation; ultrasonography; injections; value-based healthcare.
Citation: JRM-CC 2023; 6: jrmcc6573. DOI: https://doi.org/10.2340/jrmcc.v6.6573
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Aug 15, 2023; Published: Sep 13, 2023
Correspondence address: Jose M. De la Lama, Physical Medicine and Rehabilitation Service, La Merced Hospital, Osuna, Spain (41640). E-mail: josem.lama.sspa@juntadeandalucia.es
Competing interests and funding: The authors have no conflicts of interest to declare.
Physician-led point-of-care ultrasound (POCUS) is increasingly used to evaluate patients with musculoskeletal conditions. POCUS helps to accurately diagnose musculoskeletal pathologies, complements the physical examination, and ensures that injections are performed in a timely and safe manner.
In 2022, over half of all medical schools in the United States included POCUS training in their undergraduate curricula (1). Many medical specialties have formal ultrasound training programs. The use of musculoskeletal POCUS is especially useful in emergency services. A systematic review evaluating POCUS for the diagnosis of skull fractures in children showed a sensitivity of 91%, specificity of 96%, positive predictive value of 88%, and negative predictive value of 97% (2). A prospective cross-sectional study analyzed the accuracy of POCUS in the diagnosis of suspected ligamentous injuries in the wrist, using magnetic resonance imaging as the gold standard (3). Results showed POCUS had a high sensitivity (97–99%), specificity (97%), and accuracy (97–98%).
Furthermore, in a meta-analysis of 7 studies of the use of POCUS in patients with shoulder dislocations (n = 739), POCUS showed 99% sensitivity and specificity versus X-ray imaging (4). In a meta-analysis of ultrasound for elbow fracture diagnosis, a sub-group analysis of 5 studies showed that ultrasound had a specificity of 95% and sensitivity of 94% (5). Finally, in a case series published in 2020, the authors defended the use of POCUS to confirm joint effusion in patients with suspected septic arthritis of the hip, despite non-confirmatory plain X-rays (6).
The adaptability and potential impact of POCUS have also been demonstrated in accidents outside-of-hospital. It has been reported that POCUS analgesic blocks prior to hospital transfer avoid the requirement for analgesic drugs and improve logistics (7). However, we consider that one of the difficulties to accelerate the implementation of new technology is the lack of standard methodology to assess the impact on patient outcomes and clinical processes.
This study aimed to determine the potential capability of POCUS to reduce the need for hospital referrals for challenging injections, to increase the number of injections performed during consultation, and to use it as a diagnostic tool.
METHODS
This was a retrospective case study of patients with musculoskeletal symptoms who were evaluated in a rehabilitation consultation over a period of 4 months (November 2021 to February 2022). POCUS was performed by 2 physical medicine and rehabilitation specialists trained in the use of musculoskeletal ultrasound (1 with 4 years and another with 15 years of US training) according to their own clinical criteria. The specialists visited patients directly at 2 primary care centers in Tomares and Castilleja de la Cuesta (Seville, Spain) instead of visiting patients in a tertiary referral hospital (Virgen del Rocio Hospital). Patients were referred by their primary care doctors and were evaluated directly in the primary care center to reduce waiting lists and hospital visits. Typical agenda was usually 20 to 25 patients per day. If necessary, diagnostic tests were ordered by the rehabilitation specialist and therapeutic injections were performed using anatomical landmark. However, if injection was considered technically too challenging, it was not performed during the consultation and patients were referred to the tertiary referral hospital for an ultrasound-guided injection.
In November 2021, we started using a portable ultrasound system (Philips Lumify L12-4 high-resolution linear transducer), with a frequency range of 12 to 4 MHz. The portable ultrasound system was connected to a smartphone or tablet via a MicroB-type USB transducer (Fig. 1). The cost of this device was estimated to be a quarter of that of conventional equipment. Moreover, the device is easy and intuitive to use.

Fig. 1. Injection Performed in Consultation under US Guidance. Red arrow points smartphone connected to Ultrasound. Written informed consent was obtained.
We classified the main uses and anatomical sites after use of POCUS for diagnosis and treatment. As a control group, we analyzed the consultations during the 4 months prior to the introduction of the portable ultrasound device (June 2021 to September 2022), recording the number of patients evaluated, the injections performed immediately during the consultations, and the number of patients referred to the hospital for ultrasound-guided injections. The data were analyzed using SPSS statistical software version 22.0 (Statistical Package for Social Sciences, IBM Corp, Armonk, NY, USA). The χ2 test for a 2 × 2 contingency table, including Yates’s correction for continuity, was performed for comparison and the data multiplied by 100 to enable data presentation as positive integers.
Finally, a novel ratio, the number needed to scan (NNS) was calculated, which is equivalent to the number needed to treat in clinical drug trials (number of patients that need to receive a treatment to observe a relevant clinical result). It would be equivalent to the number of patients we need to scan to change attitude once. NNS is calculated as the inverse of the absolute risk reduction (ARR). Therefore, NNS = 1/ARR (8).
RESULTS
In the POCUS period, 589 patients were evaluated during 21 consultations. In the pre-POCUS period, 470 patients were evaluated during 21 consultations (Table I).
Comparison of the pre-POCUS and POCUS periods showed a reduced number of referrals to the Rehabilitation Service of the tertiary referral center for injections, from 1.29 to 0.1 referrals per consultation (−92.6%). An increase in the number of injections during consultation, from 2.05 to 2.76 (+34.9%), was also shown.
For diagnosis, an ultrasound study was performed on 42 patients for a first-time diagnostic study (92.9%) and follow-up (7.1%). Among them, in 16 cases, an initial diagnostic ultrasound was performed before the clinician performed an ultrasound-guided injection during the same visit. Based on our data, we calculated the ARR as 0.38 (16 patients divided by 42 total diagnostic ultrasounds); therefore, the NNS would be 3 patients (NNS = 1/0.38 = 2.62), meaning we must perform 3 ultrasound studies to change the clinical plan once.
The most commonly studied symptomatic locations using POCUS were the shoulder (n = 19; 45.2%), ankle (n = 4; 10.8%), foot (n = 4; 10.8%), hip and knee (n = 3; 8.1%), and other (n = 10; 2%).
Regarding therapeutic use, the most frequent injection sites were shoulder (n = 26; 44.4%), interfascial (n = 7; 12.1%), trochanter (n = 6; 10.3%), knee (n = 5; 8.6%), wrist & hand (n = 5; 8.6%), and others (n = 10; 16%). The 27 shoulder injections were divided as follows: subacromial-subdeltoid (n = 14; 53.8%); periarticular (n = 6; 23.1%); intra-articular (n = 4; 15.4%) and suprascapular nerve blocks (n = 2; 7.7%).
By using a 2 × 2 contingency table, the χ2 statistic was 110.7854 (p < 0.001); with Yates’s correction for continuity (assuming that the discrete probabilities of frequencies could be approximated to a continuous distribution), the χ2 statistic was 108.75 (p < 0.001). Sensitivity analysis showed that even with a 11% reduction of referrals, the comparison between both periods was statistically significant.
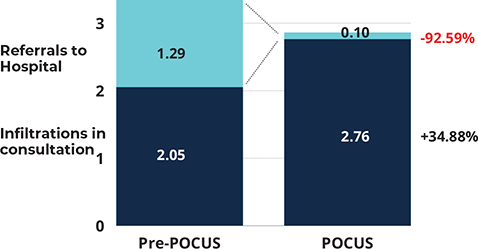
Fig. 2. Infiltrations and referrals per day.
Analyzing per anatomical target, the injections sites that increased more with POCUS were interfascial (from 0 to 12.07%), trochanter (from 2.33 to 10.34%) and wrist & hand (from 13.95 to 15.25%). All these 3 locations were considered easier to execute under US or, in the interfascial case, not recommended to be performed without POCUS.
In POCUS period, only 2 patients were referred to the hospital for injections, 1 with back pain requiring a lumbar medial branch block (a technique that could not be performed in the primary care environment) and another with shoulder pain requiring a suprascapular nerve block associated with an axillary nerve block (a hospital setting was preferred based on the patient’s characteristics for safety reasons).
DISCUSSION
Based on these results, we observed that the use of a portable ultrasound device is linked with a significantly reduced number of referrals to the tertiary referral hospital and an increased number of injections performed in the consultation. Both results might justify the use of POCUS, either as a tool to increase productivity and also to reduce hospital referrals for injections that could not be performed in consultation for technical or safety reasons.
Avoiding hospital referrals is relevant from a clinical and social point of view. First, the need to defer a necessary invasive technique is solved, reducing any delay in recovery or inclusion for physiotherapy treatment. Second, making a new appointment for the patient at the tertiary referral hospital is an inconvenience, both for the patient and accompanying family member in many cases. Finally, deferring an injection (the previous average waiting time for such cases was 1.5 months) increases the risk that the treatment will never be offered.
In addition to the rise in the number of injections in consultation, the increase of type of injections performed, such as interfascial injections must be highlighted. These injections (using a local anesthetic and a corticosteroid) are often performed to patients with myofascial neck pain; they need to be very precise and therefore are not considered safe under anatomical landmarks. Having an US opens the possibility to faster treatment of such a prevalent problem, thereby, accelerating recovery and increasing the quality of care.
Regarding the use of POCUS to avoid hospital transfers, our results are similar to those reported by a study of the medical service during a music festival with 180,000 attendees. POCUS was used in 28 of the 686 patients assessed, changing the management plan in 39% of patients and avoiding 53% of ambulance transfers (9).
We calculated that NNS would be 3 patients. This result is similar to previous studies. Tayal published a study evaluating the use of POCUS in patients presenting to the emergency department with edema and joint pain. He observed that the use of ultrasound changed the attitude in 56% of cases, equivalent to an NNS of 2 patients (10).
Overall, these study results seem positive and encouraging. Future research may analyze the clinical impact of the faster resolution of cases versus traditional care.
The limitations of this study include the short study period of 8 months and the team size of only 2 physicians. As such, it is necessary to analyze the future impact of POCUS with a greater number of professionals (with varying degrees of experience and ultrasound knowledge) in different settings.
Moreover, both the increase in total injections and the reduction in referrals were made in the context of a 25.3% increase in patients per day, which could be attributed to the pre-POCUS period covering the months of June to September. However, we did not analyze data on injections per visited patient, rather the number of injections per consultation, which is a more reliable indicator of the activity performed, and independent from the total number of visits. This limitation will be addressed in a further case study over a longer follow-up period.
Furthermore, an ultrasound procedure has an impact on the total consultation time and needs to be used with clinical judgment. Our results show this was the case, with the portable ultrasound being used for 4.1 patients per consultation, 14.6% of the total patients evaluated.
Based on the value-based approach (11), if clinicians believe in the value of new technologies, they should develop a convincing data-driven case of their benefits with concrete real-life examples and evidence. In this study, we showed the use of portable ultrasound in musculoskeletal rehabilitation.
In conclusion, our data suggest that POCUS might have a positive impact on the productivity of musculoskeletal rehabilitation consultations conducted outside hospitals. We observed that POCUS significantly reduced hospital referrals for injections, increased injections in consultation and helped to change the clinical attitude in 1 of every 3 patients.
ACKNOWLEDGEMENTS
The authors are grateful to the Tomares and Castilleja de la Cuesta Physiotherapy team for their support in the treatment of patients with musculoskeletal pathology.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- Russell FM, Zakeri B, Herbert A, Ferre RM, Leiser A, Wallach PM. The state of oint-of-care ultrasound training in undergraduate medical education: findings from a national survey. Acad Med 2022; 97: 723–727. https://doi.org/10.1097/ACM.0000000000004512
- Alexandridis G, Verschuuren EW, Rosendaal AV, Kanhai DA. Evidence base for point-of-care ultrasound (POCUS) for diagnosis of skull fractures in children: a systematic review and meta-analysis. Emerg Med J 2022; 39: 30–36. https://doi.org/10.1136/emermed-2020-209887
- Lee SH, Yun SJ. Point-of-care wrist ultrasonography in trauma patients with ulnar-sided pain and instability. Am J Emerg Med 2018; 36: 859–864. https://doi.org/10.1016/j.ajem.2018.01.005
- Gottlieb M, Holladay D, Peksa GD. Point-of-care ultrasound for the diagnosis of shoulder dislocation: a systematic review and meta-analysis. Am J Emerg Med 2019; 37: 757–761. https://doi.org/10.1016/j.ajem.2018.01.005
- Lee SH, Yun SJ. Diagnostic performance of ultrasonography for detection of pediatric elbow fracture: a meta-analysis. Ann Emerg Med 2019; 74: 493–502. https://doi.org/10.1016/j.annemergmed.2019.03.009
- Boniface K, Pyle M, Jaleesah N, Shokoohi H. Point-of-care ultrasound for the detection of hip effusion and septic arthritis in adult patients with hip pain and negative initial imaging. J Emerg Med 2020; 58: 627–631. https://doi.org/10.1016/j.jemermed.2019.11.036
- Malchow RJ. Ultrasonography for advanced regional anesthesia and acute pain management in a combat environment. US Army Med Dep J 2009; 13: 64–66. https://doi.org/10.1053/j.trap.2009.06.005
- Amini R, Patanwala AE, Shokoohi H, Adhikari S, et al. Number needed to scan: evidence-based point-of-care ultrasound (POCUS). Cureus 2021; 13: e17278. https://doi.org/10.7759/cureus.17278
- Prager R, Sedgwick C, Lund A, Kim D, Ho B, Stachura M, et al. Prospective evaluation of point-of-care ultrasound at a remote, multi-day music festival. Prehosp Disaster Med 2018; 33: 484–489. https://doi.org/10.1017/S1049023X18000821
- Tayal VS, Hasan N, Norton HJ, Tomaszewski CA. The effect of soft-tissue ultrasound on the management of cellulitis in the emergency department. Acad Emerg Med 2006; 13: 384–388. https://doi.org/10.1197/j.aem.2005.11.074
- Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Acad Med 2020; 95: 682–685.https://doi.org/10.1097/ACM.0000000000003122