ORIGINAL REPORT
COMPARISON OF SIX-MINUTE WALK TEST AND MODIFIED BRUCE TREADMILL TEST IN PAEDIATRIC PATIENTS WITH SEVERE BURNS: A CROSS-OVER STUDY
Alen PALACKIC, MD1,4, Stephanie ABAZIE, MD1, Ingrid PARRY, PT3, Soman SEN, MD3, Ronald P. MLCAK, PhD6, Jong O. LEE, MD1, David N. HERNDON, MD5, Ludwik K. BRANSKI, MD1, Steven E. WOLF, MD1,6, Heidi SPRATT, PhD2 and Oscar E. SUMAN, PhD1
From the 1Department of Surgery, 2Office of Biostatistics, Preventive Medicine and Population Health, University of Texas Medical Branch, Galveston, TX, 3University of California-Davis, Shriners Hospital for Children, Sacramento, CA, USA, 4Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Graz, Austria, 5Chief Executive Officer, Joseph Still Burn Research Foundation, Senior Editor Journal of Burn Care and Research and 6Shriners Children’s Texas, Galveston, TX, USA
Objective: To compare the six-minute walk test and the Modified Bruce treadmill test in paediatric patients with severe burns.
Subjects: A total of 67 children, aged 7–17 years, with severe burns.
Methods: Participants were assigned to perform the six-minute walk test and the Modified Bruce treadmill test in randomized order on discharge from acute burn care. Primary outcome measure was heart rate. Secondary outcome measures were distance walked, Borg’s CR-10 rate of perceived exertion, and maximal oxygen uptake (VO2).
Results: A total of 67 participants were enrolled. Thirty-eight patients completed both tests. The mean six-minute walk test maximum heart rate was 135 ± 19 bpm (range 97–180 bpm) and the mean Modified Bruce treadmill test maximum heart rate was 148 ± 24 bpm (range 100–197 bpm; p ≤ 0.05), with a weak positive correlation of R² = 0.14. The mean six-minute walk test maximum distance was 294 ± 124 m (range 55 to 522 m) while the mean Modified Bruce treadmill test maximum distance was 439 ± 181 m (range 53 to 976 m; p ≤ 0.05), with no correlation of R² = 0.006. The mean RPE CR-10 score for the six-minute walk test was 3 ± 2.5 (range 0–10) vs a mean RPE CR-10 score of 10 ± 0 for the Modified Bruce treadmill test.
Conclusion: The Modified Bruce treadmill test challenges the cardiorespiratory system significantly more than the six-minute walk test, as reflected by maximum heart rate measurements, and the perception of effort (i.e. rate of perceived exertion) by the patient. When possible, the Modified Bruce treadmill test should be used to assess cardiovascular functional capacity. However, the six-minute walk test may be more clinically feasible for use with paediatric patients with burns, and provides information about submaximal functional exercise capacity.
LAY ABSTRACT
Children with severe burns benefit from an implemented outpatient exercise rehabilitation programme. Before prescribing an aerobic exercise programme, patients should be tested in objective manner. Two common tests for these purposes are the six-minute walk test and the Modified Bruce Treadmill test. These tests have been used for measurement of the cardiopulmonary function in this population. The aim of this study was to compare these tests and the level of agreement of their responses. A total of 67 children with major burns participated in the study. Of these, 38 children completed both tests after they were treated in the acute care unit. This study showed that the treadmill test is not in agreement with the six-minute walk test in terms of heart rate. The results suggest the treadmill test should be used to assess cardiovascular functional capacity. However, the six-minute walk test may be more clinically feasible and provides information about submaximal functional exercise capacity.
Key words: burns; exercise; paediatric; rehabilitation; walk test; treadmill test.
Citation: J Rehabil Med 2022; 54: jrm00305. DOI: 10.2340/jrm.v54.1064
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jun 17, 2022; Epub ahead of print: Jul 8, 2022; Published: Oct 19, 2022
Correspondence address: Alen Palackic, Department of Surgery, University of Texas Medical Branch, 301 University Blvd, Galveston, TX 77555, USA. E-mail: alpalack@utmb.edu
Competing interests and funding: The authors have no conflicts of interest to declare.
This work was supported by the Department of Defense [W81XWH-15-1-0143, W81XWH-14-2-0160], and National Institutes of Health [R01HD049471] and The National Institute on Disability Independent Living and Rehabilitation Research (NIDILRR) [#90DPBU0003]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding sources.
Severe burns are one of the most devastating traumas, with approximately 500,000 people being admitted for burn treatment each year. Of these admissions, 30% of cases involve children under 16 years of age (1). Due to improvements in acute burn care, mortality continues to decrease, and most patients with severe burns survive. However, following survival there is persistence of weakness, fatigue, and muscle catabolism from various factors that include prolonged bed rest and inactivity during the acute care stage (2). Outpatient exercise rehabilitation programmes are considered one of the non-pharmacological approaches to mitigate the long-term effects of the burn-induced hypermetabolic stress response and weakness induced by inactivity or bed rest (3). The programmes typically consist of progressive resistance and aerobic exercises, and have been shown to maintain or increase lean body mass (LBM), exercise work capacity, cardiorespiratory function, range of motion, endurance, and strength (4–6).
Before being prescribed an aerobic exercise programme, patients should be tested in a standardized and objective manner. Two relatively common tests are the six-minute walk test (SMWT) and the Modified Bruce Treadmill (TM) test. These tests have been used for measurement of cardiopulmonary function in the burn population (7, 8). The exercise heart rate during these tests is a common clinical value obtained and can be used as a simple cost-effective tool to set an appropriate intensity for an exercise programme (9). Exercise heart rate is often measured during standard exercise protocols. However, the level of agreement between heart rate obtained during the SMWT and the TM test is unknown. The aim of this study was to investigate whether a submaximal SMWT offers an alternative to the TM test in children with severe burns. The study hypothesis was that the SMWT would not be in agreement with the TM test in terms of heart rate.
METHODS
Study design
This was a prospective, multicentre cross-over study, which evaluated the SMWT and TM tests for assessing cardiorespiratory and exercise function and the level of agreement of their responses. Participants were assigned to perform the SMWT and the TM test in randomized order on discharge from acute burn care. The study was conducted between 2015 and 2018. The participating paediatric burn centres included Shriners Children’s Texas, Galveston, TX, and the Shriners Hospital for Children, Sacramento, CA, USA.
Subjects
Paediatric participants between the ages of 7 and 17 years who were admitted to the acute care unit at Shriners Children’s Texas or the Shriners Hospital for Children, Sacramento, CA, USA, were considered for inclusion in the study. Subjects who had severe burn injuries that covered 30% of their total body surface are (TBSA) or more were enrolled. Once the patients were given orders for discharge from the acute care unit, all individuals completed a SMWT and a TM test in random order. Randomization was performed after consent was obtained, and randomization was performed by a clinical biostatistician from the Office of Biostatistics at the University of Texas Medical Branch (UTMB). Randomization was done in a cross-over design for the order of test mode, i.e. SMWT or the TM test. Participants who were able to complete one test, but not the other, were excluded from the study. Other exclusion criteria were mental impairment, limb amputation, or any other physical or mental conditions that made it impossible to participate in exercise activities. There were no limitations on activities, treatment, or medications that were considered part of standard of burn care (SOC). Common SOC at burn centres included surgical interventions for burn debridement, medications aimed at reducing the hypermetabolic effect of severe burns, early nutritional intervention, and physical and occupational therapy activities and exercises that aimed to improve range of motion, ambulation, mobilization, and stretching.
Six-minute walk test
The SMWT was conducted according to the American Thoracic Society guidelines (10) indoors, along a long, flat surface in an area with little traffic. Each individual was given the same instructions verbally and was allowed to use walking aids during the test as needed. All participants were under the supervision of a physical therapist, occupational therapist, or exercise physiologist to ensure that the SMWT was completed correctly. At the end of 6 min, the participant was instructed to stop, and the distance walked was measured, rounding to the nearest foot. The maximum heart rate during the SMWT was recorded every minute using a digital finger heart rate monitor (Rad-57®-Pulse CO-Oximeter® (Masimo Corp., Irvine, CA, USA) and Radical-7® Pulse CO-Oximeter® (Masimo Corp., Irvine, CA, USA)). A Borg’s Rated Perceived Exertion level (RPE; CR-10) also served as indicator for assessing the effort value of the SMWT (11).
Modified Bruce Treadmill Test
The TM test consisted of multiple exercise stages (12, 13). Initial speed was set at 0.75 m/s and angle of elevation at 0%. Speed and elevation were then increased every 3 min. Participants were continually encouraged to complete 3-min stages. Patients were told to walk on the treadmill to volitional fatigue that interfered with keeping up with the treadmill speed (12). As with the SMWT, patients were allowed to warm up by taking a few steps prior to starting the official reading. Patients were allowed to end the treadmill walking period completely or slow down as needed at any time. The test was brought to an end when the participant’s maximum effort was reached, and the participant was unable to maintain pace on the treadmill belt. The TM test maximum heart rate and maximal oxygen uptake (VO2) were assessed using the Medgraphics CardiO2 and a VO2/ECG exercise system (Medgraphics Cardiorespiratory Diagnostics, St. Paul, MN, USA). Participant’s heart rate was monitored continuously during the TM test. A subanalysis of the participants from Galveston Texas (n = 24) was conducted, by assessing the correlation between the total distance walked in the SMWT and the measured peak VO2 in the TM test (Fig. 1). Peak VO2 could not be measured in the remaining subjects from Galveston (n = 7), due to severe facial burns or multi-drug-resistant infection. All participants completed both tests at discharge from the acute care unit. Primary outcome measure was heart rate, and secondary outcome measures were RPE CR-10 score, distance, and peak VO2.

Fig. 1. Distance measured with six-minute walk test (SMWT) and peak VO2 measured with treadmill test (TM) test shows no correlation.
Statistical analysis
Data from the study, including demographic information, date of birth, sex, and TBSA, were inputted into Google Sheets spreadsheets. All statistical calculations were performed using either Google Sheets or Microsoft Excel. Comparison and correlation graphs were also completed using Google Sheets or Microsoft Excel. Data are expressed as means ± standard deviation (SD). Significance was set at p ≤ 0.05 and the p-value was determined using a paired 2-group t-test. A Pearson correlation was performed to assess the relationship between the SMWT and the TM test in terms of heart rate, total distance walked and total distance walked/peak VO2. A plot of SMWT minus TM difference in HR (y-axis) against the mean of the SMWT and TM (x-axis) was made to assess agreement of HR between SMWT and TM, following the Bland–Altman method (14). In addition, the level of agreement between SMWT and TM was assessed by calculating the bias (mean and SD of the differences), and the 95% confidence intervals (95% CI) for the bias. The power calculation was based on preliminary data, in which a sample size of 38 children will achieve 90% power using a 2-sided paired t-test when the effect size is 0.54 and alpha is 0.05.
Ethical considerations
The study was approved by the Institutional Review Board of the University of Texas Medical Branch (IRB # 14-0525) and the University of California Davis, Davis, CA (IRB # 734894-20). Prior to the start of the study, each child’s parent or legal guardian signed a written informed consent form. All participants were assured confidentiality and anonymity. This clinical trial is registered at Clinicaltrials.gov (NCT #02739464).
RESULTS
Demographics
A total of 67 children were enrolled in the study. Of those, 38 children with severe burns (31 males; 7 females) completed both tests. The remaining patients did not complete the study due to severity of burn injuries, death related to burn injuries, inability to walk, or participant withdrawal. Notably, 19 patients were able to finish the SMWT, but unable to finish the TM test due, most notably, to non-compliance or volitional fatigue (Fig. 2). There was no significant difference in injury characteristics, such as %TBSA burned and third-degree %TBSA burned, as well as age, between the subjects completing both tests and subjects completing only the SMWT or no test (p > 0.05). The mean age was 12 ± 3 years (range 7–17 years). The tests were taken, on a mean of 5 days from each other (± 5 days). Mean % TBSA burned was 46% ± 15%, (range 30–83%), mean third-degree % TBSA burned was 33% ± 22%. Demographics of all included subjects are shown in Table I. Each subject performed both the SMWT and the Modified Bruce TM test.
| Characteristics | |
| Total number of patients who completed both tests | 38 |
| Age, years | 13 ± 3* |
| Sex | 31 males, 7 females |
| % TBSA burn | 46 ± 15* |
| % Third-degree TBSA burn | 35 ± 22* |
| Days between SMWT and TM test | 5 ± 5* |
| *Data presented as mean ± SD or count (percentage). TBSA: total body surface area; SMWT: six-minute walk test; TM: Modified Bruce treadmill test. | |

Fig. 2. Flowchart showing enrolment and inclusion/exclusion of the participants from Shriners Children’s Texas, Galveston, TX and Shriners Hospital for Children, Sacramento, CA, USA in this multicentre prospective trial. SMWT: six-minute walk test; TM: treadmill test.
HEART RATE
Some participants achieved maximum heart rate prior to 6 min and others closer to the end of the TM walking period. The mean SWMT maximum heart rate was 135 ± 19 bpm (range 97–180 bpm) and the mean TM test maximum heart rate was 148 ± 24 bpm (range 100–197 bpm; p < 0.05), with a weak positive correlation of R2 = 0.14 (Fig. 3). Agreement between HR values using the SMWT and TM test (SMWT_HR; TM_HR) was assessed using the method of Bland and Altman. The mean of the difference, TM_HR minus SMWT_HR was –13 ± 25 bpm. The 95% CI for the level of agreements were [–62 bpm, 35 bpm], showing a poor level of agreement between these 2 methods (Fig. 4). There was no difference in maximum heart rate between the 38 subjects who completed both tests and the 19 subjects who only completed the SMWT (p > 0.05).

Fig. 3. Six-minute walk test (SMWT) heart rate vs treadmill test (TM) test heart rate (n = 38) shows a weak positive correlation. HR: heart rate; Max: maximum.

Fig. 4. Bland-Altman plot of the 2 testing methods in terms of heart rate (HR) shows a mean bias of –13 bpm, a lower level of agreement of –62 bpm and an upper level of agreement of 35 bpm. HR: heart rate; TM: treadmill; SMWT: six-minute walk test.
Borg’s Rated Perceived Exertion level
The RPE CR-10 score was measured in the SMWT and the TM test. The TM test was stopped when participant’s maximum effort was reached, and the participants were unable to maintain pace on the treadmill belt. The mean (± SD) RPE CR-10 score for the SMWT was 3 ± 2.5 (range 0–10) vs a mean (± SD) RPE CR-10 score of 10 ± 0 for the TM test. There was no difference in RPE between the 38 subjects who completed both tests and the 19 subjects who only completed the SMWT (p > 0.05).
Distance walked
The total distance walked at the end of the SMWT was measured and recorded in each participant’s chart. For the TM test, most of the participants walked for longer than 6 min, as there is no time limit. Therefore, the total length of time walked during the TM test was recorded in each participant’s chart. The total distance walked on TM was calculated using the following formula: distance = speed × time. The calculation for distance took into account any increases in speed by analysing the distance per speed value and calculating the summation of all values. The recorded distances for the SMWT and the TM test were analysed. The mean SMWT maximum distance was 294 ± 124 m (range 55 to 522 m), while the mean TM test maximum distance was 439 ± 181 m (range 53 to 976 m; p < 0.05), with no correlation of R2 = 0.0061 (Fig. 5). Agreement between distance values using the SMWT and TM test (SMWT_distance; TM_distance) was assessed using the method of Bland and Altman. The mean of the difference, TM_distance minus SMWT_distance was 144 m. The 95% CI for the level of agreements were [–301 m, 590 m], showing poor agreement between these 2 methods (Fig. 6). Pearson correlation showed that %TBSA burned and maximum distance had a weak negative correlation (r = –0.28) and when correlating for third-degree %TBSA burned vs maximum distance walked also yielded a weak negative correlation (r = –0.38). However, the 38 subjects who completed both tests could reach a statistically significant higher maximum distance compared with the 19 subjects who only completed the SMWT (p < 0.05).

Fig. 5. Distance measured with six-minute walk test (SMWT) and treadmill (TM) test (n = 38) shows no correlation. m: meter.
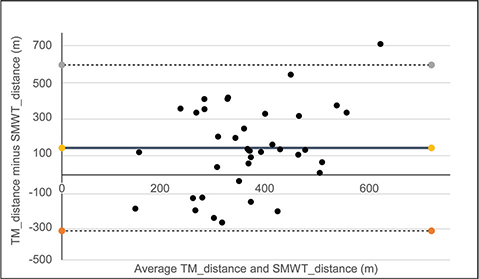
Fig. 6. Bland-Altman plot of the 2 testing methods in terms of distance shows a mean bias of 144 m, with a lower level of agreement of –301 m and an upper level of agreement of 590 m.
DISCUSSION
This multicentre prospective cohort study compared the maximum HR, RPE and total distance walked of patients with severe burn injury while performing the SMWT and TM test. This study highlights the physical condition of this population and the feasibility of exercise testing in the acute care unit at discharge. Based on these results, the TM test challenges the cardiorespiratory system significantly more than does the SMWT, as reflected by maximum heart rate measurements, and the perception of effort (i.e. RPE) by the patient. The correlation between the SMWT_HR and TM_HR was weak. This is not surprising, as the TM adds different components not present in the SMWT, such as percentage elevation and no ceiling under time, etc. In addition, the Bland–Altman plot showed a poor level of agreement, suggesting the use of the TM test for a more valid assessment of the maximum heart rate for aerobic exercise prescriptions. These findings are not surprising, as the SMWT has a stoppage time at 6 min independent of effort, although the tester attempts to motivate the patient with standard voice commands to result in a “maximal” effort. In contrast, the TM has no set time to stop, and stops with RPEs of 9–10 and heart rates > 90% of age predicted maximum values. Furthermore, this study demonstrates that subjects could walk significantly at a higher intensity (based on maximal HR).
Several studies have been conducted in the paediatric burn population, demonstrating the implementation and benefits of rehabilitative exercising. It was found that exercising restores LBM, exercise capacity, aerobic fitness, strength and pulmonary function, while improving quality of life (12, 15–17). Notably, very few hospitals have implemented rehabilitative exercise programmes during acute care or after hospital discharge (18), despite evidence showing the efficacy and implementation of exercise rehabilitation prescriptions (19). A study by Cambiaso-Daniel et al. (20) demonstrated, in a survey of practice in the US, that early rehabilitation programmes seem to be integral during burn survivor’s acute care stay; however, no true SOC exists in either exercise rehabilitation programmes, or in exercise testing methods.
To prescribe rehabilitative aerobic exercise programmes for burn survivors in a more accurate manner, an appropriate test should be used. Many methodologies for the determination of endurance training intensity in severely burned patients are currently described. A distinction can be made between objective and subjective methods for the determination of endurance training intensity. Concerning the objective methodologies, HR and VO2 (i.e. percent HR/VO2 peak) are commonly used to guide exercise prescription in clinical subjects and to determine the accurate exercise intensity (21). The higher the HR during the activity, the higher the intensity. For constant improvement in exercise capacity, an exercise intensity between 65% and 95% peak HR, that corresponds to 70–80% peak VO2, should be attained. Notably, Rivas et al. (22) showed that children with burns have an attenuated peak HR compared with non-burned children, suggesting that formulas developed by others to predict peak HR values for the purpose of estimating exercise intensity (% peak HR) may not be a valid approach in burned populations. Therefore, they suggest that an exercise stress test is needed for obtaining peak HR values for the estimation of exercise intensity for prescription purposes in burned patients. The current study shows that this population, reaches higher mean peak HR and RPEs with the TM test than with the SMWT, suggesting that the use of the TM for aerobic exercise prescription purposes is more appropriate. As running is not permitted in the SMWT, even prolonged walking at a maximum speed is far from maximal heart rate measurements in fit individuals. Interestingly, 1.5% of the study population presented a higher maximum HR during the SMWT. One reason for this could be the time between testing modalities (5 ± 5 days), although we could not confirm this, as it occurred in only 4 subjects. Notably, these 4 subjects presented with a higher RPE (= 9) in the SMWT, which was comparable to the RPE of the TM test (= 10), which would explain the higher HR attained during the SMWT.
The maximal oxygen uptake (VO2) is the gold standard (23) for quantifying cardiorespiratory endurance in healthy individuals. However, VO2 peak has also been used to quantify cardiorespiratory endurance in children with burns (3, 24, 25). In comparison with the logistic challenges of the TM test, the SMWT is simpler, and no injuries resulted during this test. This is particularly the case for children with severe functional limitations, as it could also be shown in a study in children with cerebral palsy (26). In this current study, VO2 associated with the SMWT was not compared with VO2 determined using the TM test. It would address validity; however, it would also add cost to the testing. Notably, the aforementioned study by Rivas et al. (22) provided regression equations that can be used to predict percent VO2 based on percent peak HR and be useful for prescribing appropriate exercise intensity (i.e. percent peak VO2). However, the subanalysis showed that the SMWT is not reliable in predicting peakVO2 (Fig. 1), which could be confirmed in several other studies. Therefore, the SMWT is an inexpensive and relatively easy to use alternative to test the patient’s physical abilities, rather than assessing the cardiorespiratory endurance.
Concerning the subjective methodologies, the Borg’s Rated Perceived Exertion level (RPE; CR-10) also serves as indicator for assessing the effort value, if obtaining the peak HR is not possible. The RPE scale runs from zero to 10, zero being no perceived exertion and 10 being very, very heavy. In the adult population, a moderate intensity (RPE = 4) is recommended to improve aerobic capacity and be safe at the same time, which could be also found in other fields of medicine (4, 27). In the current study, participants could reach only a mean maximum RPE of 3 in the SMWT vs a mean maximum RPE of 9 or 10 in the TM test, reflecting a submaximal perceived estimation of effort during the SMWT.
Based on the current results, the TM test allows us to challenge the cardiorespiratory capacity of our patients more, and possibly reveal more valid results of cardiorespiratory maximal endurance than the SMWT. However, the SMWT seems more clinically feasible and is still appropriate for those patients who cannot participate in the TM test. Furthermore, the SMWT provides a valuable option for assessing submaximal functional exercise capacity in low-to-middle-income countries with limited access to resources. The SMWT does not correlate with the peak VO2 measured in the TM test and shows lower RPEs due to a possible ceiling effect of the SMWT when conducted with more capable and fit patients. However, the SMWT is applicable in people with severe functional limitations rather than those whose functional limitations are mild. In this study, 19 subjects who finished the SMWT were excluded, because they could not finish the TM test, due to the severity of the burn injury (Fig. 2). Therefore, it is important to find the “right” test for each individual. If the patient is not able to run on a treadmill due to physical or mental impairment, then the TM test should not be forced and the SMWT might be the best option for the individual. A recent study by Kakitsuka et al. (7) showed that the SMWT is applicable and well tolerated for the assessment of functional exercise capacity at the time of hospital discharge in burn survivors. Therefore, the SMWT should not be discounted for these purposes.
Study limitations
This study has some potential limitations. Firstly, it was not possible to follow-up the patients for several months post-discharge, or to further evaluate the long-lasting effects of the aerobic exercise programme prescriptions, which would add more validity to this study. Secondly, a small sample size was included into the final analysis. However, as seen in Fig. 2, many of the patients were excluded due to burn injury limitations, which underscores the reality and applicability of clinical practice and the physical ability of each participant at acute care discharge. Finally, there was no ambulatory gas exchange indirect calorimeter to measure VO2 during the SMWT. Despite these potential limitations, this study is the first to evaluate 2 different tests upon discharge after acute care for aerobic exercise prescription purposes in this population.
Conclusion
The TM test challenges the cardiovascular system more than the SMWT in terms of heart rate and RPE in paediatric patients with severe burns. When possible, the TM test should be used for more valid cardiorespiratory exercise prescriptions in this population. The SMWT is more clinically feasible in many burn settings and has proven applicable, well tolerated and reproducible in people with severe functional limitations rather than those whose functional limitations are mild (7). Future studies should include a larger sample size and measurement of gas exchange during the SMWT in paediatric patients with severe burns.
ACKNOWLEDGEMENTS
The authors acknowledge Miss Angela Agudelo and Miss Shauna Glover for the exercise training and exercise testing of the participants.
Author contributions
OES, IP, for exercise experimental design, OES and IP, AP, SA contributed to data collection, OES, AP, SA and HS for data analysis, OES, IP, RPM, SEW, DNH, JOL, SS, LKB contributed to clinical research design, AP, SA, OES for the completion of final manuscript draft. All authors approved the final version.
REFERENCES
- American Burn Association. Burn Incidence Fact Sheet. Burn incidence and treatment in the United States: 2016 [serial on the internet]. 2020 [cited 2021 Dec 3]. Available from: https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/
- Bloomfield SA. Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc 1997; 29: 197–206.
- Porter C, Hardee JP, Herndon DN, Suman OE. The role of exercise in the rehabilitation of patients with severe burns. Exerc Sport Sci Rev 2015; 43: 34–40.
- de Lateur BJ, Magyar-Russell G, Bresnick MG, Bernier FA, Ober MS, Krabak BJ, et al. Augmented exercise in the treatment of deconditioning from major burn injury. Arch Phys Med Rehabil 2007; 88: S18–23.
- Al-Mousawi AM, Williams FN, Mlcak RP, Jeschke MG, Herndon DN, Suman OE. Effects of exercise training on resting energy expenditure and lean mass during pediatric burn rehabilitation. J Burn Care Res 2010; 31: 400–408.
- Suman OE, Mlcak RP, Herndon DN. Effect of exercise training on pulmonary function in children with thermal injury. J Burn Care Rehabil 2002; 23: 288–293; discussion 287.
- Kakitsuka EE, Morita AA, Itakussu EY, Kuwahara RM, Anami EHT, Pitta F, et al. Six-minute walk test in burned subjects: Applicability, reproducibility and performance at hospital discharge. Burns 2020; 46: 1540–1547.
- Porro L, Rivero HG, Gonzalez D, Tan A, Herndon DN, Suman OE. Prediction of maximal aerobic capacity in severely burned children. Burns 2011; 37: 682–686.
- Palackic A, Suman OE, Porter C, Murton AJ, Crandall CG, Rivas E. Rehabilitative exercise training for burn injury. Sports Med 2021; 51: 2469–2482.
- American Thoracic Society. ATS Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117.
- Przkora R, Herndon DN, Suman OE. The effects of oxandrolone and exercise on muscle mass and function in children with severe burns. Pediatrics 2007; 119: e109–116.
- Suman OE, Spies RJ, Celis MM, Mlcak RP, Herndon DN. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J Appl Physiol (1985) 2001; 91: 1168–1175.
- Froelicher VF, Quagletti S. Applying the exercise test. In: Froelicher VF, Quagletti S, editors. Handbook of exercise testing. 1st edn. Boston: Little, Brown, and Company; 1996, p. 16–17.
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160.
- Hardee JP, Porter C, Sidossis LS, Borsheim E, Carson JA, Herndon DN, et al. Early rehabilitative exercise training in the recovery from pediatric burn. Med Sci Sports Exerc 2014; 46: 1710–1716.
- Rosenberg M, Celis MM, Meyer W, 3rd, Tropez-Arceneaux L, McEntire SJ, Fuchs H, et al. Effects of a hospital based wellness and exercise program on quality of life of children with severe burns. Burns 2013; 39: 599–609.
- Suman OE, Herndon DN. Effects of cessation of a structured and supervised exercise conditioning program on lean mass and muscle strength in severely burned children. Arch Phys Med Rehabil 2007; 88: S24–29.
- Diego AM, Serghiou M, Padmanabha A, Porro LJ, Herndon DN, Suman OE. Exercise training after burn injury: a survey of practice. J Burn Care Res 2013; 34: e311–317.
- Disseldorp LM, Nieuwenhuis MK, Van Baar ME, Mouton LJ. Physical fitness in people after burn injury: a systematic review. Arch Phys Med Rehabil 2011; 92: 1501–1510.
- Cambiaso-Daniel J, Parry I, Rivas E, Kemp-Offenberg J, Sen S, Rizzo JA, et al. Strength and cardiorespiratory exercise rehabilitation for severely burned patients during intensive care units: a survey of practice. J Burn Care Res 2018; 39: 897–901.
- Pescatello LS. ACSM’s Guidelines for exercise testing and prescription. 9th edn. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2013.
- Rivas E, Herndon DN, Cambiaso-Daniel J, Rontoyanni VG, Porter C, Glover S, et al. Quantification of an exercise rehabilitation program for severely burned children: the standard of care at Shriners Hospitals for Children(R)-Galveston. J Burn Care Res 2018; 39: 889–896.
- Kenney WL. ACSM’s guidelines for exercise testing and prescription. 6th edn. Baltimore: Lippincott Williams & Wilkins; 2000.
- Porro LJ, Al-Mousawi AM, Williams F, Herndon DN, Mlcak RP, Suman OE. Effects of propranolol and exercise training in children with severe burns. J Pediatr 2013; 162: 799–803 e791.
- Rivas E, Herndon DN, Beck KC, Suman OE. Children with burn injury have impaired cardiac output during submaximal exercise. Med Sci Sports Exerc 2017; 49: 1993–2000.
- Nsenga Leunkeu A, Shephard RJ, Ahmaidi S. Six-minute walk test in children with cerebral palsy gross motor function classification system levels I and II: reproducibility, validity, and training effects. Arch Phys Med Rehabil 2012; 93: 2333–2339.
- Mottola MF. Components of exercise prescription and pregnancy. Clin Obstet Gynecol 2016; 59: 552–558.