ORIGINAL REPORT
EFFECT OF SENSE OF COHERENCE ON LONG-TERM WORK PARTICIPATION AMONG REHABILITATION PATIENTS: A LONGITUDINAL STUDY
Anne Mette BERGET, MSc1,2, Vegard Pihl MOEN, PhD1,3, Merethe HUSTOFT, PhD1,3, Jörg ASSMUS, PhD4, Liv Inger STRAND, PhD2, Jan Sture SKOUEN, PhD5 and Øystein HETLEVIK, PhD2
From the 1Centre of Habilitation and Rehabilitation in Western Norway, Haukeland University Hospital, 2Department of Global Public Health and Primary Care, University of Bergen, 3Department of Health and Functioning, Western Norway University of Applied Sciences, 4Centre for Clinical Research, Haukeland University Hospital and 5Department of Physical Medicine and Rehabilitation, Haukeland University Hospital, Bergen, Norway
Objective: To investigate the causal effect of sense of coherence on long-term work participation after rehabilitation, including stratification by age and diagnoses.
Design: Longitudinal cohort study.
Participants: Patients aged ≤ 60 years, employed and accepted for somatic interprofessional rehabilitation in 2015 (n = 192).
Methods: Patients reported sense of coherence before rehabilitation in 2015 and mental and physical functioning in 2016. Register data were used to measure work participation during 2018 and days working without social security benefits during 2016–18. Regression models were used to explore the total effect of sense of coherence and the possible mediation of functioning. Results are reported as odds ratios (95% confidence intervals).
Results: During 2018, 77% of the total study cohort participated in work activities. The subgroup with musculoskeletal diagnoses had the fewest days of working without social security benefits. A causal relationship was found between sense of coherence and long-term work participation. Some of the effect of sense of coherence was mediated by mental functioning. The total effect of sense of coherence was strongest for patients with musculoskeletal diagnoses (work participation: 1.11 (1.05, 1.17), days working without social security benefits: 1.05 (0.01, 109)).
Conclusion: Improving coping resources may be beneficial to facilitate long-term work participation after injury or illness, especially for individuals with musculoskeletal diagnoses.
LAY ABSTRACT
Sense of coherence is an inherent coping resource. The aim of this study was to investigate the effect of sense of coherence on long-term work participation among 192 rehabilitation patients. Patients reported sense of coherence before rehabilitation in 2015, and reported functioning in 2016. Register data were used to measure work participation. The study found that 77% of the patients who worked in 2015 also worked in 2018. The subgroup with musculoskeletal diagnoses had the fewest days of working without social security benefits (e.g. sick leave) during 2016–18. A stronger sense of coherence had a positive effect on long-term work participation. Sense of coherence also had an impact on mental functioning, which again had a positive effect on long-term work participation. The results suggest that interventions to improve coping resources (sense of coherence) may be important to help patients participate in working life after injury or illness, especially for individuals with musculoskeletal diagnoses.
Key words: rehabilitation; sense of coherence; coping resources; physical and mental functioning; work participation; musculoskeletal.
Citation: J Rehabil Med 2023; 55: jrm11982. DOI: https://doi.org/10.2340/jrm.v55.11982
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Sep 26, 2023; Published: Oct 19, 2023
Correspondence address: Anne Mette Berget, Centre of Habilitation and Rehabilitation in Western Norway, Østre Nesttunvegen 2, NO-5221 Nesttun, Bergen, Norway. E-mail: anne.mette.gravaas.berget@helse-bergen.no
Competing interests and funding: The authors have no conflicts of interests to declare.
There is evidence that employment is beneficial for physical and mental health (1–3). Participation in working life is a common goal for society and for the individual. Nevertheless, many people tend to leave working life prematurely due to health problems or disability (4). Individuals experiencing health problems that cause functional limitation are commonly offered rehabilitation aimed at maintaining or improving their functioning (5).
Reduced work participation due to illness or diagnoses that cause functional limitation is reported in several studies among people with back pain (6), cancer (7) and stroke (8). Musculoskeletal diagnoses are a major contributor to early exit from working life (9). In Norway, approximately 30% of work absence is due to musculoskeletal diagnoses (10). Better functional recovery is associated with work participation after stroke (11), critical illness (12) and with inflammatory joint conditions (13). However, additional factors, such as coping, expectation of recovery, and duration of absence, have also been found to predict work participation (14–17).
From Antonovsky’s salutogenic perspective, health is described as a continuum and focuses on resources within the individual that improve health (18). A key concept in Antonovsky’s salutogenic approach is sense of coherence. Sense of coherence is described as the individuals’ capability to mobilize their internal and external resources to cope with challenges in everyday life and is central in movement towards the health end of the continuum (19, 20). Three important resources for the individual are highlighted: comprehensibility, manageability, and meaningfulness. Comprehensibility is a cognitive aspect and refers to the sense that stimuli are understandable. Manageability is a behavioural aspect and refers to the belief that one has the resources to manage the stimuli and stay in control. Meaningfulness is a motivational aspect and includes the feeling that things are meaningful and worth your time and effort. Antonovsky regarded meaningfulness as the driving force of life and therefore the most important resource of sense of coherence (19).
In studies among rehabilitation patients, sense of coherence has been found to be an important factor for improving health and function (21, 22).
In a regional, non-rehabilitation setting, a Swedish survey-based study found that individuals with strong sense of coherence had greater work participation than individuals with weaker sense of coherence (23). Another Swedish study, conducted across diagnoses, combined patient-reported survey data from 1 measurement point and 2 years of register data before and after the survey, found that stronger sense of coherence predicted return to work (24). However, in a Norwegian rehabilitation setting, a study among patients with chronic musculoskeletal pain found no evidence that sense of coherence was associated with work participation 52 weeks after vocational rehabilitation (25).
To our knowledge, no studies have previously investigated the causal effect of sense of coherence, assessed before rehabilitation, on long-term work participation using patient-reported data and register data in a rehabilitation setting. Thus, the aim of this study was to investigate this effect using a combination of patient-reported data and register data from a generic rehabilitation cohort after somatic interprofessional rehabilitation. A second aim was to examine the effect of sense of coherence on long-term work participation, stratified by age and diagnoses.
The study hypothesis was of a causal relationship between sense of coherence and long-term work participation; that: (i) patients with stronger sense of coherence have a higher level of work participation; (ii) sense of coherence has a positive effect on work participation; and (iii) sense of coherence has a direct positive effect on work participation mediated by physical and mental functioning.
METHODS
Study design and setting
This study was part of the Rehabilitation Cohort West (REKOVE) study, a multi-centre, longitudinal cohort study conducted among rehabilitation patients and based on patient-reported survey data and register data.
Between 2015 and 2016, all patients received up to 4 weeks of somatic, interprofessional rehabilitation as an inpatient or outpatient in specialized, secondary healthcare. As described in the agreement between the rehabilitation centres and the regional health authority, rehabilitation across all centres was evidence-based, goal-orientated, and individually adapted. Interventions focused on physical activity, cognitive approaches, coping strategies, and pain management.
Patient-reported data were collected using well-known instruments prior to admittance to specialized rehabilitation (secondary healthcare) in 2015, and 1-year follow-up data were collected in 2016. Register data (2015–18) were retrieved from Statistics Norway (SSB) and the Norwegian Control and Payment of Health Reimbursements database (KUHR). SSB data included sociodemographic measures and information regarding education, income, and social allowances. KUHR data included contacts with general practitioners and diagnoses according to the International Classification of Primary Care (ICPC-2) for each patient contact.
Participants
Patients living in Western Norway, aged ≥ 18 years and who were accepted for specialized rehabilitation between January and June 2015 were invited to participate in the REKOVE study. Of the 2,863 eligible participants, 984 responded to the baseline survey and 675 responded to the 1-year follow-up survey. In the current study, patients were included if they responded to the 1-year follow-up survey, were ≤ 60 years old and were working in 2015 with a yearly income ≥ 45,034 NOK≈4,300 € (the limit for receiving sick leave allowance in 2015). Individuals were excluded if they received disability allowance or pension in 2015 (Fig. 1).
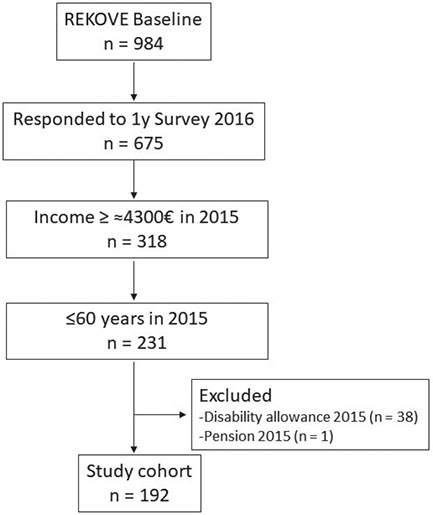
Fig. 1. Flowchart of the inclusion process of study participants. REKOVE: Rehabilitation cohort west; 1y: 1 year.
Causality
In this study, causality by time was determined using explanatory measures from 2015, with mediation measures from 2016 and outcome measures from 2016 through 2018 (Fig. 2).
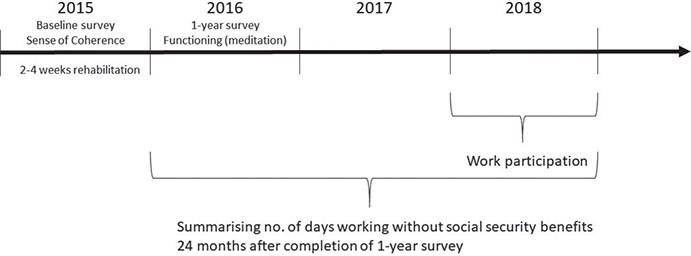
Fig. 2. Hypothesizing causality by time. Explanatory variable (sense of coherence) from the baseline survey, mediation variable (functioning) from the 1-year follow-up survey, and outcome variable: (i) work participation during 2018; (ii) days without social security benefits 2 years following completion of the 1-year follow-up survey.
Outcome variables
The first outcome variable was work participation during 2018 (Fig. 2). Work participation was defined as having a yearly income ≥ 48,442 NOK≈4,600 € (the limit for obtaining a sick leave allowance in 2018).
The second outcome variable was level of work participation, defined as days without receiving social security benefits from the Norwegian national social insurance scheme (e.g. sick leave, work assessment allowance, disability allowance). Days were summarized from the date the patient completed the 2016 survey through the following 24 months (Fig. 2). This approach was chosen to ensure the same timeline for comparable data on functioning at the start of the observational period.
Explanatory variable
The explanatory variable was sense of coherence. Sense of coherence was measured at baseline (2015) using the 13-item Sense of Coherence questionnaire (SOC-13). Responses were given on a 7-point Likert-type scale from “never” (1) to “very often” (7). Five negatively formulated items were recoded. Scores were summarized to a global score of 13–91, where 91 was the best score. Higher scores indicated that the participant finds their life comprehensible, manageable, and meaningful (19). The SOC-13 has been found to be a valid and reliable measure (26, 27).
Mediator variable
Physical and mental functioning was used as a mediator variable and measured at 1-year follow-up (2016) using the 36-Item Short Form Health Survey (SF-36), version 1. The SF-36 is a self-reported generic measure of health and functional outcomes that are affected by disease and treatment (28, 29). The instrument assesses 8 functional domains, summarized into 2 components: a physical component summary (PCS) and a mental component summary (MCS). The PCS measures general health, bodily pain, physical functioning, and role physical; the MCS measures vitality, social functioning, mental health, and role emotional (30). The PCS and MCS were calculated on a scale from 0 to 100 in accordance with the SF-36 scoring manual, with a higher score representing better functioning (30, 31). The SF-36 has been shown to be a valid and reliable instrument (29). Normative data for the Norwegian population are available (32).
Adjustment variables
Referral diagnoses related to rehabilitation, based on the International Classification of Diseases Tenth Revision (ICD-10) (33), were used to categorize participants into 2 diagnoses groups: patients with musculoskeletal diagnoses and those with other diagnoses. Data on comorbidity were obtained from KUHR. A selection of diagnoses based on the ICPC-2 comorbidity index was used to categorize comorbidity into 4 groups (from 0 to 3 or more) (34). The highest level of education completed was categorized as elementary school (at most 10 years completed), high school (11–13 years), or university/college (≥ 14 years). In addition, age in years (obtained in 2015) and sex were used as adjustment variables.
Statistical methods
For descriptive statistics, percentage, mean, and standard deviation (SD) are reported. A directed acyclic graph (DAG) was used to form a hypothesis model of a causal relationship to build the regression models (Fig. S1). Baron & Kenny’s (1986) criteria for mediation were used to define mediation between the explanatory variable and outcomes (35). The SOC-13 was regressed with the MCS and PCS to analyse potential mediation. Then, logistic regression was used to explore the odds ratio (OR) of work participation, with the dichotomous outcome variable of work participation (yes/no). Ordinal regression was used to explore the grade of work participation (days working without social security benefits). By using ordinal regression with a continuous outcome, we were able to compare the information found between those participants who had no days working with social security benefits and those who received social security benefits every day (36). In both regression models, the total effect of the SOC-13 was analysed before the effect of the mediator was added (Fig. 3). Adjusted and unadjusted analyses were performed in both regression models. The same procedure was used in the stratified analyses. First, we applied age-dependent stratification of participants ≥ 50 years and < 50 years, followed by stratification of participants with a musculoskeletal diagnoses and other diagnoses (not musculoskeletal). Results are reported with OR and 95% confidence intervals (95% CI). An odds ratio (OR) larger than 1 was associated with a positive outcome in both regression models (1 = OR for work participation/level of work participation). The data were analysed using Stata/SE 17 for windows (StataCorp LLC, College Station, TX, USA), R 4.2.2 (37), and MATLAB (Mathworks Inc, Natick, MA, USA).
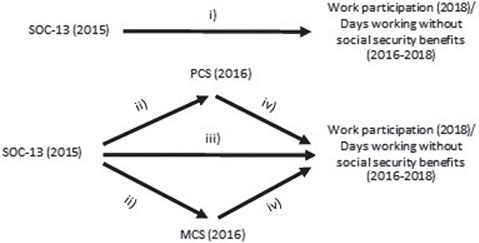
Fig. 3. Visualizing the model: (i) total effect of the 13-item sense of coherence questionnaire (SOC-13) on outcome measure (without mediation). Effect of SOC-13 in a mediation model: (ii) effect of SOC-13 on mediator, (iii) direct effect of SOC-13, (ii+iv) indirect effect of SOC-13 on outcome. MCS: Mental Component Summary; PCS: Physical Component Summary.
Missing values in the SF-36 were treated according to the SF-36 manual; participants had to respond to at least 50% of the items to obtain PCS and MCS scores (31). For the SOC-13, participants with more than 3 missing values per subscale were not included in the analysis. For included participants, missing scores were imputed according to the mean across each participant’s available responses for each subscale.
RESULTS
Of the 984 patients participating in the REKOVE study at baseline, 192 met the inclusion criteria for the current study (Fig. 1). The mean (SD) age was 49 (8) years, 63% were women, and 51% had musculoskeletal diagnoses (Table I). Of the 192 included patients, 148 (77%) were working during 2018 (3 years after inclusion in the study). These patients were younger, had higher education levels, and less comorbidity than patients who were not working (Table I).
Furthermore, patients who were working had a higher mean SOC-13 score at baseline in 2015 and higher PCS and MCS scores at 1 year follow-up (2016) compared with patients who were not working (Fig. 4. Table SI). Patients aged ≥ 50 years reported higher SOC-13 scor-es at baseline as well as higher PCS and MCS scores at 1-year follow-up compared with patients aged < 50 years (Fig. 4. Table SI). Patients with musculoskeletal diagnoses reported lower SOC-13, PCS, and MCS scor-es than those with diagnoses other than musculoskeletal (Fig. 4. Table SI). Cronbach’s alpha was 0.82 for SOC-13 at baseline and 0.94 for SF-36 at 1-year follow-up.
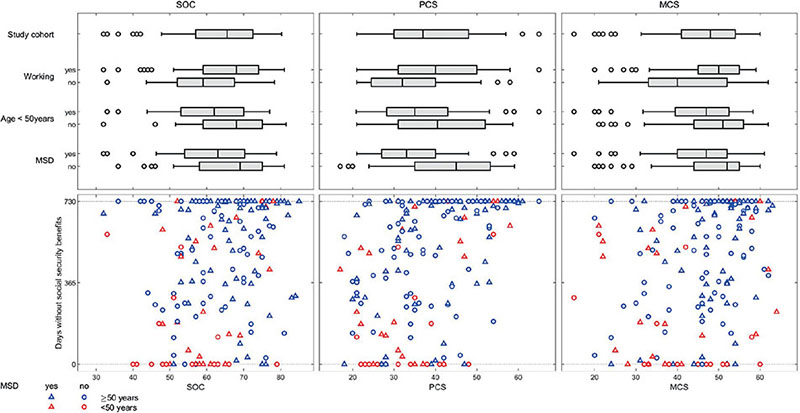
Fig. 4. Description of explanatory variable; the 13-item Sense of Coherence questionnaire (SOC-13) at baseline (2015) and mediating variable; Physical Component Summary (PCS) and Mental Component Summary (MCS) at 1 year (2016) as reported by participants. Top 3 figures: reporting values within the study cohort (n = 192) and stratification by work participation in 2018, age (≥ 50/< 50 years) and diagnoses (musculoskeletal/other). Bottom 3 figures: association between SOC-13, PCS and MCS and days without social security benefits 24 months after responding to the 1-year follow-up survey in 2016.
Mediation
In the regression model analysing the potential mediation of MCS and PCS scores at 1-year follow-up on SOC-13 scores at baseline, only the MCS was found to be associated with the SOC-13 in the total study group (β 0.43, 95% CI 0.31–0.59) and within all stratified analysis (Table SII). The PCS was not associated with SOC-13 scores in either the total study group or within the stratified analysis (Table SII); consequently, PCS scores were not qualified as a mediator of the SOC-13 in further analysis of work participation (35).
Effect of sense of coherence on work participation
In the analyses regarding the total effect of SOC-13 on work participation during 2018, a causal effect was found in the total study cohort, in both age groups, and in participants with musculoskeletal diagnoses (Fig. 5, Table SIII).
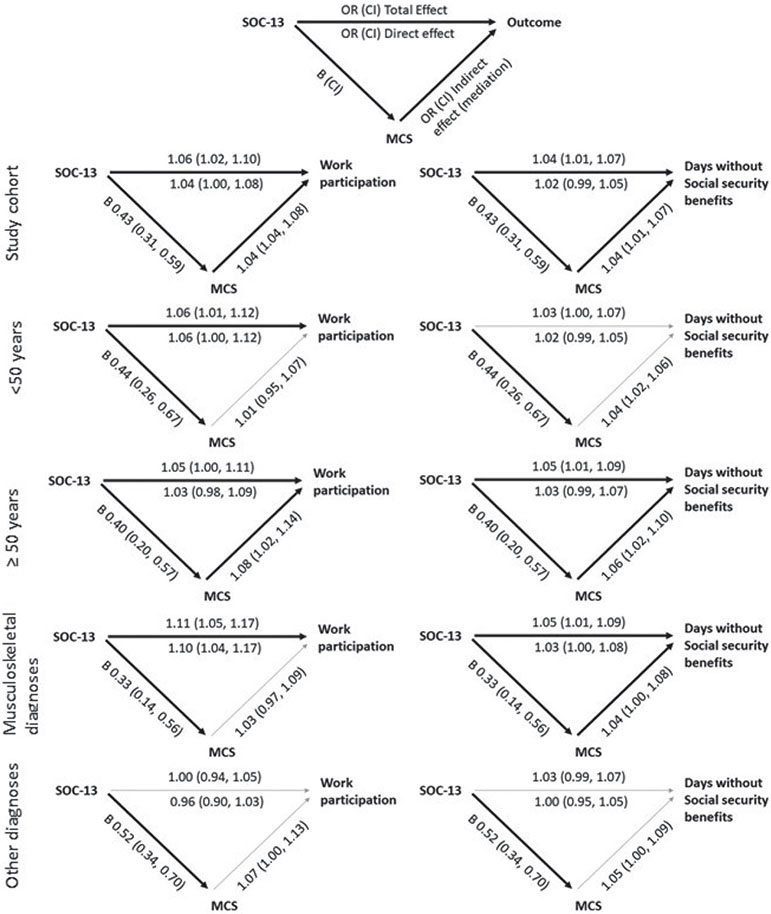
Fig. 5. Causal relationship and effect of the 13-item Sense of Coherence questionnaire (scale 13–91, 91 best) (SOC-13) baseline (2015) and work participation during 2018 (left), days working without social security benefits 24 months after completion of the 1 y survey in 2016 (right). Mediation of Mental Component Summary (scale 0–100, 100 best) (MCS) at 1 year (1y) (2016). Black arrow: relationship/mediation; grey arrow: no relationship/no mediation. Adjusted for age, sex, level of education, diagnoses, comorbidity. OR: odds ratio; 95% CI: 95% confidence interval; B: beta.
The MCS acted as a mediator between the SOC-13 and work participation in the total study group and in participants aged ≥ 50 years (Fig. 5, Table SIII).
Effect of sense of coherence on level of work participation
For the total study cohort (n = 192), the mean (SD) of days working without social security benefits during the 24 months after responding to the 1-year survey was 472.6 (270) days (minimum 0, maximum 730 days) (Table I). A higher number of days working without social security benefits was associated with better SOC-13, PCS, and MCS scores (Fig. 4). Participants with musculoskeletal diagnoses had the fewest number of days working without social security benefits in 2016–2018 (Table I).
In analysing the total effect of SOC-13 scores at baseline, a causal effect was found in the total study group, in participants aged ≥ 50 years, and in participants with musculoskeletal diagnoses (Fig. 5, Table SIV).
The MCS acted as a mediator in the total study group, in participants aged ≥ 50 years, and in participants with musculoskeletal diagnoses (Fig. 5, Table SIV).
DISCUSSION
This study investigated the effect of sense of coherence before rehabilitation on long-term work participation among rehabilitation patients. Of the patients working in 2015, 77% also participated in work 3 years later. Analysing the total study cohort, it was found that stronger sense of coherence before rehabilitation increased the odds for long-term work participation and days working without social security benefits over the 3-year follow-up period, implying a causal relationship between sense of coherence and work participation. Importantly, sense of coherence was found to be of greater importance among patients with musculoskeletal diagnoses than among patients with other diagnoses.
Sense of coherence, work participation, and diagnoses
Antonovsky (1987) claimed that a strong sense of coherence enables an individual to use adequate and effective strategies to cope with stressors (19). This hypothesized causal relationship seemed to be supported in the current study, where a stronger sense of coherence was found to be related to greater long-term work participation. The current study result is in line with a regional, survey-based Swedish study, which found that a strong sense of coherence was preventative for both short- and long-term sickness absence (self-reported 12 months prior to the survey) (23). However, the current study found that sense of coherence before rehabilitation may not have the same degree of importance across diagnoses. In the stratified analysis, it was found that sense of coherence was causally related to work participation for patients with musculoskeletal diagnoses, but not for patients with other diagnoses. An association between sense of coherence and long-term work participation was also found in a previous Swedish study among rehabilitation patients with musculoskeletal disorders (38). The authors found that individuals who were working 10 years after rehabilitation had higher SOC-13 scores (measured at 10 years) than those who were not working at that time-point. However, in contrast to the current study, the Swedish study measured sense of coherence and work participation at the same time-point, without causal analysis (38). Hence, the current study offers new knowledge regarding causality.
These results are in contrast to a previous Norwegian study among patients with chronic musculoskeletal pain (25). The authors found a significant improvement in SOC-13 scores, but no association with work participation 52 weeks after rehabilitation using between-group factor analysis measuring SOC-13 scores at 1, 5, and 52 weeks after rehabilitation (25). Explanations for differences in the results may be methodological. The current study results suggest that the time-point when sense of coherence was measured and homogeneity of the included patient groups may affect the results. The analysis indicated that an increase of 1 point on the SOC-13 scale before rehabilitation could increase the odds for work participation 3 years later, by 11% for patients with musculoskeletal diagnoses. This is encouraging because sense of coherence has been found to be changeable (25, 26), and it can be influenced by interventions in rehabilitation. Thus, adding a measure of sense of coherence at admittance to rehabilitation may therefore be beneficial in providing individually focused interventions enabling long-term work participation for this patient population.
This study did not find that sense of coherence had an effect on long-term work participation among patients with diagnoses other than musculoskeletal. This indicates that sense of coherence is of particular importance for patients with musculoskeletal diagnoses. However, this patient group constituted more than half of the current study sample; thus, we can primarily assume an effect within this group. Other diagnoses in the current study were heterogeneous, including cardiovascular and cancer diagnoses. Moreover, the diagnostic groups were small, influencing the statistical estimate of the effect. For patients with stroke or cancer diagnoses, the course of illness influencing functional change may have a larger impact on long-term work participation than the state of sense of coherence before rehabilitation. Thus, factors other than sense of coherence may be of importance within the separate diagnostic groups.
Sense of coherence, work participation, and age
In the age-dependent analysis, we found a stronger causal relationship between sense of coherence and work participation among patients aged < 50 years than among those aged ≥ 50 years. However, sense of coherence did not have an effect on days working without social security benefits for this group. This may suggest that sense of coherence has a stronger effect on whether patients aged < 50 years are or are not participating in work rather than the extent of participation. A study investigating the SOC-13 across age groups found that SOC-13 scores increased almost linearly with age (27). In the current study, participants aged ≥ 50 years had a higher mean SOC-13 score than participants aged < 50 years; as a group, older patients might have better coping strategies and might therefore be better equipped to cope with work-related challenges. A Finnish study investigating the association between a change in SOC-13 scores and a change in employment trajectories among individuals with a non-permanent job found that the effect of the SOC-13 was particularly strong among individuals < 30 years of age, i.e. a stronger sense of coherence was associated with a positive employment trajectory (39). Although the authors’ conclusion referred to younger individuals, the Finnish study may support our finding that sense of coherence has various effects on different age groups.
Mental functioning as mediator
Previous studies have found that improved functional recovery is associated with work participation (11–13). The current study found that patients with work participation during 2018 reported higher scores on the physical (PCS) and mental (MCS) component summaries of the SF-36 in 2016; a similar pattern was found among those with fewer days on social security benefits. However, the current study did not find that PCS measured at the 1-year follow-up survey could act as a mediator for SOC-13 scores at baseline. To qualify as a mediator, there must be an association between the SOC-13 and PCS; otherwise, the PCS cannot mediate any effect between SOC-13 scores and long-term work participation (35). Although the PCS cannot act as a mediator, it might still be associated with long-term work participation; however, this was not analysed in the current study. An association was found between the SOC-13 and MCS, implying that the MCS could mediate some or all of the effect between the SOC-13 and long-term work participation. The finding of the MCS as a possible mediator may confirm the relationship between sense of coherence and MCS, which was also found in previous studies, as summarized by Eriksson & Lindstrøm (20). In addition, an Italian study among patients with chronic diseases (diabetes, thyroid disorders, cancer) explored mediation between the SOC-13 and PCS and MCS (40). The authors found that the SOC-13 was directly related to the MCS and that the MCS acted as a mediator of the PCS (40). The current study did not analyse the MCS as a mediator of the PCS. The current study found that sense of coherence had a total effect on long-term work participation (without MCS in the model) as well as a combination of direct and indirect effects mediated via the MCS. This suggests that sense of coherence has an effect on mental functioning, which, in turn, affects work participation and days working without social security benefits. The current study found that the MCS might be a mediator for the total study group and for patients aged ≥ 50 years in the stratified analysis of both work participation and days working without social security benefits, as well as for both diagnostic groups regarding days working without social security benefits. This may imply that the MCS is an important factor in the causal relationship between sense of coherence and work participation for the above-mentioned groups. However, the characteristics of the subgroups may imply mediation rather than there being actual mediation. To investigate this, further analysis of interactions is needed; however, due to insufficient number of observations, this was not done in the current study. Regardless, in the absence of mediation, i.e. in the stratified analyses for patients aged < 50 years and patients with musculoskeletal diagnoses (as previously discussed), we may argue that sense of coherence is the key factor in a causal relationship.
Strengths and limitations
A strength of this study is the use of patient-reported data in combination with register data. Moreover, the use of validated instruments increases the external validity and ability to compare the results with previous research. With the longitudinal design, included patients were followed over a period of 3 years, making it possible to investigate work participation over a longer period than in other rehabilitation cohorts.
The current study also has several limitations, one being the relatively small sample size. Although the study cohort represents diagnostic groups commonly encountered in somatic rehabilitation, the small sample size within each group did not allow us to compare subgroups within the cohort other than the stratification of musculoskeletal diagnoses and other diagnoses (not musculoskeletal). In addition, participants in this cohort may not be representative for the rehabilitation group at large, as patients with severe functional limitations often receive specialized rehabilitation in hospital; thus we do not have data on their work participation. Moreover, stratification according to age (over and under 50 years) was based on data explorations of each year of age that indicated a shift in the effect of SOC-13 scores at approximately age 50 years. Additional cut-offs may be worth analysing. However, due to insufficient number of observations, this was not examined in the current study. This study offers new knowledge regarding causality and mediation; however, we cannot exclude possible intervening events explaining mediation rather than the MCS due to the timeline of measurements. Unknown or other variables may be influencing the outcome rather than the mediator.
Conclusion
This study found that patients who reported a stronger sense of coherence before rehabilitation had greater odds of work participation and days working without social security benefits over the 3-year follow-up period. Sense of coherence was found to be of greater importance among patients with musculoskeletal diagnoses than among patients with other diagnoses. The results suggest that interventions to strengthen sense of coherence, especially among patients with musculoskeletal diagnoses, could be beneficial in rehabilitation to promote long-term work participation after injury or illness.
ACKNOWLEDGEMENTS
The authors thank the Western Norway Regional Health Authority for funding this study.
This study was performed in accordance with the principles of the Declaration of Helsinki, and approved by The Regional Committee for Medical Research Ethics in Western Norway (REK-No. 2014-1636). All participants gave written informed consent.
All authors confirm that they accept and agree with the UN’s Declaration of Human Rights.
REFERENCES
- van der Noordt M, H IJ, Droomers M, Proper KI. Health effects of employment: a systematic review of prospective studies. Occup Environ Med 2014; 71: 730–736. DOI: 10.1136/oemed-2013-101891.
- Modini M, Joyce S, Mykletun A, Christensen H, Bryant RA, Mitchell PB, et al. The mental health benefits of employment: results of a systematic meta-review. Australas Psychiatry 2016; 24: 331–336. DOI: 10.1177/1039856215618523.
- Waddell G, Burton K. Is work good for your health and well-being? Lonfon: TSO (The stationary Office); 2006.
- Organisation for Economic Co-operation and Development. Sickness, Disability and Work: Breaking the Barriers. A synthesis of findings across OECD countries. Paris: OECD Publishing; 2011. DOI: 10.1787/9789264088856-en.
- Stucki G. Advancing the rehabilitation sciences. Front Rehabil Sci 2021; 1: 1–4. DOI: 10.3389/fresc.2020.617749.
- Strand LI, Ljunggren AE, Haldorsen EM, Espehaug B. The impact of physical function and pain on work status at 1-year follow-up in patients with back pain. Spine (Phila Pa 1976) 2001; 26: 800–808. DOI: 10.1097/00007632-200104010-00022.
- Arndt V, Koch-Gallenkamp L, Bertram H, Eberle A, Holleczek B, Pritzkuleit R, et al. Return to work after cancer. A multi-regional population-based study from Germany. Acta Oncol 2019; 58: 811–818. DOI: 10.1080/0284186X.2018.1557341.
- Nascimento LR, Scianni AA, Ada L, Fantauzzi MO, Hirochi TL, Teixeira-Salmela LF. Predictors of return to work after stroke: a prospective, observational cohort study with 6 months follow-up. Disabil Rehabil 2021; 43: 525–529. DOI: 10.1080/09638288.2019.1631396.
- Musculoskeletal health [database on the internet]. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions. 2022. [cited 2023 Jan 2]. Available from: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions.
- Sick leave, annual statistics (Sykefraværsstatistikk - Årsstatistikk): NAV. [cited 2023 Feb 27]. Available from: https://www.nav.no/no/nav-og-samfunn/statistikk/sykefravar-statistikk/sykefravaersstatistikk-arsstatistikk.
- Busch MA, Coshall C, Heuschmann PU, McKevitt C, Wolfe CD. Sociodemographic differences in return to work after stroke: the South London Stroke Register (SLSR). J Neurol Neurosurg Psychiatry 2009; 80: 888–893. DOI: 10.1136/jnnp.2008.163295.
- Hodgson CL, Haines KJ, Bailey M, Barrett J, Bellomo R, Bucknall T, et al. Predictors of return to work in survivors of critical illness. J Crit Care 2018; 48: 21–25. DOI: 10.1016/j.jcrc.2018.08.005.
- Geuskens GA, Hazes JM, Barendregt PJ, Burdorf A. Predictors of sick leave and reduced productivity at work among persons with early inflammatory joint conditions. Scand J Work Environ Health 2008; 34: 420–429. DOI: 10.5271/sjweh.1298.
- Cancelliere C, Donovan J, Stochkendahl MJ, Biscardi M, Ammendolia C, Myburgh C, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap 2016; 24: 32. DOI: 10.1186/s12998-016-0113-z.
- Gerg MJ, Hazak KM, Carrie BR, Melendez N, Jewell VD. Non-physical factors that impact return to work in individuals with upper extremity injuries: a scoping review. Work 2022; 73: 93–106. DOI: 10.3233/WOR-211059.
- Weerdesteijn KHN, Schaafsma F, Bonefaas-Groenewoud K, Heymans M, Van der Beek A, Anema J. Predicting return to work after long-term sickness absence with subjective health complaints: a prospective cohort study. BMC Public Health 2020; 20: 1095. DOI: 10.1186/s12889-020-09203-5.
- LoMartire R, Dahlstrom O, Bjork M, Vixner L, Frumento P, Constan L, et al. Predictors of sickness absence in a clinical population with chronic pain. J Pain 2021; 22: 1180–1194. DOI: 10.1016/j.jpain.2021.03.145.
- Mittelmark MB, Bauer GF. Salutogenesis as a theory, as an orientation and as the sense of coherence. In: Mittelmark MB, Bauer GF, Vaandrager L, Pelikan JM, Sagy S, Eriksson M, et al. (editors). The handbook of salutogenesis. Second edn. Springer, Cham, Switzerland; 2022: p. 11–17. DOI: 10.1007/978-3-030-79515-3_3.
- Antonovsky A. Unraveling the mystery of health: how people manage stress and stay well. San Fransisco, CA: Jossey-Bass; 1987.
- Eriksson M, Lindstrom B. Antonovsky’s sense of coherence scale and the relation with health: a systematic review. J Epidemiol Community Health 2006; 60: 376–381. DOI: 10.1136/jech.2005.041616.
- Moen VP, Eide GE, Drageset J, Gjesdal S. Sense of coherence, disability, and health-related quality of life: a cross-sectional study of rehabilitation patients in Norway. Arch Phys Med Rehabil 2019; 100: 448–457. DOI: 10.1016/j.apmr.2018.06.009.
- Berget AM, Moen VP, Hustoft M, Eide GE, Skouen JS, Strand LI, et al. Long-term change and predictors of change in physical and mental function after rehabilitation: a multi-centre study. J Rehabil Med 2023; 55: jrm00358. DOI: 10.2340/jrm.v55.2809.
- Engstrom LG, Janson S. Predictors of work presence – sickness absence in a salutogenic perspective. Work 2009; 33: 287–295. DOI: 10.3233/WOR-2009-0876.
- Hansen A, Edlund C, Henningsson M. Factors relevant to a return to work: a multivariate approach. Work 2006; 26: 179–190.
- Lillefjell M, Jakobsen K. Sense of coherence as a predictor of work reentry following multidisciplinary rehabilitation for individuals with chronic musculoskeletal pain. J Occup Health Psychol 2007; 12: 222–231. DOI: 10.1037/1076-8998.12.3.222.
- Eriksson M, Lindstrom B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Comm Health 2005; 59: 460–466. DOI: 10.1136/jech.2003.018085.
- Grevenstein D, Bluemke M. Measurement invariance of the SOC-13 sense of coherence scle across gender and age groups. Eur J Psychol Assess 2022; 38: 61–71.
- Garratt AM, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ 2002; 324: 1417. DOI: 10.1136/bmj.324.7351.1417.
- Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ 1993; 306: 1440–1444. DOI: 10.1136/bmj.306.6890.1440.
- Ware JE, Jr., Kosinski M, Keller SD. SF-36 Physical and mental health summary scales: a user’s manual. Boston, MA: Health Assessment Lab.; 1994.
- Ware JE, Jr., Kosinski M, Dewey JE. SF-36 health survey: manual and interpretation guide. Lincoln, RI: Quality Metric Inc; 2000.
- Garratt AM, Stavem K. Measurement properties and normative data for the Norwegian SF-36: results from a general population survey. Health Qual Life Outcomes 2017; 15: 51. DOI: 10.1186/s12955-017-0625-9.
- World Health Organisation. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2nd edn. Geneva: World Health Organization; 2004.
- Sandvik H, Ruths S, Hunskaar S, Blinkenberg J, Hetlevik O. Construction and validation of a morbidity index based on the International Classification of Primary Care. Scand J Prim Health Care 2022; 40: 305–312. DOI: 10.1080/02813432.2022.2097617.
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986; 51: 1173–1182. DOI: 10.1037//0022-3514.51.6.1173.
- Harrell Jr. FE. Regression Modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Second edn. New York: Springer; 2015.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022.
- Lydell M, Marklund B, Baigi A, Mattsson B, Mansson J. Return or no return – psychosocial factors related to sick leave in persons with musculoskeletal disorders: a prospective cohort study. Disabil Rehabil 2011; 33: 661–666. DOI: 10.3109/09638288.2010.506237.
- Liukkonen V, Virtanen P, Vahtera J, Suominen S, Sillanmaki L, Koskenvuo M. Employment trajectories and changes in sense of coherence. Eur J Public Health 2010; 20: 293–298. DOI: 10.1093/eurpub/ckp171.
- Galletta M, Cherchi M, Cocco A, Lai G, Manca V, Pau M, et al. Sense of coherence and physical health-related quality of life in Italian chronic patients: the mediating role of the mental component. BMJ Open 2019; 9: e030001. DOI: 10.1136/bmjopen-2019-030001.