ORIGINAL REPORT
EFFECTS OF AN INPATIENT REHABILITATION PROGRAMME ON FUNCTIONAL CAPACITY, QUALITY OF LIFE AND PSYCHOLOGICAL DISTRESS IN PATIENTS WITH POST COVID-19 CONDITION: AN OBSERVATIONAL STUDY
Daniel GRAF, PhD1,2, Stefan GSCHWENTER, MA1, Marina KUZDAS-SALLABERGER, MSc1, Gabriele REIGER, MD3, Alexandra EDLMAYER, MD1, David FELDER, MAG1, Hermine KLAUSBERGER3, Katharina WAGNER, BSc3 and Martin SKOUMAL, MD4
From the 1Department for Research, Innovation and Medical Service Development – Applied Rehabilitation Research, Pension Insurance Institution, Vienna, Austria, 2University of Turku, Turku, Finland, 3Rehabilitation Clinic Weyer, Pension Insurance Institution, Weyer, Austria and 4Main Office, Pension Insurance Institution, Vienna, Austria
Objectives: To examine changes in functional capacity, health-related quality of life and psychological distress in patients with post-COVID-19 condition following a multidisciplinary rehabilitation programme. In addition, to explore whether additional respiratory muscle training for more impaired patients might support their recovery process.
Design: Retrospective observational cohort study.
Patients: A total of 779 patients with post-COVID-19 condition (47.9% female, mean age 56.6 years).
Methods: Measures assessed were: 6-minute walk test (6MWT), 5-level EQ-5D (EQ-5D-5L) including EQ Visual Analogue Scale (EQ-VAS) and Patient Health Questionnaire-4 (PHQ-4). Data were provided pre- and post-rehabilitation from 2 cohorts: (i) patients participating in a regular multidisciplinary rehabilitation programme; and (ii) patients receiving additional respiratory muscle training due to an initially greater level of impairment. Dependent t-tests and general linear mixed models were used for data analysis.
Results: A series of dependent t-tests revealed mean overall improvement for both groups in 6-minute walk test distance (6MWD), EQ-5D-5L index, EQ-VAS and PHQ-4 following the rehabilitation programme. General linear mixed models showed significant interaction effects between groups and time for the EQ-5D-5L index and 6MWD.
Conclusion: A multidisciplinary rehabilitation programme appears to have a beneficial impact on the recovery process of patients with post-COVID-19 condition.
LAY ABSTRACT
According to the World Health Organization (WHO) approximately 10–20% of people have ongoing symptoms following a SARS-CoV-2 (COVID-19) infection. If these symptoms persist over a period of at least 2 months it is referred to as post-COVID-19 condition. Affected patients experience impairments in their quality of life and daily activities. This study investigated the impact of a multidisciplinary rehabilitation programme on functional capacity, health-related quality of life and psychological distress in individuals with post-COVID-19 condition. The results showed beneficial changes in all 3 areas following a multidisciplinary rehabilitation programme based on the International Classification of Functioning, Disability and Health (ICF). The study also showed that patients receiving additional respiratory muscle training as part of their regular rehabilitation programme appeared to recover more rapidly than patients without such training.
Key words: EQ-5D-5L; PHQ-4; post-COVID-19 condition; long COVID; rehabilitation; respiratory muscle training; 6MWT.
Citation: J Rehabil Med 2023; 55: jrm12437. DOI: https://doi.org/10.2340/jrm.v55.12437.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Oct 5, 2023; Published: Nov 12, 2023
Correspondence address: Stefan Gschwenter, Department of Rehabilitation Research, Pension Insurance Institution, Friedrich-Hillegeist-Str. 1, 1021, Vienna, Austria. E-mail: stefan.gschwenter@pv.at
Competing interests and funding: All authors of this study are currently, or have been, employed by the Pension Insurance Institution, Vienna, Austria.
The SARS-CoV-2 (COVID-19) pandemic still poses major challenges for healthcare systems around the world. While the situation in acute care hospitals has eased, numerous studies report an increasing number of individuals who have a variety of long-lasting symptoms, even after a mild COVID-19 infection (1–3). As of the end of January 2022 approximately 350 million confirmed COVID-19 infections had been reported by WHO (4). It is estimated that 10–20% of affected individuals experience mid- to long-term impairment after their initial illness (5). This symptom complex of long-term complications was initially termed post-COVID or post-acute COVID-19 syndrome (PACS) and defined by the National Institute for Health and Care Excellence (NICE) in the UK as persistent and/or delayed or long-term COVID-19 signs and symptoms (6). Literature distinguished between 2 subtypes: (i) ongoing COVID-19 symptoms and abnormalities lasting 4–12 weeks after infection; and (ii) chronic or post-COVID-19 syndrome, a symptom complex that persists beyond 12 weeks after onset of a COVID-19 infection or is characterized by the development of new symptoms that cannot be otherwise explained (3, 6, 7). More recently the term post-COVID-19 condition (long COVID) is increasingly used in the scientific community and is defined by the WHO as continuation or development of new symptoms 3 months after the initial infection, with symptoms lasting for at least 2 months that have no other explanation (5). The most common long COVID health issues are fatigue, dyspnoea, as well as musculoskeletal, cognitive, and mental health impairments (1, 3, 8). These symptoms affect patients’ physical, cognitive and mental functions, which, in turn, influence their activities of daily living and reduce their quality of life (QoL) (8, 9).
Recent literature (8, 10), medical societies (11, 12) and the WHO (13) suggest that rehabilitation is an effective intervention to improve respiratory, physical and psychosocial impairments in patients with post-COVID-19 condition. Due to the complexity of post-COVID-19 condition and the resulting individual needs of patients, comprehensive and multidisciplinary rehabilitation should be considered (10, 14). Multidisciplinary rehabilitation programmes rely mainly on an individualized, supervised exercise programme as well as patient education, occupational therapy and psychological treatment (10). Such programmes are well established as rehabilitation interventions for many other chronic diseases (15–18).
Although rehabilitation treatment is suggested for patients with post-COVID-19 condition, and recent studies have shown promising results for multidisciplinary treatments (10, 19, 20), as well as specific single interventions (21), the evidence of its effectiveness is still limited. Moreover, to our knowledge, there are limited guidelines regarding a rehabilitation programme for these individuals (22).
The aim of the present study is to evaluate the effects of a multidisciplinary rehabilitation programme on changes in functional capacity, health-related quality of life (HRQoL) and psychological distress in patients with post-COVID-19 condition. We hypothesize that a multidisciplinary rehabilitation programme can improve functional capacity, patient’s HRQoL and psychological distress. Moreover, since COVID-19 has been shown to affect respiratory muscles (23), this study also explores whether patients who initially had impaired respiratory muscle strength and, therefore, received additional specific respiratory muscle training (RMT) recover more rapidly with regard to their functional capacity, HRQoL and psychological distress compared with patients without initial muscle strength limitations who did not undergo RMT.
METHODS
Study design, sample and procedure
This retrospective secondary data analysis used data drawn from regular clinical practice and included records from 779 patients with post-COVID-19 condition (47.9% female, mean age 56.6 years (standard deviation (SD) 13.2 years) enrolled in a 3-week inpatient rehabilitation programme between October 2020 and January 2022 at the Pension Insurance Institution rehabalitation centre in Weyer, Austria. All patients who completed their rehabilitation stay and had pre- and post-measures of the 6-minute walk test (6MWT) were included in the sample. For patients with multiple rehabilitation visits, only data from their first visit were used. All data used in this study were provided anonymously. The study was submitted to the clinical trials database (NCT05496842) and approved by the local ethics committee of the Medical Faculty of JKU Linz (1122/2022).
Based on an initial respiratory muscle strength measurement (MasterScreen Body, Jaeger, Germany), represented by the maximum inspiratory pressure (MIP), patients were assigned either to a group with RMT or a group without RMT. The cut-off for assignment to RMT was set at MIP < 6 kPa or 60 cmH2O. In some cases, the assignment was based on the expertise of the attending physician. Patients who had contraindications, such as pulmonary hypertension, pregnancy, acute infections, aortic aneurysm or other conditions which precluded RMT (e.g. hernia), did not receive RMT during rehabilitation and were therefore assigned to the non-RMT group.
Multidisciplinary rehabilitation programme for COVID-19 patients (non-respiratory muscle training)
The multidisciplinary rehabilitation programme is a coordinated pool of treatments and therapeutic interventions lasting approximately 3 weeks to treat lung-related diseases and to provide the best possible physical, mental and social conditions for recovery within the framework of the International Classification of Functioning, Disability and Health (ICF) (24). The goal for recovery may be individual for each patient, but can be generalized to maintaining or regaining optimal functioning in their community through their own efforts and slowing or reversing disease progression through improved health behaviours. Accordingly, multidisciplinary rehabilitation is a complex, comprehensive intervention, which includes exercise training, patient education, psychosocial management and behavioural modification programmes to improve physical and emotional well-being. The rehabilitation programme for patients with post-COVID-19 condition consists of an individualized set of supervised exercises, individual therapy (e.g. physical, occupational therapy), nutritional counselling, smell retraining therapy, patient education and psychosocial support, depending on their specific needs (see Table I for an overview).
Multidisciplinary rehabilitation with respiratory muscle training
Patients with a MIP < 6 kPa or physician referral underwent supervised RMT in accordance with Göhl et al. (25) as an additional part of their multidisciplinary rehabilitation programme (see Table I). RMT was performed 3 times a week for the duration of their rehabilitation stay in a group of up to 6 participants. Each session consisted of 7 sets of training using a positive expiratory pressure device (PEP – IN 3.5 mm, OUT 5 mm and +100/–150 manometer) (PEP/RMT Set, Mediplast, Sweden). Participants breathed for 90 s in each set followed by a 60-s rest. The intensity was at 60–70% of their individual MIP. Participants were asked to train on their own (unsupervised) on the remaining days (maximum 7 days/week).
Measures
Six-minute walk test. To measure functional capacity, a 6MWT was performed on the day of admission and 2 days before discharge from rehabilitation. The 6MWT is a valid and reliable test of functional capacity in chronic respiratory conditions (26). The primary outcome of the 6MWT, the 6-minute walk distance (6MWD), is used to compare changes in functional performance over the course of rehabilitation. Changes exceeding 30 m can be considered clinically meaningful, as shown by studies in adult patients with chronic respiratory disease (26, 27).
5-level EQ-5D. The EQ-5D-5L is a general instrument for measuring patient-reported outcomes that can be used to evaluate subjective HRQoL. It includes 5 dimensions: mobility, self-care, usual activities, pain/physical discomfort, and anxiety/depression. Each dimension is represented by 1 item with response levels ranging from “1 – no problems” to “5 – extreme problems”. The EQ-5D-5L is capable of describing 55 = 3,125 different states of health and provides an EQ-5D-5L index value that can be calculated using a set of preference values from a general population. Since there is no value set for the Austrian population, the German value set was used for calculations. The index value ranges between –0.661 (extreme problems in all 5 dimensions) and 1 (no problems in any dimension) (28). In addition, a visual analogue scale (VAS) measures respondents’ subjective health conditions by asking them to rate their current condition on a scale ranging from 0 (worst imaginable health) to 100 (best imaginable health) (29).
Patient Health Questionnaire-4. The PHQ-4 is an ultra-brief self-reported questionnaire screening for symptoms of anxiety and depression. It consists of 2 2-item subscales: the PHQ-2 for depression and the GAD-2 for anxiety. Items are combined to form 2 corresponding sub-scores or a total score. Thus, the subscale values can have scores between 0 and 6, while the total score ranges from 0 to 12. PHQ-4 scores can be categorized as normal (0–2), mild (3–5), moderate (6–8) or severe (9–12) (30, 31).
Data analysis
Statistical procedures were performed using SAS Viya V.03.05 (SAS Institute, Cary, NC, USA). Descriptive results for continuous data are presented as mean values (M) with standard deviation (SD), and categorical data are presented as frequencies. Differences in outcomes before and after treatment were calculated by a series of dependent t-tests with Bonferroni-Holm-correction. Pre-post effect sizes and 95% confidence intervals (95% CI) are reported (32, 33). To deal with missing data within the t-test, pairwise deletion was used, which involves analysing only the available data for each pair of variables. This method allowed us to maximize the sample size for each analysis. In order to examine differences in outcomes between patient groups with and without RMT and to calculate group (RMT vs non-RMT) × time (before and after treatment) interaction effects, a series of general linear mixed models (GLMM) were performed using the restricted maximum likelihood (REML) estimator. To deal with missing data within the GLMMs maximum likelihood estimation (MLE) was utilized in the PROC MIXED procedure of SAS. The significance level for all procedures was set at p < 0.05.
RESULTS
Descriptive statistics
In total, 352 patients (64.2% female, mean (SD) age 57.0 (14.7) years were enrolled in a rehabilitation programme with RMT and 427 patients (34.4% female, mean (SD) age 56.2 (11.8) years in a rehabilitation programme without RMT (non-RMT). Table II shows sample characteristics and results for patients with and without RMT. The mean (SD) MIP was 6.10 (2.22) in the RMT group and 9.54 (2.58) in the non-RMT group (see Table II).
Overall changes in exercise capacity, health-related quality of life, and psychological distress
Results indicate that patients walked significantly longer distances in the 6MWT after treatment (mean (SD) 516.0 (119.3) m) than before (415.3 (128.8) m). The mean difference in the 6MWD was 100.8 m (95% CI 95.8, 105.8). In addition, patients reported to be significantly less restricted in their HRQoL (EQ-5D-5L index) after treatment (mean (SD) 0.91 (0.12)) than before (0.80 (0.18)). The mean improvement in the EQ-5D-5L index following rehabilitation was 0.11 (95% CI 0.10, 0.13). Moreover, patients rated their state of health (EQ-VAS) as being significantly better after treatment (mean (SD) 79.76 (14.77)) than before (62.11 (15.6)). A mean change in the EQ-VAS of 17.65 (95% CI 16.20, 19.10) could be observed. Finally, patients indicated less psychological distress after rehabilitation treatment (mean (SD) 2.32 (2.64)) than before (2.87 (2.67)). The mean reduction in the PHQ-4 was 0.55 (95% CI 0.42, 0.68). Detailed results for all scales and related subscales are shown in Table III.
| Measures | n | Pre-treatment | Post-treatment | Mean change | t-value | DF | Cohen’s d |
| 6MWD | 779 | 415.26 (128.75) | 516.04 (119.34) | 100.80 (95.81, 105.80) | 39.79*** | 778 | 0.81 (0.76, 0.87) |
| EQ-5D-5L index score | 577 | 0.80 (0.18) | 0.91 (0.12) | 0.11 (0.10, 0.13) | 14.94*** | 576 | 0.75 (0.64, 0.85) |
| Mobility | 588 | 1.66 (0.96) | 1.25 (0.59) | –0.42 (–0.49, –0.35) | –11.16*** | 587 | –0.53 (–0.62, –0.43) |
| Self-care | 589 | 1.15 (0.47) | 1.05 (0.27) | –0.09 (– 0.13, –0.06) | –5.44*** | 588 | –0.25 (–0.33, –0.16) |
| Usual activity | 587 | 2.12 (0.93) | 1.41 (0.72) | –0.71 (–0.79, –0.63) | –17.97*** | 586 | –0.86 (–0.97, –0.76) |
| Pain/discomfort | 585 | 2.36 (0.88) | 1.82 (0.73) | –0.55 (–0.63, –0.47) | –13.54*** | 584 | –0.68 (–0.78, –0.57) |
| Anxiety/depression | 588 | 1.76 (0.93) | 1.26 (0.59) | –0.50 (–0.58, –0.42) | –12.99*** | 587 | –0.64 (–0.74, –0.54) |
| EQ-VAS | 585 | 62.11 (15.60) | 79.76 (14.76) | 17.65 (16.20, 19.10) | 23.90*** | 584 | 1.16 (1.05, 1.28) |
| PHQ-4 | 702 | 2.87 (2.67) | 2.32 (2.64) | –0.55 (–0.68, –0.42) | –8.29*** | 701 | –0.21 (–0.26, –0.16) |
| Depression | 702 | 1.52 (1.48) | 1.16 (1.45) | –0.36 (–0.44, –0.29) | –9.60*** | 701 | –0.25 (–0.30, –0.20) |
| Anxiety | 702 | 1.35 (1.47) | 1.16 (1.41) | –0.19 (–0.26, –0.11) | –4.88*** | 701 | –0.13 (–0.18, –0.08) |
| Data are presented as n, mean (SD), mean change (95% CI) and effect size as Cohen’s d (95% CI). EQ-5D-5L: 5-level EQ-5D; EQ-VAS: EQ Visual Analog Scale; PHQ-4: Patient Health Questionnaire-4; 6MWD: 6-minute walk distance in m; DF: degrees of freedom. ***p < 0.001 (Bonferroni-Holm adjusted). |
|||||||
Differences in changes in exercise capacity, health-related quality of life and psychological distress between groups
A series of general linear mixed models revealed a significant main effect of group for the 6MWD, the EQ-5D-5L index score, the EQ-VAS and the PHQ-4. These results indicate that the non-RMT group showed less severe impairments than the RMT group in all outcomes across time. There was also a significant main effect of time for the 6MWD, the EQ-5D-5L index score, the EQ-VAS and the PHQ-4, indicating that all outcome variables improved from time 1 to time 2 for both groups.
In addition, a significant interaction was observed between group and time for the 6MWD and for the EQ-5D-5L index score, indicating that the effect of time on the 6MWD and the EQ-5D-5L index score differed between the 2 groups. Specifically, the RMT group showed a better recovery for these outcomes from time 1 to time 2 compared with the non-RMT group. No interaction between group and time was found for the EQ-VAS and the PHQ-4. Detailed results are shown in Table IV. A graphical representation is shown in Fig. 1.
| Effect | DF | Estimate | t-value |
| 6MWT | |||
| Group | 1:777 | –96.27 (8.61) | –11.18*** |
| Time | 1:777 | 91.32 (3.39) | 26.97*** |
| Time*Group | 1:777 | 20.96 (5.04) | 4.16*** |
| EQ-5D-5L index score | |||
| Group | 1:620 | –0.09 (0.01) | –6.31*** |
| Time | 1:596 | 0.10 (0.01) | 9.67*** |
| Time*Group | 1:596 | 0.04 (0.02) | 2.97* |
| EQ-VAS | |||
| Group | 1:645 | –5.60 (1.24) | –4.50*** |
| Time | 1:618 | 17.85 (0.98) | 18.26*** |
| Time*Group | 1:618 | –0.73 (1.46) | –0.50 |
| PHQ-4 | |||
| Group | 1:700 | 1.04 (0.20) | 5.23*** |
| Time | 1:700 | –0.47 (0.09) | –5.28*** |
| Time*Group | 1:700 | –0.18 (0.13) | –1.34 |
| Data are presented as fixed effect estimates and standard errors (SE). DF: degrees of freedom. *p < 0.05; ***p < 0.001. |
|||
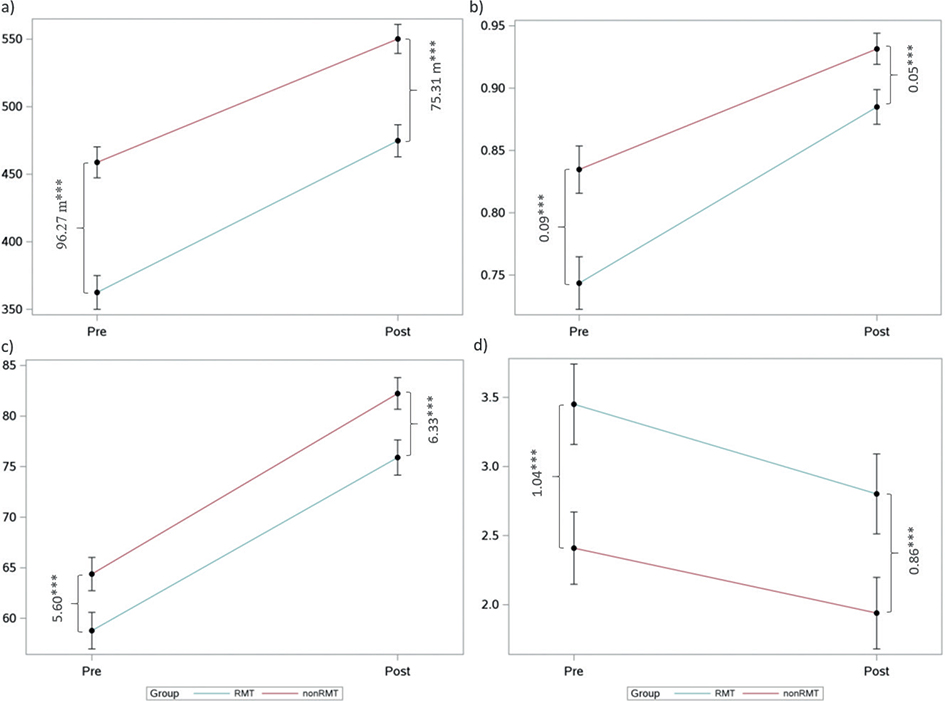
Fig. 1. Graphical representation of the results of the general linear mixed model. (a) Six-minute walk distance (6MWD), (b) 5-level EQ-5D (EQ-5D-5L) index score, (c) EQ Visual Analog Scale (EQ-VAS), and (d) Patient Health Questionnaire-4 (PHQ-4) score. ***p < 0.001.
DISCUSSION
Multidisciplinary rehabilitation is recommended by several healthcare organizations (e.g. NICE, WHO) as treatment for managing the effects of post-COVID-19 condition; however there is a lack of evidence concerning the effectiveness of certain interventions (13). Nevertheless, positive effects of multidisciplinary rehabilitation treatments have been observed in several studies. For instance, Ostrowska et al. (34) found that individuals with post-COVID-19 condition benefited from a 6-week outpatient multidisciplinary rehabilitation, particularly in terms of functional capacity. These findings are consistent with previous studies by Glöckl et al. (10) and Hermann et al. (19), who also reported improvements in functional capacity as well as in patients’ QoL after a 3-week and a 2- to 4-week inpatient rehabilitation programme, respectively. Moreover, individual interventions, such as RMT, have also been shown to be effective in improving the recovery of patients affected by post-COVID-19 condition (21, 35).
The current study retrospectively analysed changes in multiple outcomes, i.e. functional capacity, HRQoL and psychological distress after a 3-week inpatient comprehensive and multidisciplinary rehabilitation programme with a specific focus on RMT. The study found that, after completing the programme, patients with post-COVID-19 condition improved their functional capacity, HRQoL, and psychological distress. Specifically, functional capacity measured by the 6MWD improved significantly during rehabilitation, with a mean improvement of 100.8 m across the total patient cohort, which is above the suggested minimal clinically important difference (MCID) of 14–33 m for individuals with different pathologies including respiratory diseases (26, 27). However, compared with a healthy reference population (36), the 6MWD was lower in the analysed sample at both measurement points. Nevertheless, the findings of the current study regarding the 6MWT were similar to values found in comparable studies, which also documented improvements in the 6MWD (10, 37, 38). While patients in the RMT group had lower values at both time-points, they showed greater improvements in their 6MWD than patients without RMT. One explanation could be that RMT leads to a more efficient work of the respiratory muscles during exercise performance, thus reducing the feeling of exertion and shortness of breath, allowing patients to walk faster and increase their distance during the 6MWT (23, 39). Another explanation for the improvement in functional capacity could be adaptations of the cardiovascular system or improvement in skeletal musculature due to exercise therapy (40). Finally, a greater potential for improvement may also have contributed to the stronger recovery in the RMT group.
Regarding HRQoL, this study made similar observations. Compared with healthy adult German and Italian reference data, the mean EQ-5D-5L index score in the current study sample was slightly lower before rehabilitation, but improved to a score comparable to that of a healthy population at the end of rehabilitation (41, 42). Compared with the normative mean EQ-VAS for healthy German and Italian populations (41, 42), slightly lower values were observed at baseline. However, as with the EQ-5D-5L index, the EQ-VAS improved to a level similar to that of a healthy population at the end of rehabilitation. Moreover, patients with RMT had a generally lower EQ-5D-5L index score at both measurement points, but improved to a greater extent over the course of rehabilitation than patients without RMT.
The current analysis also distinguished between different dimensions of the EQ-5D-5L questionnaire. Examining the different dimensions constituting the EQ-5D-5L can be useful to learn more about the complex symptoms that patients with post-COVID-19 condition experience, and might be helpful in developing tailored rehabilitation programmes for this relatively new group of patients. The current study showed that, on average, patients were more affected in the dimensions pain and discomfort, as well as usual activities at both time-points. These 2 dimensions of HRQoL might be especially affected due to the reduced functional capacity and the impairment of respiratory muscle strength. Moreover, other factors, such as symptoms of fatigue, could additionally play a role in the context of HRQoL outcomes (43). With respect to the sub-dimension of self-care, floor effects could be observed, suggesting that, even at the beginning of rehabilitation, patients were not limited in caring for themselves even while experiencing post-COVID-19 condition. Regarding the EQ-VAS, patients improved by a mean of 17.6 points, which is more than double the MCID of 8 points (44). This is in line with findings reported by Hayden et al. (37), who report similar changes and developments in the EQ-VAS. In addition, no differences were found in the improvement of the EQ-VAS over time between the RMT vs the non-RMT group.
In contrast to recent studies, that reported clinically relevant or a higher psychological load in patients with post-COVID-19 condition (10, 37, 45), the current study did not identify greater emotional distress for patients. When comparing the RMT vs the non-RMT group, it was found that the RMT group reported mild psychological distress before treatment, but this was reduced to a normal score in the course of the rehabilitation programme. In the non-RMT group, the mean PHQ-4 score was in a normal range before and after treatment (30).
In terms of effect sizes, strong effects (i.e. before treatment – after treatment) were found in the EQ-VAS and the 6MWT. Hayden et al. (37) also noted similar findings in the EQ-VAS and 6MWT in patients with post-COVID-19 condition. Furthermore, a moderate effect size was found for the EQ-5D-5L index score and a small effect size for the PHQ-4.
Overall, these results suggest that both groups (RMT and non-RMT) benefited from the rehabilitation programme and showed improvements in functional capacity, HRQoL and psychological distress. However, despite improving functional capacity, the mean 6MWD at discharge was still lower compared with a healthy population. This indicates that some patients may require ongoing treatment, such as telerehabilitation, outpatient forms of rehabilitation, or home-based self-management programmes.
Study limitations
Despite the strengths of this study (i.e. simultaneous consideration of numerous health-related outcomes, a relatively large sample of a relatively new patient population, differentiation of patients with and without RMT), some limitations must be mentioned. First, the data analysed were collected in the context of a regular inpatient rehabilitation programme, rather than a randomized controlled trial. Therefore, the causality of the results cannot be assumed with complete certainty due to the lack of a control group. That is, improvement over time could also be due to natural recovery processes. Secondly, the study does not include a follow-up measurement. Thus, no conclusions can be drawn about the stability and long-term effects of the results. Thirdly, due to the naturalistic approach taken, it was not possible to distinguish between the different stages of post-COVID-19 condition or the severity of the individual’s COVID-infection. Future studies should consider this as a covariate in order to control for the individual potential for recovery.
In addition, although it is recommended to repeat the 6MWT twice per session, due to a possible learning effect, the strict timeframe of the routine setting did not allow for this procedure. Finally, the distribution of responses to some EQ-5D-5L items suggest the occurrence of floor effects, making it difficult to calculate a central tendency for these dimensions.
Conclusion
Multidisciplinary rehabilitation appears to have positive effects on patient recovery. The results of the current study support the integration of such a programme as a model of care for patients with post-COVID-19 condition. Functional capacity and HRQoL improved during the 3-week inpatient rehabilitation, with patients experiencing more severe impairments possibly benefiting more. In addition, reductions in psychological distress were observed. Further research is needed into the long-term effects, as well as changes in other clinical and patient-reported outcomes, following multidisciplinary long COVID-related rehabilitation treatments. Therefore, (quasi-)experimental designs could be used to analyse possible causalities and effects of rehabilitation interventions.
ACKNOWLEDGEMENTS
The authors thank Claudia Jindra and Drita Bytyqi from the Pension Insurance Institution, who helped with data management, and Benedikt Steininger for his statistical expertise.
The study was submitted to the clinical trials database (NCT05496842) and approved by the local ethics committee of the Medical Faculty of JKU Linz (1122/2022).
This study represents a secondary data analysis of data collected during regular rehabilitation stays.
REFERENCES
- Carfi A, Bernabei R, Landi F, Gemelli Against C-P-ACSG. Persistent symptoms in patients after acute COVID-19. JAMA 2020; 324: 603–605. DOI: 10.1001/jama.2020.12603
- Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med 2021; 27: 626–631. DOI: 10.1038/s41591-021-01292-y
- Alkodaymi MS, Omrani OA, Fawzy NA, Shaar BA, Almamlouk R, Riaz M, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect 2022; 28: 657–666. DOI: 10.1016/j.cmi.2022.01.014
- World Health Organization (WHO). COVID-19 weekly epidemiological update. Edition 76; 2022 25 January 2022. Geneva: WHO.
- World Health Organization (WHO). Coronavirus disease (COVID-19): post COVID-19 condition. 2021 [cited 2021 Dec 16]. Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition?gclid=Cj0KCQjw2cWgBhDYARIsALggUhprutjWOzQL5A3GYicy0jgGKQRXhiol1nF-JWlsuLHLm3SrqQI9yY4aArg8EALw_wcB
- National Institute for Health and Care Excellence (NICE). COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: NICE; 2020.
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med 2021; 27: 601–615. DOI: 10.1038/s41591-021-01283-z
- Fugazzaro S, Contri A, Esseroukh O, Kaleci S, Croci S, Massari M, et al. Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int J Environ Res Public Health 2022; 19: 5185. DOI: 10.3390/ijerph19095185
- Montani D, Savale L, Noel N, Meyrignac O, Colle R, Gasnier M, et al. Post-acute COVID-19 syndrome. Eur Respir Rev 2022; 31: 210185. DOI: 10.1183/16000617.0185-2021
- Gloeckl R, Leitl D, Jarosch I, Schneeberger T, Nell C, Stenzel N, et al. Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res 2021; 7: 00108-2021. DOI: 10.1183/23120541.00108-2021
- Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19: Interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society and American Thoracic Society-coordinated international task force. Eur Respir J 2020; 56; 2002197. DOI: 10.1183/13993003.02197-2020
- Rabady S, Altenberger J, Brose M, Denk-Linnert DM, Fertl E, Gotzinger F, et al. Leitlinie S1: Long COVID: Differenzialdiagnostik und Behandlungsstrategien. Wien Klin Wochenschr 2021; 133: 237–278. DOI: 10.1007/s00508-021-01974-0
- World Health Organization (WHO). Clinical management of COVID-19: living guideline, 13 January 2023. Geneva: WHO; 2023 (WHO/2019-nCoV/clinical/2023.1).
- Polastri M, Nava S, Clini E, Vitacca M, Gosselink R. COVID-19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J 2020; 55: 2001822. DOI: 10.1183/13993003.01822-2020
- McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2015: CD003793. DOI: 10.1002/14651858.CD003793.pub3
- McMahon SR, Ades PA, Thompson PD. The role of cardiac rehabilitation in patients with heart disease. Trends Cardiovasc Med 2017; 27: 420–425. DOI: 10.1016/j.tcm.2017.02.005
- Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2021; 11: CD001800. DOI: 10.1002/14651858.CD001800.pub4
- Dibben GO, Dalal HM, Taylor RS, Doherty P, Tang LH, Hillsdon M. Cardiac rehabilitation and physical activity: systematic review and meta-analysis. Heart 2018; 104: 1394–1402. DOI: 10.1136/heartjnl-2017-312832
- Hermann M, Pekacka-Egli AM, Witassek F, Baumgaertner R, Schoendorf S, Spielmanns M. Feasibility and efficacy of cardiopulmonary rehabilitation after COVID-19. Am J Phys Med Rehabil 2020; 99: 865–869. DOI: 10.1097/PHM.0000000000001549
- Nopp S, Moik F, Klok FA, Gattinger D, Petrovic M, Vonbank K, et al. Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration 2022; 101: 593–601. DOI: 10.1159/000522118
- McNarry MA, Berg RMG, Shelley J, Hudson J, Saynor ZL, Duckers J, et al. Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur Respir J 2022; 60: 2103101. DOI: 10.1183/13993003.03101-2021
- Agostini F, Mangone M, Ruiu P, Paolucci T, Santilli V, Bernetti A. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med 2021; 53: jrm00141. DOI: 10.2340/16501977-2776
- Severin R, Franz CK, Farr E, Meirelles C, Arena R, Phillips SA, et al. The effects of COVID-19 on respiratory muscle performance: making the case for respiratory muscle testing and training. Eur Respir Rev 2022; 31; 220006. DOI: 10.1183/16000617.0006-2022
- World Health Organization (WHO). International classification of functioning, disability and health : ICF. Geneva: WHO; 2001.
- Gohl O, Walker DJ, Walterspacher S, Langer D, Spengler CM, Wanke T, et al. Atemmuskeltraining: state-of-the-art. Pneumologie 2016; 70: 37–48. DOI: 10.1055/s-0041-109312
- Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014; 44: 1428–1446. DOI: 10.1183/09031936.00150314
- Bohannon RW, Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J Eval Clin Pract 2017; 23: 377–381. DOI: 10.1111/jep.12629
- Ludwig K, Graf von der Schulenburg JM, Greiner W. German value set for the EQ-5D-5L. Pharmacoeconomics 2018; 36: 663–674. DOI: 10.1007/s40273-018-0615-8
- Feng YS, Kohlmann T, Janssen MF, Buchholz I. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res 2021; 30: 647–673. DOI: 10.1007/s11136-020-02688-y
- Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009; 50: 613–621. DOI: 10.1176/appi.psy.50.6.613
- Lowe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 2010; 122: 86–95. DOI: 10.1016/j.jad.2009.06.019
- Kadel R, Kip K. SAS macro to compute effect size (Cohen’s d) and its confidence interval from raw survey data. Proceedings of the annual southeast SAS users group conference; 2012: Raleigh/Durham, NC; 2012.
- Cohen J. edition 2. Statistical power analysis for the behavioral sciences. Hillsdale. NJ: Erlbaum; 1988.
- Ostrowska M, Rzepka-Cholasinska A, Pietrzykowski L, Michalski P, Kosobucka-Ozdoba A, Jasiewicz M, et al. Effects of multidisciplinary rehabilitation program in patients with long COVID-19: Post-COVID-19 Rehabilitation (PCR SIRIO 8) study. J Clin Med 2023; 12: 420. DOI: 10.3390/jcm12020420
- Del Corral T, Fabero-Garrido R, Plaza-Manzano G, Fernandez-de-Las-Penas C, Navarro-Santana M, Lopez-de-Uralde-Villanueva I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: randomized controlled trial. Ann Phys Rehabil Med 2023; 66: 101709. DOI: 10.1016/j.rehab.2022.101709
- Cazzoletti L, Zanolin ME, Dorelli G, Ferrari P, Dalle Carbonare LG, Crisafulli E, et al. Six-minute walk distance in healthy subjects: reference standards from a general population sample. Respir Res 2022; 23: 83. DOI: 10.1186/s12931-022-02003-y
- Hayden MC, Limbach M, Schuler M, Merkl S, Schwarzl G, Jakab K, et al. Effectiveness of a three-week inpatient pulmonary rehabilitation program for patients after COVID-19: a prospective observational study. Int J Environ Res Public Health 2021; 18: 9001. DOI: 10.3390/ijerph18179001
- Rausch L, Puchner B, Fuchshuber J, Seebacher B, Loffler-Ragg J, Pramsohler S, et al. The effects of exercise therapy moderated by sex in rehabilitation of COVID-19. Int J Sports Med 2022; 43: 1043–1051. DOI: 10.1055/a-1866-6092
- Alvarez-Herms J, Julia-Sanchez S, Corbi F, Odriozola-Martinez A, Burtscher M. Putative role of respiratory muscle training to improve endurance performance in hypoxia: a review. Front Physiol 2018; 9: 1970. DOI: 10.3389/fphys.2018.01970
- Barbara C, Clavario P, De Marzo V, Lotti R, Guglielmi G, Porcile A, et al. Effects of exercise rehabilitation in patients with long coronavirus disease 2019. Eur J Prev Cardiol 2022; 29: e258–e260. DOI: 10.1093/eurjpc/zwac019
- Grochtdreis T, Dams J, Konig HH, Konnopka A. Health-related quality of life measured with the EQ-5D-5L: estimation of normative index values based on a representative German population sample and value set. Eur J Health Econ 2019; 20: 933–944. DOI: 10.1007/s10198-019-01054-1
- Meregaglia M, Malandrini F, Finch AP, Ciani O, Jommi C. EQ-5D-5L population norms for Italy. Appl Health Econ Health Policy 2023; 21: 289–303. DOI: 10.1007/s40258-022-00772-7
- Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys Ther 2022; 102: pzac005. DOI: 10.1093/ptj/pzac005
- Zanini A, Aiello M, Adamo D, Casale S, Cherubino F, Della Patrona S, et al. Estimation of minimal clinically important difference in EQ-5D visual analog scale score after pulmonary rehabilitation in subjects with COPD. Respir Care 2015; 60: 88–95. DOI: 10.4187/respcare.0327
- Han JH, Womack KN, Tenforde MW, Files DC, Gibbs KW, Shapiro NI, et al. Associations between persistent symptoms after mild COVID-19 and long-term health status, quality of life, and psychological distress. Influenza Other Respir Viruses 2022; 16: 680–689. DOI: 10.1111/irv.1298