ORIGINAL REPORT
SOCIAL PARTICIPATION, RESILIENCE, AND COPING TENDENCY IN A SAMPLE OF STROKE SURVIVORS: A MULTI-CENTRE CROSS-SECTIONAL STUDY IN CHINA
Xuan ZHOU1#, Ying WANG2# and Lanshu ZHOU, PhD1
From the 1School of Nursing, Naval Medical University, Shanghai and 2Department of Nursing, Shanghai First Rehabilitation Hospital, Shanghai, China
#These authors should be considered as co-first authors.
Objectives: To investigate the association between resilience and social participation and examine the mediation of resilience on coping strategies and social participation.
Design: A multi-centre cross-sectional study performed from April to July 2022.
Participants: The study sample comprised 239 stroke survivors (53.1% male). The mean age of participants was 65.4 years.
Methods: The study was conducted at 3 neurorehabilitation centres in Shanghai, China. The Utrecht Scale for Evaluation of Rehabilitation Participation (USER-P) was used to measure both objective and subjective social participation. Resilience was evaluated using the Connor-Davidson Resilience Scale (CD-RISC), while positive coping tendency was assessed using the Simplified Coping Style Questionnaire (SCSQ). Multivariate linear regression was employed, taking into account confounding factors. In cases where a significant interaction effect was observed, simple slope analysis was conducted to explore the relationship between positive coping tendency and social participation at different levels of resilience.
Results: The mean scores of social participation frequency, restriction, and satisfaction were 21.80 ± 15.13, 38.92 ± 26.48, and 63.34 ± 22.35, respectively. Higher resilience level was independently associated with higher social participation frequency (B = 0.210, p < 0.001), less participation restriction (B = 0.584, p < 0.001), and higher participation satisfaction (B = 0.250, p < 0.001). Moreover, higher resilience was correlated with more positive coping tendency. More positive coping tendency was related to higher social participation frequency and less participation restriction, but not to social participation satisfaction. Furthermore, individuals at different resilience levels moderated the effect of positive coping tendency on social participation frequency.
Conclusion: This study underlines the importance of resilience as a potential intervention in enhancing both objective and subjective social participation in stroke survivors, and provides insights into increasing the efficacy of positive coping strategies on social participation.
LAY ABSTRACT
Stroke causes considerable disability among Chinese adults. Substantial restriction in social participation is observed among stroke survivors. However, the factors associated with post-stroke social participation have not been studied. This multi-centre cross-sectional study examines the relationship between resilience and social participation, as well as the potential mediating role of resilience in the relationship between coping strategies and social participation among individuals who have survived a stroke. The finding that resilience was positively associated with both objective and subjective social participation suggests that resilience-targeted intervention may have the potential to promote social participation in stroke survivors. Furthermore, the moderating effect of resilience on the relationship between positive coping tendencies and participation frequency also presents an opportunity to enhance the effectiveness of positive coping strategies in improving social participation.
Key words: stroke; social participation; resilience; coping; cross-sectional study.
Citation: J Rehabil Med 2024; 56: jrm12448. DOI: https://doi.org/10.2340/jrm.v56.12448.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Submitted: May 4, 2023; Accepted: Nov 29, 2023; Published: Jan 4, 2024
Correspondence address: Xuan Zhou, School of Nursing, Naval Medical University, 800 Xiangyin Road, Yangpu District, Shanghai 200433, China. E-mail: zhoulanshu@hotmail.com
Competing interests and funding: The authors have no conflicts of interest to declare.
Stroke is the leading cause of disability among adults in China, exhibiting a notable prevalence, mortality, recurrence, and economic burden (1). Current stroke survivors aged 40 years and above in China exceed 13 million, with approximately 75% experiencing diminished physical capabilities (2). Consequently, social participation, an ultimate outcome of rehabilitation, remains a major challenge in stroke survivors (3). Social participation, as one of the core concepts of International Classification of Functioning, Disability and Health (ICF), refers to involvement in a life situation (4, 5). Numerous studies have consistently demonstrated that individuals who have had a stroke frequently encounter significant difficulties across various domains of social participation, encompassing social role enactment and interpersonal interaction (6, 7). These challenges subsequently exacerbate their physical impairments and psychological distress, while also diminishing their overall quality of life (8, 9). Consequently, it is imperative to comprehend the predictors of social participation and how best to advise and support stroke survivors to achieve meaningful participation.
In contemporary perspectives, social participation is regarded as a multifaceted construct that encompasses both objective indicators of individual engagement in social activities and subjective aspects related to personal experiences and satisfaction (10). Häggström et al.’s study revealed that the assessment of subjective social participation entails the identification of autonomous involvement, meaningful activities, and a sense of belonging and engagement, which cannot be adequately captured through objective observation and measurement alone (11). Previous qualitative studies have demonstrated that stroke survivors reported negative experiences in terms of participation autonomy and sense of belonging (12, 13). It seems that the perceived engagement in social activities, rather than the total number of social activities, holds greater significance for individuals with stroke. Therefore, it is imperative to consider subjective social participation when aiming to enhance social participation among stroke survivors.
There are some factors influencing individual social participation, with coping styles being the most studied, which are defined as behaviours adopted to protect oneself against stress and psychological harm from bad experiences (14). Coping styles can be divided into either positive strategies or negative strategies. Positive coping styles entail individuals actively addressing problems, whereas negative coping styles involve individuals adopting negative attitudes and approaches towards problems. Previous research has shown that higher level of social participation is associated with more use of positive coping strategies in individuals with stroke (15). In addition, Li et al. discovered that stroke survivors who employed more resignation coping tended to experience reduced perceived participation and autonomy in outdoor activities (16). Demers et al. found that behavioural coping strategies were the predominant determinant of daily activities, social roles and total participation, independent of the type of living environment and age (17). These findings underline the importance of positive coping strategies as a mechanism for abating the effect of stressful events or challenges pertaining to social participation.
Resilience has been defined by the American Psychological Association (APA) as a well-adjusted process under the impact of adversity, trauma, threats, or other stressors (e.g. family breakdown, work stress, financial stress), which means “bouncing back” from difficulties (18). Despite still being a matter of debate, the APA’s definition of resilience as a process vs a personality trait suggests that individuals possess the capacity to develop and apply resilience, irrespective of their sociodemographic background, personal experiences, or social environment (19). Extensive studies have found that individuals with a high level of resilience can experience enhanced well-being and improved quality of life, as they are able to more efficiently manage and recover from stress related to stroke (20, 21). However, the association between resilience and social participation among stroke survivors remains unclear. Directing attention towards the positive variable resilience may provide new insights for improving social participation in stroke survivors. Importantly, existing evidence has demonstrated a correlation between resilience and coping style. Zhang et al. found that stroke survivors who used resignation as a coping mechanism tended to exhibit a lower level of long-term resilience (22). A cross-sectional study conducted by Liu et al. revealed a statistically significant relationship between resilience and coping style in stroke patients during the acute stage of hospitalization (23). These findings suggest that individuals with higher resilience can use positive coping strategies more frequently and rely less on negative coping strategies (19). Thereby, social participation, resilience and coping may all interact with each other, ultimately determining the individuals’ health outcome.
Therefore, the Utrecht Scale for Evaluation of Rehabilitation Participation (USER-P), a validated questionnaire, was used to evaluate both objective and subjective social participation. The primary aim of this study was to identify the association between resilience and social participation in individuals who have had a stroke. The second aim was to determine the mediating role of resilience in the relationship between coping and social participation.
METHODS
The current study was a multicentre cross-sectional design and was approved by the ethics committee of Shanghai First Rehabilitation Hospital (YK-2021-04-036). Written informed consent was obtained from study participants.
Participants
A total of patients was recruited from 3 neurorehabilitation centres in Shanghai, China, from April to July 2022. The inclusion criteria encompassed patients meeting the following conditions: (i) diagnosis of stroke according to the Fourth National Conference on cerebrovascular disease, confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) (24); (ii) aged at least 18 years; (iii) minimum of 1 month post-stroke; (iv) possessing home experiences following stroke; (v) voluntarily signing of informed consent forms. Participants who were ineligible for the study included those with cognitive disorders, as assessed by the Montreal Cognitive Assessment (MoCA) with a score below 26, or the Montreal Cognitive Assessment-Basic (MoCA-B) with a score below 19 for individuals with limited literacy or primary school education (25). In addition, individuals with major psychiatric illness, terminal illness, such as malignancy or organ failure, and/or severe vision disorder were also excluded from the study. Participation in the study was voluntary, and participants were informed that they had the option to omit any questions they were uncomfortable with or to withdraw from the study at any point. A total of 246 participants provided consent to participate in the survey. Five patients were excluded due to regular answers and 2 persons were excluded as they missed responses for most of the items.
PROCEDURES
Print recruitment advertisements highlighting the research study were disseminated across 3 neurorehabilitation centres, prompting the evaluation of stroke patients who expressed interest in accordance with predetermined criteria for inclusion and exclusion. The potential participants were fully informed of the benefits and risks of the research. While the study does not inherently entail discernible risks, the acting of completing the questionnaire may induce fatigue among participants. Furthermore, despite diligent measures to safeguard data, the potential for inadvertent disclosure of participant information remains a concern. The potential participants were informed regarding their rights and responsibilities, such as the ability to withdraw from the study at any point without any negative consequences regarding their medical treatment. Subsequently, a written informed consent form was acquired. Trained researchers administered assessment instruments and requested participants to autonomously complete a questionnaire. In cases where participants were unable to independently complete the questionnaire due to illiteracy, the researchers would read the items aloud to ensure a comprehensive understanding and enable subjects to give their own considered answers.
Outcome measures
A self-designed general information questionnaire was used to obtain social-demographic data (e.g. age, sex, education, work or not before stroke onset, marriage, caregiver, and family income) and disease-related information (e.g. stroke type, time after onset, relapse or not, and self-care ability).
The 32-item USER-P was used to assess social participation across 3 domains: participation frequency (11 items), participation restriction (11 items), and participation satisfaction (10 items). The first 2 domain primarily capture objective social participation, while the last domain reflects subjective social participation (26). The participation frequency domain comprises 2 parts: the first part includes 4 items on frequency of vocational activity, while the second part contains 7 items examining the frequency of leisure and social activity. Participation restriction assesses the participant’s restrictions, experienced due to their health condition, in 11 activities. Participation satisfaction consists of 9 items on satisfaction with vocational, leisure and social relationship (26, 27). Responses are on a 6-point Likert scale for participation frequency with 2 anchor responses (0 “never” and 5 “36 h or more a week” or “19 times or more over 4 weeks”), a 4-point Likert scale for participation restriction with 2 anchor responses (0 “impossible” and 3 “no difficulties”), a 5-point Likert scale for participation satisfaction with 2 anchor responses (0 “extremely dissatisfied” and 4 “extremely satisfied”). Sum scores for 3 domains were computed using complex scoring outlined in the manual, with a scale ranging from 0 to 100. A high score signifies a greater frequency, less restriction, and more satisfaction. Notably, there is no total score for USER-P. The internal consistency of the USER-P was deemed satisfactory, with a Cronbach’s alpha coefficient ranging from 0.70 to 0.91. In addition, concurrent validity was established through strong correlations observed between the frequency scale and Frenchay Activity (r = 0.59), the restriction scale and the participation subscale of the ICF Measure of Participation and Activities Screener (r = 0.75), and the satisfaction scale and the Participation Scale (r = –0.73) (27, 28).The Connor-Davidson Resilience Scale (CD-RISC) was utilized to measure resilience. This scale contains 25 items that are categorized into 3 domains: tenacity (13 items), strength (8 items), and optimism (4 items) (29). A 5-rating Likert scale was used to evaluate frequency, with anchors at “0” (never) to “4” (always). The total score of this scale ranges from 0 to 100, with a higher score indicating a greater level of resilience. The CD-RISC has been translated into multiple languages and has been employed across diverse population. The Cronbach’s α coefficient of the CD-RISC was 0.89~0.906 (30, 31). The CD-RISC showed expected positive correlation with social support (r = 0.44, p < 0.001) and negative correlations with depression (r = –0.38, p < 0.001) and anxiety (r = –0.25, p < 0.001).
The 20-item Simplified Coping Style Questionnaire (SCSQ) was used to assess coping style across 2 domains: positive coping (12 items) and negative coping (8 items) (32). This scale was rated using a 4-point Likert score from 0 (no) to 3 (usually). Due to the disparity in the quantity of items encompassed within the 2 domains, it is customary to compute the mean scores of both domains when assessing the inclination towards adopting positive and negative coping styles. Furthermore, the disparity between the mean scores of the 2 dimensions serves as an indicator of coping tendency, signifying an individual’s propensity towards embracing positive or negative coping styles. The positive coping tendency is determined by subtracting the mean score of negative copingrom the mean score of positive coping, yielding a range of –3 to 3, with a higher score denoting a greater positive coping inclination. The Cronbach’s α coefficient of the SCSQ is 0.75, which shows an acceptable reliability (33).
Data analysis
Data management and statistical analyses were performed using R 4.2.1. Descriptive statistics, including frequency, percentage, mean, and standard deviation (SD), were used to present the sociodemographic and psychological characteristics of the participants. Following the assessment of normality and Levene’s test, independent sample t-tests or 1-way analysis of variance (ANOVA) were used to examine the relationships between social participation frequency, social participation restriction, social participation satisfaction, and the participants’ sociodemographic and clinical data. Pearson’s correlation analyses were used to examine the associations among social participation frequency, social participation restriction, social participation satisfaction, resilience, and positive coping tendency. Variables that yielded statistically significant results in the univariate analyses were subsequently included in the multivariate linear regression analysis to determine whether resilience could independently predict social participation and moderate the relationship between positive coping tendency and social participation. The stepwise forward selection strategy was utilized.
Moderation was deemed to have occurred when a model including interaction terms demonstrated a significantly higher amount of variance explained compared with a model without interaction terms, and when the regression coefficient corresponding to an interaction term was found to be statistically significant (p < 0.05). In the presence of a significant interaction effect, a simple slope analysis was conducted to explore the relationship between positive coping tendency and social participation at both high (+1 SD) and low (–1 SD) levels of resilience. A 2-tailed hypothesis test at a significance level of 0.05 was used to determine statistical significance. In cases of missing responses, the mean value was employed. For missing responses, the mean of all completed answers was used to impute the score. Of note, questionnaires with regular answers and missing responses greater than 5% were removed.
RESULTS
The study included a total of 239 participants, with 53.1% being male. The participants had a mean age of 65.4 years. Among them, 11.7% were younger than 45 years, 34.7% were younger than 60 years, and 24.7% were older than 75 years. A significant proportion of the participants (38.5%) had only completed primary school education, while 17.6% were illiterate. Prior to having a stroke, 20.5% of the participants reported being employed. The majority of participants (79.1%) were diagnosed with cerebral infarction. Further details regarding the characteristics of the participants are shown in Table I.
Level of perceived social participation
The mean score for social participation frequency, as measured by the subscale of the USER-P, was 21.80 ± 15.13, indicating a low level of social participation frequency. The distribution of values ranged from 0 to 74.55 and followed a normal distribution. Age (F = 9.696, p ≤ 0.000001), family income per month (F = 6.780, p = 0.001), and self-care ability (F = 2.961, p = 0.033) were found to be significantly related to social participation frequency. Table I gives a detailed overview of the associations between social participation and the characteristics of the participants. The participants who were employed prior to experiencing a stroke demonstrated a significantly higher frequency of social participation compared with those who were not employed (t = 2.106, p = 0.042). In addition, participants diagnosed with cerebral haemorrhage exhibited a higher level of social participation frequency (t = –2.485, p = 0.014). No significant associations were found between social participation frequency and variables such as sex, education, marital status, caregiver presence, onset time, and relapse. The mean score for social participation restriction, as assessed using the subscale of the USER-P instrument, was 38.92±26.48, indicating a moderate to severe restriction on social participation. The data followed a normal distribution and ranged from 0 to 100. Individuals who did not have any employment before experiencing a stroke (t = 4.202, p ≤ 0.0010) or who had a recurrent stroke (t = –3.352, p = 0.001) showed higher levels of social participation limitation (Table I). In addition, age, level of education, presence of a caregiver, monthly family income, and ability to take care of oneself were strongly correlated with social participation restriction. However, there was no significant statistical association found between social participation limitation and sex, marital status, type of stroke, or duration of stroke. The subscale of the USER-P instrument was utilized to evaluate social participation satisfaction, yielding a mean score of 63.34 ± 22.35, indicating a moderate level of satisfaction. The scores, which ranged from 0 to 100, exhibited a normal distribution. Notably, family income (F = 5.068, p = 0.007) and onset time of stroke (F = 6.222, p ≤ 0.0010) demonstrated significant associations with social participation satisfaction.
Level of resilience and positive coping tendency
The mean score for resilience on the CD-RISC questionnaire was 53.57 ± 19.17, reflecting moderate levels of resilience. The resilience scores also followed a normal distribution within the range 0 to 100. The mean scores for the 3 domains of the CD-RISC questionnaire were as follows: 27.41 ± 10.70 for tenacity, 17.57 ± 6.13 for strength, and 8.59 ± 3.06 for optimism. The mean and SD for the positive coping tendency, as measured by the SCSQ, were 0.16 ± 0.59, indicating that participants were more inclined to adopt a positive coping style. Specifically, the mean score for positive coping items was 1.45 ± 0.71, while the mean score for negative coping items was 1.29 ± 0.60.
Bivariate correlations between social participation, resilience, and positive coping tendency
Bivariate correlations are shown in Fig. 1. A higher level of resilience exhibited a strong positive association with increased frequency of social participation (r = 0.361, p < 0.001), decreased restriction in social participation (r = 0.545, p < 0.001), and enhanced satisfaction with social participation (r = 0.252, p < 0.001). In addition, a higher level of resilience was significantly linked to a greater inclination towards positive coping strategies (r = 0.449, p < 0.001). Positive coping tendency was found to be significantly associated with more frequent and less restricted social participation (r = 0.217, p = 0.001; r = 0.240, p < 0.001). However, no significant correlation was observed between positive coping tendency and satisfaction with social participation (r = 0.018, p = 0.786).
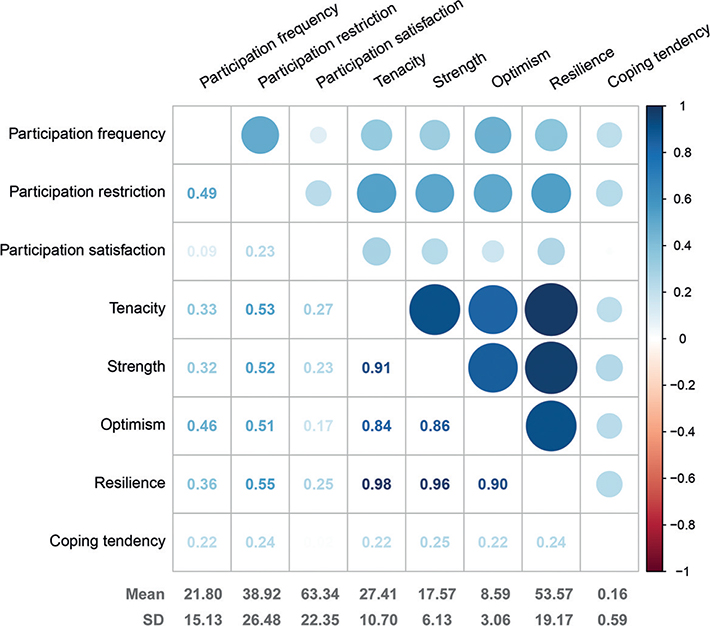
Fig. 1. Bivariate correlations between social participation, resilience, and positive coping tendency. Numbers and circles in the correlation matrix suggest significant r value. The colour of the circles reflects the strength of correlation, with a dark colour representing stronger correlation. Blue indicates positive associations and red represents negative associations. The bottom 2 rows in the figure demonstrate the mean and standard deviation (SD) for each variable.
Investigating the interaction between resilience and positive coping tendency in predicting social participation
Multiple linear regression analyses were conducted for social participation frequency (Table II). The significantly demographic and clinical characteristics (age, work, family income, stroke type, self-care ability), positive coping tendency, resilience, and the interaction terms between resilience and positive coping tendency were entered. The tests demonstrated that multicollinearity was not a concern. There were 4 variables (age, stroke type, resilience, and interaction of resilience and positive coping tendency) entering model, which accounted for 33.9% of the variance in social participation frequency (F = 21.592, p < 0.001). The majority of this variance was attributed to the independent main effect of resilience. Furthermore, the interaction term between resilience and positive coping tendency significantly contributed to the variance in social participation frequency (B = 0.077, p = 0.001). Fig. 2 demonstrates that when resilience is at high levels (+1 SD), there is a positive and significant relationship between positive coping tendency and social participation frequency (B = 0.362, p < 0.001). Conversely, when resilience is at low levels (–1 SD), the relationship between positive coping tendency and social participation frequency is inverse and significant (B = –0.276, p < 0.001). This suggests that individuals with low resilience may experience less benefit and even some adverse effects when engaging in positive coping strategies to improve their frequency of social participation. With regards to predictors of social participation restriction, the optimal model included 4 variables: age, family income, self-care ability, and resilience, which explained 40.8% of the overall variance in social participation restriction (F = 40.337, p < 0.001; Table II). The primary contributor to social participation restriction was found to be resilience. Furthermore, it was observed that older age, lower monthly family income, and decreased self-care ability were associated with greater limitations on social participation. Notably, resilience exhibited a significant correlation with social participation restriction, irrespective of age, family income per month, and self-care ability. However, the independent effect, positive coping tendency, and the interaction term between resilience and positive coping tendency did not yield significant results in predicting social participation restriction. The variables that showed significance in univariate analyses, namely family income per month, onset time of stroke, resilience, and the interaction term between resilience and positive coping tendency, were included in the multivariate linear regression analysis (Table II). Both family income per month and resilience exhibited a significant impact on the prediction of social participation satisfaction. However, these 2 variables explained only a modest 8.3% of the variance in social participation satisfaction (F = 10.739, p < 0.001). Specifically, higher level of resilience and family income was strongly associated with higher satisfaction with social participation.
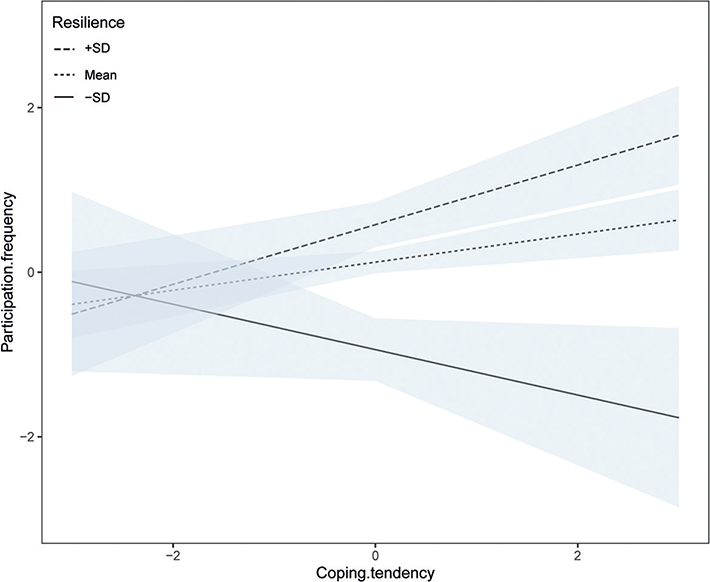
Fig. 2. Relationship between social participation and positive coping tendency at different levels of resilience.
DISCUSSION
This study examined the association between social participation, resilience, and positive coping tendency in stroke survivors in China. A noteworthy results was the significant association between resilience and various aspects of social participation, including frequency, restriction, and satisfaction, independent of significant demographics, clinical information, and coping strategies. This finding holds significance, as it implies that resilience may serve as a protective factor in enhancing both objective and subjective dimensions of social participation in individuals with stroke. The concept of resilience pertains to a good adaptation process in the face of adversity or stress (18). Previous research has demonstrated that individuals exhibiting higher level of resilience tend to recover more rapidly from adverse exposure by employing internal or external resources, thereby reducing the harmful effect of stressors (21). A study suggests that stroke survivors with higher level of resilience are characteristic of the employment of social support, access to spirituality, and goal setting (34). Consequently, stroke survivors with higher level of resilience tend to resist negative emotions caused by the inability to adapt to the dramatic changes in their lives following the onset of stroke. Furthermore, they are able to more quickly and effectively accommodate to changed condition where a return to premorbid functioning may not be possible. These individuals are inclined to continue their involvement in meaningful activities, as well as uphold their social functioning and overall quality of life over the course of many years (35, 36). In addition, the relationship of resilience and subjective social participation suggests that, despite restricted social participation faced by stroke survivors, resilience has the potential to enhance positive experiences of participation. It is evident that the Chinese version of CD-RISC identifies optimism as one of the key dimensions for evaluating resilience (30). Previous research has shown that adopting an optimistic lifestyle enables individuals to continuously cultivate their capacity for learning and subsequently construct a renewed sense of self-identity (37). Hence, it is plausible that stroke survivors exhibiting a greater degree of resilience are more inclined to achieve psychological adjustment and construct the benefits when re-engaging in society. The most effective approaches to enhance social participation following stroke remain unclear. Thus, the current study may provide insights into resilience-targeted interventions that can raise both objective and subjective levels of social participation among stroke survivors.
The second important finding refers to the moderating effect of resilience on the relationship between positive coping tendency and social participation frequency. The results of bivariate linear correlation analysis indicate a significant relationship between resilience and positive coping tendency, which is accordant with previous studies (38, 39). This finding suggests that individuals with higher levels of resilience are more likely to employ proactive coping strategies and less likely to rely on reactive coping strategies (40). Moreover, a significant correlation was observed between a higher inclination towards positive coping strategies and enhanced frequency of participation, as well as decreased restrictions on participation, consistent with previous research (15, 17, 41), suggesting that the manner in which individuals cope with stressful events impacts their social participation behaviours. However, no association was found between positive coping tendencies and satisfaction with social participation. While stroke survivors can potentially benefit from employing positive coping strategies to reintegrate into society, the availability of a satisfactory experience remains a separate concern. The current study observed that positive coping tendency exhibited a positive correlation with social participation frequency among individuals with a high level of resilience. Conversely, this correlation was found to be negative for individuals with a low level of resilience. In essence, the findings suggest that a positive coping tendency would be more beneficial for stroke survivors with higher resilience in their reintegration into society, while it may have adverse effects on stroke survivors with lower resilience. Hence, a hierarchical approach to intervention should be adopted in order to enhance the frequency of societal participation among stroke survivors in clinical practice. More specifically, it is found that targeting coping strategies is more effective for stroke survivors with high levels of self-reported resilience, whereas interventions aimed at enhancing resilience should precede coping strategy interventions for stroke survivors with low levels of resilience.
This study not only highlights resilience and coping strategies, but also identifies various predictors of objective social participation. The level of the frequency and restriction of participation among stroke survivors in this study are largely consistent with prior research (42, 43). Moreover, a strong correlation was observed between higher self-care ability and decreased social participation restriction, which is in line with previous studies (44, 45). Therefore, addressing physical function becomes crucial in enhancing social participation. In addition, advancing age was found to be linked to decreased participation frequency and increased participation restriction, which aligns with previous research (17, 46). Low family income may pose a potential risk to the social participation of individuals who have had a stroke. Therefore, it is imperative to prioritize elderly patients, those with low family income, and impaired self-care abilities in both social and medical practices in order to enhance their social participation. In terms of subjective social participation, the score of social participation satisfaction in the current study was accordant with a previous study conducted in patients 3 months post-stroke (47). Despite facing significant limitations in social participation and a low frequency of engagement, the level of satisfaction reported was moderate. Hence, individuals were still able to acquire positive participation experiences despite their restricted involvement in social activities. This finding can be reinforced by insights from previous research, which suggested that the quality of social engagement outweighed the quantity of activities in which subjects participated (48–50). In addition, it is plausible that the factors affecting objective and subjective social participation differ, and the account of family income per month and resilience for social participation satisfaction was obviously inadequate in this study. Further research is needed to investigate the predictors of subjective social participation in the future. Social participation, in the context of long-term disability and irreversible changes, encompasses a dynamic process that involves maintaining a balance between self-identity, self-existence, and self-satisfaction among stroke survivors (51). Consequently, it is crucial to prioritize stroke patients’ experiences and feelings, including their sense of belonging and achievement, alongside increasing their engagement in various activities. This approach can contribute to their mental well-being and overall satisfaction.
There are several limitations in the current study. The first pertains to the cross-sectional study design, which precludes the assessment of causality and directionality. The second limitation arises from the potential bias in the study sample, as it consists primarily of respondents from 3 neural rehabilitation hospitals. This implies that the stroke patients included in the study exhibit relatively severe functional impairment and limited social participation. To address this issue, the study included participants who have experiences of social participation, as this selection criterion is facilitated by the medical insurance policy in Shanghai, which restricts each rehabilitation hospital stay to a duration of less than 3 weeks. Prior to completing questionnaires, participants were assessed based on their responses on their experiences of social participation, specifically during their time residing at home. The finding that the mean score of USER-P aligned with previous research (42, 43) suggests that the current study sample may not possess significant bias. However, it is important to acknowledge the potential impact of the SARS-CoV-2 (COVID-19) pandemic on social participation levels. The strict quarantine management during the pandemic could, to some degree, limit participants’ outdoor activities and reduce their social participation. In addition, it should be noted that the predictors identified in this study did not fully explain the variance in social participation satisfaction. The predictors for subjective social participation may be different from those of objective social participation, which needs further research.
In conclusion, the identification of a potentially modifiable psychological factor (resilience) that positively influences both objective and subjective social participation provides insights into possible psychological interventions for stroke survivors. Furthermore, the moderating effect of resilience on the relationship between positive coping tendencies and participation frequency also presents an opportunity to enhance the efficacy of positive coping tendencies in promoting social participation.
ACKNOWLEDEGEMENTS
We express our gratitude to Kaiqiang Sun for helping to improve the manuscript.
This research was funded by The National Natural Science Foundation of China (82202816) and Shanghai Health Promotion Commission Office and Shanghai Health Commission (JKKPZX-2022-A25). The funders had no role in study design, data collection and analysis, or decision to publish.
REFERENCES
- Wu SM, Wu B, Liu M, Chen ZM, Wang WZ, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol 2019; 18: 394–405.
- “China Stroke Prevention and Control Report 2019” Writing Group. Summary of “China Stroke Prevention and Control Report 2019”. Chin J Cerebrovasc Dis 2020; 17: 272–281.
- O’Sullivan TL, Fahim C, Gagnon E. Asset literacy following stroke: implications for disaster resilience. Disaster Med Public Health Prep 2018; 12: 312–320.
- Bourassa KJ, Memel M, Woolverton C, Sbarra DA. Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging Ment Health 2017; 21: 133–146.
- Silva AS, de Sousa MSA, da Silva EV, Galato D. Social participation in the health technology incorporation process into Unified Health System. Rev Saude Publica 2019; 53: 109.
- Verberne DPJ, Post MWM, Köhler S, Carey LM, Visser-Meily JMA, van Heugten CM. Course of social participation in the first 2 years after stroke and its associations with demographic and stroke-related factors. Neurorehabil Neural Repair 2018; 32: 821–833.
- Zhang LF, Yan TB, You LM, Gao Y, Li K, Zhang CB. Functional activities and social participation after stroke in rural China: a qualitative study of barriers and facilitators. Clin Rehabil 2018; 32: 273–283.
- Goh HT, Tan MP, Mazlan M, Abdul-Latif L, Subramaniam P. Social participation determines quality of life among urban-dwelling older adults with stroke in a developing country. J Geriatr Phys Ther 2019; 42: E77–E84.
- Zhang LF, Sui MH, Yan TB, You LM, Li K, Gao Y. A study in persons later after stroke of the relationships between social participation, environmental factors and depression. Clin Rehabil 2017; 31: 394–402.
- Whiteneck G, Dijkers MP. Difficult to measure constructs: conceptual and methodological issues concerning participation and environmental factors. Arch Phys Med Rehabil 2009; 90: S22–35.
- Häggström A, Lund ML. The complexity of participation in daily life: a qualitative study of the experiences of persons with acquired brain injury. J Rehabil Med 2008; 40: 89–95.
- Woodman P, Riazi A, Pereira C, Jones F. Social participation post stroke: a meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disabil Rehabil 2014; 36: 2031–2043.
- Manning M, MacFarlane A, Hickey A, Galvin R, Franklin S. ‘I hated being ghosted’-The relevance of social participation for living well with post-stroke aphasia: qualitative interviews with working aged adults. Health Expect 2021; 24: 1504–1515.
- Demers L, Robichaud L, Gélinas I, Noreau L, Desrosiers J. Coping strategies and social participation in older adults. Gerontology 2009; 55: 233–239.
- Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav 1978; 19: 2–21.
- Vecchia CD, Préau M, Haesebaert J, Viprey M, Rode G, Termoz A, et al. Factors associated with post-stroke social participation: a quantitative study based on the ICF framework. Ann Phys Rehabil Med 2023; 66: 101686.
- Li YX, Zhang W, Ye MM, Zhou LS. Perceived participation and autonomy post-stroke and associated factors: an explorative cross-sectional study. J Adv Nurs 2021; 77: 1293–1303.
- American Psychology Association Help Center. The road to resilience: what is resilience? [EB/OL]. [cited 2017 Jan 6]. Available from: http://www.apa.org/helpcenter/roadresilience.aspx,2011
- Vannini P, Gagliardi GP, Kuppe M, Dossett d ML, Donovan NJ, Gatchel JR, et al. Stress, resilience, and coping strategies in a sample of community-dwelling older adults during COVID-19. J Psychiatr Res 2021; 138: 176–185.
- Liu ZH, Zhou X, Zhang W, Zhou LS. Resilience is an independent correlate of the course of quality of life in patients with first-ever ischemic stroke. Int Psychogeriatr 2021; 33: 567–575.
- Zhou X, Liu ZH, Zhang W, Zhou LS. Resilience is associated with post-stoke depression in Chinese stroke survivors: A longitudinal study. J Affect Disord 2020; 273: 402–409.
- Zhang W, Liu ZH, Zhou X, Zhou LS. Resilience among stroke survivors: a cohort study of the first 6 months. J Adv Nurs 2020; 76: 504–513.
- Liu ZH, Zhou X, Zhang W, Zhou LS. Resilience and its correlates among first ischemic stroke survivors at acute stage of hospitalization from a tertiary hospital in China: a cross-sectional study. Aging Ment Health 2020; 24: 828–836.
- Chinese Medical Association. Clinical guide for diagnosis and treatment: the archives of 379 neurology. Beijing: People’s Medical Publishing House; 2006.
- Guo QH. Neuropsychological assessement (3th edition). Shanghai: Shanghai Science and Technology Press; 2020: p. 72–79.
- van der Zee CH, Priesterbach AR, van der Dussen L, Kap A, Schepers VPM, Visser-Meily JMA, et al. Reproducibility of three self-report participation measures: the ICF Measure of Participation and Activities Screener, the Participation Scale, and the Utrecht Scale for Evaluation of Rehabilitation-Participation. J Rehabil Med 2010; 42: 752–757.
- Post MWM, van der Zee CH, Hennink J, Schafrat CG, Visser-Meily JMA, van Berlekom SB. Validity of the Utrecht scale for evaluation of rehabilitation-participation. Disabil Rehabil 2012; 34: 478–485.
- de Graaf JA, Volkers EJ, Schepers VPM, Visser-Meily JMA, Post MWM. Validity of the Utrecht scale for evaluation of rehabilitation-participation restrictions scale in a hospital-based stroke population 3 months after stroke. Top Stroke Rehabil 2022; 29: 516–525.
- Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson resilience scale (CD-RISC) with Chinese people. Soc Behav Pers 2007; 35: 19–30.
- Yu XN, Lau JT, Mak WW, Zhang J, Lui WW, Zhang J. Factor structure and psychometric properties of the Connor Davidson Resilience Scale among Chinese adolescents. Compr Psychiatry 2011; 52: 218–224.
- Wu Z, Liu Y, Li X, Li X. Resilience and associated factors among mainland Chinese women newly diagnosed with breast cancer. PLoS One 2016; 11: e0167976.
- Xie YN. A preliminary study on the reliability and validity of the simple coping style scale. Chin J Clin Psychol 1998; 02: 53–54.
- Liu Z, King M. The influencing factors and coping styles of mental health stress responses of stroke caregivers. Work 2021; 69: 499–513.
- Price P, Kinghorn J, Patrick R, Cardell B. “Still there is beauty”: one man’s resilient adaptation to stroke. Scand J Occup Ther 2012; 19: 111–117.
- Terrill AL, Molton IR. Frequency and impact of midlife stressors among men and women with physical disability. Disabil Rehabil 2019; 41: 1760–1767.
- Silverman AM, Molton IR, Alschuler KN, Ehde DM, Jensen MP. Resilience predicts functional outcomes in people aging with disability: a longitudinal investigation. Arch Phys Med Rehabil 2015; 96: 1262–1268.
- Udey MC. Uncertainty and Optimism. J Invest Dermatol 2021; 141: 1–2.
- Liu Y, Hou TY, Gu HJ, Wen J, Shao XQ, Xie YW, et al. Resilience and anxiety among healthcare workers during the spread of the SARS-CoV-2 Delta variant: a moderated mediation model. Front Psychiatry 2022; 13: 804538.
- Lin J, Ren YH, Gan HJ, Chen Y, Huang YF, You XM. Factors associated with resilience among non-local medical workers sent to Wuhan, China during the COVID-19 outbreak. BMC Psychiatry 2020; 20:417.
- Meye BC. Oping with severe mental illness: relations of the Brief COPE with symptoms, functioning, and well-being. J Psychopathol Behav Assess 2001; 23: 265–277.
- Palmes MS, Trajera SM, Ching GS. Relationship of coping strategies and quality of life: parallel and serial mediating role of resilience and social participation among older adults in Western Philippines. Int J Environ Res Public Health 2021; 18: 10006.
- Foley EL, Nicholas ML, Baum CM, Connor LT. Influence of environmental factors on social participation post-stroke. Behav Neurol 2019; 2019: 2606039.
- Silva SM, Corrêa JCF, Pereira GS, Corrêa FI. Social participation following a stroke: an assessment in accordance with the international classification of functioning, disability and health. Disabil Rehabil 2019; 41: 879–886.
- Pokryszko-Dragan A, Marschollek K, Chojko A, Karasek M, Kardyś A, Marschollek P, et al. Social participation of patients with multiple sclerosis. Adv Clin Exp Med 2020; 29: 469–473.
- Törnbom K, Persson HC, Lundälv J, Sunnerhagen KS. The impact of physical function on participation in the first year post-stroke. I Neurol Scand 2017; 135: 649–655.
- de Graaf JA, van Mierlo ML, Post MWM, Achterberg WP, Kappelle LJ, Visser-Meily JMA. Long-term restrictions in participation in stroke survivors under and over 70 years of age. Disabil Rehabil 2018; 40: 637–645.
- Groeneveld IF, Goossens PH, van Meijeren-Pont W, Arwert HJ, Meesters JJL, Rambaran Mishre AD, et al. Value-based stroke rehabilitation: feasibility and results of patient-reported outcome measures in the first year after stroke. J Stroke Cerebrovasc Dis 2019; 28: 499–512.
- van de Velde D, Coussens M, Baets SD, Sabbe L, Vanderstraeten G, Vlerick P, et al. Application of participation in clinical practice: key issues. J Rehabil Med 2018; 50: 679–695.
- Fallahpour M, Jonsson H, Joghataei MT, Nasrabadi AN, Tham K. “I am not living my life”: lived experience of participation in everyday occupations after stroke in Tehran. J Rehabil Med 2013; 45: 528–534.
- Dalemans RJ, de Witte L, Wade D, van den Heuvel W. Social participation through the eyes of people with aphasia. Int J Lang Commun Disord 2010; 45: 537–550.
- Hoffmann L, Völlm C, Bernard M, Fink A, Richter M, Dawal B. What does social participation mean? A qualitative study exploring the concept of participation from the perspectives of experts and parents. BMJ Open 2023; 13: e072684.