ORIGINAL REPORT
LONGER DAILY DURATION OF SUPERVISED REHABILITATION AFTER LAPAROSCOPIC SURGERY FOR COLORECTAL CANCER IMPROVES ACTIVITIES OF DAILY LIVING
Takuaki TANI, MMSc1,2, Shinobu IMAI, PhD2,3 and Kiyohide FUSHIMI, PhD1,2
From 1Tokyo Medical and Dental University Graduate School of Medical and Dental Sciences, 2Clinical Research Center National Hospital Organization and 3Tokyo University of Pharmacy and Life Sciences, Tokyo, Japan
Objective: To evaluate the effect of a supervised rehabilitation programme with longer hours per day on activities of daily living after laparoscopic surgery for colorectal cancer.
Design: This study represents retrospective observational use of nationwide administrative data.
Patients: Eligible patients (n = 8,633) were first diagnosed with colorectal cancer between 1 April 2017 and 31 March 2018, underwent laparoscopic-assisted colorectal resection, and began rehabilitation within 3 days of surgery.
Methods: Patients underwent a long (40 min or more) or short (less than 40 min) supervised rehabilitation programme, defined as rehabilitation under physiotherapist and occupational therapist supervision. The main outcome measure was improvement in activities of daily living from postoperative day 0 to day 14 using Nursing Need Degree.
Results: Patients who underwent longer daily supervised rehabilitation (n = 7,173) showed greater improvements in activities of daily living at 14 days after laparoscopic surgery than patients who underwent shorter daily supervised rehabilitation (n = 1,460) (odds ratio (95% confidence interval; 95% confidence interval): 1.42 (1.22–1.64), p < 0.001). The rate of postoperative complications did not differ between groups.
Conclusion: Longer daily supervised rehabilitation for colorectal cancer improves activities of daily living after laparoscopic surgery.
LAY ABSTRACT
Post-operative rehabilitation is performed for muscle weakness, decreased range of motion of joints, and pain caused by surgery, in order to promote recovery and help patients with activities of daily living after surgery. Supervised rehabilitation provides the patient with a programme based on their postoperative condition and background. Laparoscopic surgery for colorectal cancer, the focus of this study, is minimally invasive and results in less postoperative decline than other surgeries. The aim of this study was to evaluate the effect of a supervised rehabilitation programme with longer daily duration on the ability of patients (n = 8,633) to perform activities of daily living after laparoscopic surgery for colorectal cancer. The results show that engaging in daily supervised rehabilitation for longer duration (40 min or more) after laparoscopic surgery for colorectal cancer improves activities of daily living.
Key words: supervised rehabilitation; colorectal cancer; laparoscopic surgery; activities of daily living.
Citation: J Rehabil Med 2022; 54: jrm00304. DOI: https://dx.doi.org/10.2340/jrm.v54.1510
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: June 17, 2022 Epub ahead of print: July 11, 2022; Published: Jul 25, 2022
Correspondence address: Kiyohide Fushimi, Tokyo Medical and Dental University Graduate School of Medical and Dental Sciences, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8510, Japan. E-mail: kfushimi.hci@tmd.ac.jp.
Colorectal cancer is the fourth most common cancer and the fifth leading cause of cancer-related deaths worldwide, with an estimated 1,096,601 people (6.1% of all cancers) diagnosed and 551,265 deaths (5.8% of all cancers) in 2018 (1).
Currently, laparoscopic surgery is the first-choice surgical treatment for patients with colorectal cancer, and a comprehensive programme to promote postoperative recovery is the mainstream of postoperative treatment (2, 3). The objective of comprehensive recovery programmes after surgery is to facilitate rapid recovery of activities of daily living (ADL) and to maintain quality of life for inpatients. Enhanced recovery programmes after surgery (ERAS) are multimodal programmes that decrease postoperative complications and promote early recovery by diminishing the effects of surgical and other interventional techniques, trauma, and the inherent stress response of the body (4–7). Randomized controlled trials have demonstrated that a comprehensive ERAS programme implemented after laparoscopic surgery for colon cancer is the best perioperative strategy (8, 9), providing more rapid recovery and/or shortened hospital stays after surgery (10, 11). According to the guidelines for ERAS, mobilization from the early postoperative period is an essential component of multimodality rehabilitation for enhanced recovery, and is associated with successful recovery of ADL (12). Several studies have shown that early postoperative rehabilitation is effective for good outcomes after laparoscopic surgery (13, 14).
Postoperative supervised rehabilitation (SVR) for cancer patients, including the ERAS component, aims to maximize physical function and enhance recovery. In general, patients who undergo SVR are under the supervision of qualified medical professionals, including physiotherapists and occupational therapists (15). This rehabilitation promotes patient’s confidence and determination to achieve the recommended exercise goals with appropriate risk management (16). An SVR programme may include calisthenics, muscle training, and aerobic exercise to improve strength, balance, and coordination (17). Another benefit of rehabilitation is the prevention of complications. A previous study of early rehabilitation for cancer inpatients revealed that rehabilitation could prevent complications in patients undergoing surgery (18). Another study on SVR for cancer showed that exercise programmes improved postoperative physical functioning compared with standard care (16, 19). However, few studies have evaluated postoperative SVR alone, and the evidence for the benefit of SVR after laparoscopic colon surgery needs to be clarified.
Increasing the duration of rehabilitation per day may contribute to improvements in ADL if SVR is effective after laparoscopic surgery for colorectal cancer. Systematic reviews on exercise and cancer rehabilitation have generally shown that exercise prescription increases the intensity or duration of rehabilitation activities during the intervention period. However, many of these studies have not focused on the effects of different rehabilitation durations per day; therefore the impact of different daily rehabilitation durations on cancer patients is unknown (20, 21).
The study hypothesis was that engaging in SVR for longer durations after laparoscopic surgery for colorectal cancer promotes the recovery of ADLs in hospitalized patients. To test this hypothesis, this study evaluated the effect of an SVR programme with longer daily durations on the recovery of ADLs after laparoscopic surgery for colorectal cancer.
METHODS
Study design
This was an observational retrospective cohort study using data from a nationwide database in Japan, the Diagnosis Procedure Combination (DPC) database, which records data from acute care inpatients. All procedures followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Patient selection
Data for all inpatients who had undergone laparoscopic-assisted colectomy for colorectal cancer between 1 April 2017 and 31 March 2018 was extracted from the database. Patients diagnosed with colorectal cancer (International Classification of Diseases, 10th Revision (ICD-10) codes C18-20) at stage I, II or III for the first time, aged 18 years and over, who were discharged home and started rehabilitation within 3 days were included. The data for patients who had died after hospitalization were excluded. Also excluded were the data for patients with hospital stays > 90 days, because rehabilitation costs are not reimbursed beyond 90 days for the eligible patients in this study.
Data source
The DPC data was established to evaluate the fixed payment system for medical expenses in Japan. The database contains data on approximately half of Japan’s acute care patients and is representative of acute care hospital data in Japan. Details of the database are described elsewhere (22, 23). The database includes the following patient data: age, sex, smoking index, primary diagnoses, admission diagnosis, comorbidity on admission, complications during hospitalization recorded with ICD-10 codes, length of hospital stay (LOS), Barthel Index, cancer stage, Nursing Need Degree (NND), and hospital location. Medical procedure data included daily records of surgeries, prescriptions, and rehabilitation.
Variables
Daily SVR duration was defined as the total duration per day of rehabilitation conducted by a therapist for inpatients with cancer. In Japan, rehabilitation is reimbursed on a unit basis by the health system. One unit consists of 20 min of rehabilitation. For each patient, the total time of rehabilitation (in min) during hospitalization was divided by the LOS. Patients were divided into 2 groups based on the mean min of daily rehabilitation they engaged in: less than 40 min (short SVR) and 40 min and over (long SVR).
Patients were also stratified into 3 groups according to age: ≤ 50, 51–75 and > 75 years, because the incidence of colon cancer increases from approximately 50 years of age (24). Body mass index (BMI) was calculated at admission, based on the patient’s height and weight. The BMI was classified on the basis of the modified World Health Organization (WHO) classifications of < 18.5 kg/m2 (underweight), 18.5–24.9 kg/m2 (normal weight), and 25.0–29.9 kg/m2 (overweight) (25). The smoking index was used as a binary variable (1 = smoking, 0 = non-smoking). The Charlson Comorbidity Index (CCI) was calculated based on Quan’s protocol (26, 27).
Medication data were extracted, including administration of acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), narcotic analgesics, direct oral anticoagulants (DOACs) and antiemetic agents, as binary variables.
Outcome measurement
As the primary outcome, ADLs were measured using the NND, including 7 items: rolling-over, transfer, oral hygiene, dietary intake, dressing, followed instructions, and risk behaviour. Rolling-over, transfer, dietary intake, and dressing were assigned a score of 0 to 1 or 2 (e.g. “without assistance”, “some assistance”, “full assistance”) depending on patient condition. Oral hygiene, followed instructions, and risk behaviour were assigned a score of 0–1 (e.g. “without assistance”, “full assistance” or “yes”, “no”) (28). Individual scores were summed for a total ADL score, with a total value of 11. Change in ADL, represented by the difference in the score between day 0 and day 14 after surgery, was calculated as the primary outcome. Changes in ADL were classified into 2 categories: more than 1 indicated an improvement, and 1 or less indicated no improvement. The ADL score calculated on day 0 before SVR began was used as a baseline variable, and patients were divided into 3 groups accordingly (0, complete; 1–10, mild; 11, severe). Secondary outcomes were LOS and postoperative complications. The LOS was divided into the following categories, following the overall distribution: ≤ 14, 15–21, 22–28, and ≥ 29 days. Postoperative complications were defined using the ICD-10, and included pneumonia (J12–J18) and ileus (K560, K562–K567, K913).
Statistical methods
Baseline characteristics were analysed according to the daily duration of SVR (short or long). The mean±standard deviation (SD) and standardized mean difference (SMD) were used to describe continuous variables. Categorical variables were described using counts, percentages, and SMD. Inverse probability weighting (IPTW) was used to minimize the selection bias (29). IPTW is a method for estimating the mean treatment effect. Weighting by the inverse probability that a subject receives treatment creates a composite sample where treatment assignment is independent of the measured baseline covariate.
Propensity scores (PS) were generated by logistic regression modelling to predict the probability of patients undergoing short and long SVR. IPTW was calculated according to the baseline weight of each patient in both SVR groups. After weighting of baseline characteristics, d-values were calculated and all variables that returned a d < 0.1 were checked.
As a primary analysis, a χ2 test was performed to assess the differences in ADL, LOS, and postoperative complications between the 2 groups after weighting using IPTW.
To provide robust results of the impact of daily SVR duration on ADLs in the 2 groups, a multilevel logistic regression was conducted. The dependent variables included in the regression model were SVR, age, sex, smoking, BMI, CCI, cancer stage, and use of drugs such as acetaminophen, NSAIDs, narcotic analgesics, DOACs, and antiemetics.
As mentioned above, long daily SVR was defined as an SVR duration exceeding 40 min. However, as this definition is somewhat imprecise, Fig. 2 lists the SMD for daily SVR durations from postoperative days 0 to 14 to identify further differences in daily durations between SVR groups. A generalized linear model was used to examine the differences in daily SVR durations between the 2 groups for SVR durations as the dependent variable. The independent variables we used for this model were SVR duration (long or short), rehabilitation days (postoperative days 0 to 14), and interactions between variables. The generalized linear model assumes a Gaussian distribution and a stationary function as the link function.
All tested hypotheses had a 2-sided significance level of < 0.05. Statistical analyses were performed using R statistical software version 3.3.2.
Ethical considerations
The requirement for informed consent was waived because of the anonymous nature of the data. Study approval was obtained from the institutional review board of Tokyo Medical and Dental University.
RESULTS
A total of 10,006 inpatients who underwent colorectal cancer and rehabilitation within 3 days of laparoscopic-assisted colectomy were identified during the study period. The study excluded the data of 537 patients who had died during hospitalization and 836 patients who had stayed at the hospital for 90 days or more. Thus, the data for 8,633 patients were included in the study. The number of patients was 7,173 (83.1%) in the short SVR group and 1,460 (16.9%) in the long SVR group (Fig. 1).
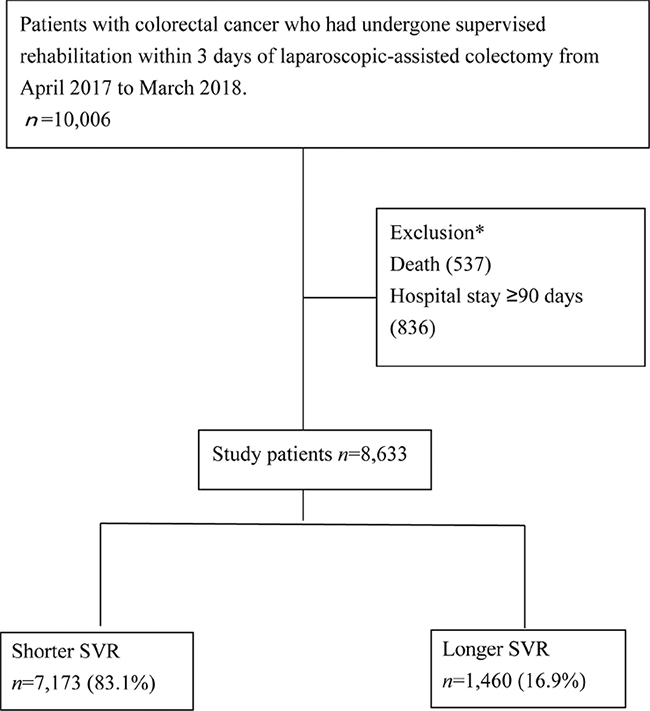
Fig. 1. Participant selection. SVR: supervised rehabilitation.
*Numbers are overlapping.
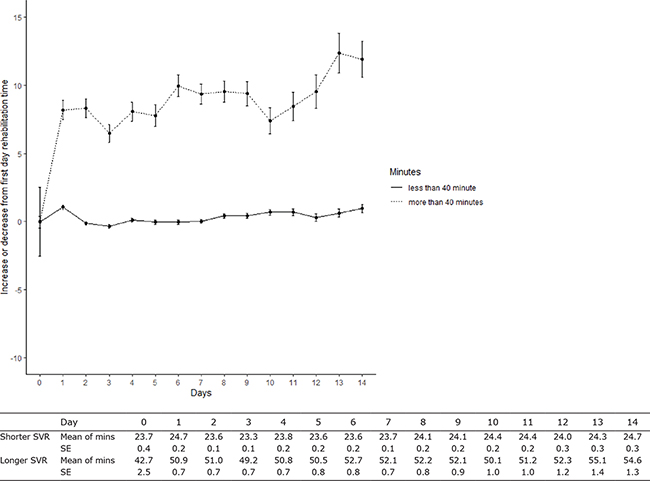
Fig. 2. Mean differences in rehabilitation duration per day from day 1 to 14 after surgery, means of rehabilitaion duration per day, and the standard error (SE) of rehabilitaion duration per day. SVR: supervised rehabilitation.
Table I shows the baseline characteristics of the unweighted and weighted values using IPTW. The mean daily duration of rehabilitation was longer in the long SVR group than in the short SVR group in the unweighted (mean (SD): 50.28 (12.5) vs 23.31 (5.37), SMD = 2.80) and weighted analysis (49.67 (12.0) vs 23.34 (5.4), SMD = 2.83). The total duration of rehabilitation was longer in the long SVR group than in the short SVR group in the unweighted (mean (SD): 304.9 (81.2) vs 640.7 (178.6), SMD = 2.42) and weighted analysis (305.2 (81.4) vs 636.1 (171.1), SMD = 2.43). Rehabilitation days were longer in long SVR than in short SVR group in the unweighted (mean (SD): 14.77 (10.72) vs 16.0 (11.3), SMD = 0.11) and weighted analysis (14.74 (10.7) vs 16.19 (11.70), SMD = 0.11). After weighting with IPTW, there were no differences in baseline characteristics between the 2 SVR groups. As all covariate SMDs between the 2 groups were < 0.1 after IPTW weighting, the 2 groups were considered to be balanced.
| Unweighted | Weighted using IPTW | ||||||||
| Shorter SVR | Longer SVR | SMD* | |||||||
| n = 7,173 | n = 1,460 | Shorter SVR | Longer SVR | SMD* | |||||
| Supervised rehabilitation, min, mean (SD) | 23.31 | (5.4) | 50.28 | (12.5) | 2.80 | 23.34 (5.4) | 49.67 (12.0) | 2.83 | |
| Rehabilitation total duration, min, mean (SD) | 304.9 | (81.2) | 640.7 | (178.6) | 2.42 | 305.2 (81.4) | 636.1 (174.2) | 2.434 | |
| Rehabilitation days, min, mean (SD) | 14.77 | (10.74) | 16.00 | (11.32) | 0.11 | 14.74 (10.7) | 16.19 (11.70) | 0.112 | |
| Age, year n, (%) | 0.09 | 0.02 | |||||||
| ≤ 50 | 336 | (4.7) | 85 | (5.8) | (4.9) | (5.0) | |||
| 51–74 | 4,036 | (56.3) | 864 | (59.2) | (56.7) | (55.7) | |||
| > 75 | 2,801 | (39.0) | 511 | (35.0) | (38.4) | (39.4) | |||
| Sex, female, n, (%) | 2,980 | (41.5) | 626 | (42.9) | 0.03 | (41.7) | (41.8) | 0.01 | |
| Smoker, n, (%) | 3,278 | (45.7) | 671 | (46.0) | 0.01 | (45.7) | (45.6) | 0.00 | |
| BMI, weight n, (%) | 0.08 | 0.04 | |||||||
| –18.5 | 650 | (9.3) | 148 | (10.4) | (9.3) | (9.1) | |||
| 18.5–24.9 | 4,631 | (66.0) | 895 | (62.6) | (64.0) | (64.1) | |||
| 25–29.9 | 1,452 | (20.7) | 314 | (22.0) | (20.4) | (19.6) | |||
| 30 | 282 | (4.0) | 72 | (5.0) | (4.1) | (4.7) | |||
| NA | 158 | (2.2) | 31 | (2.1) | (2.2) | (2.5) | |||
| Charlson Comorbidity Index, n, (%) | 0.14 | 0.07 | |||||||
| 0 | 3,586 | (51.2) | 824 | (57.1) | (51.0) | (52.3) | |||
| 1 | 2,496 | (35.6) | 453 | (31.4) | (34.5) | (32.8) | |||
| 2 | 923 | (13.2) | 165 | (11.4) | (12.2) | (13.3) | |||
| > 3 | 176 | (2.5) | 18 | (1.2) | (2.3) | (1.6) | |||
| Cancer stage, n, (%) | 0.12 | 0.01 | |||||||
| I | 2,239 | (31.2) | 517 | (35.4) | (32.0) | (32.5) | |||
| II | 2,191 | (30.5) | 471 | (32.3) | (30.6) | (30.5) | |||
| III | 2,743 | (38.2) | 472 | (32.3) | (37.3) | (37.0) | |||
| Postoperative ADL, n, (%) | 0.15 | 0.02 | |||||||
| Complete | 2,167 | (30.4) | 346 | (23.8) | (29.1) | (29.4) | |||
| Mild | 3,714 | (52.2) | 842 | (58.0) | (52.9) | (52.2) | |||
| Severe | 1,239 | (17.4) | 263 | (18.1) | (17.2) | (17.5) | |||
| NA | 53 | (0.7) | 9 | (0.6) | (0.7) | (0.8) | |||
| Acetaminophen, n, (%) | Day 0 | 935 | (13.0) | 214 | (14.7) | 0.05 | (13.3) | (12.7) | 0.02 |
| Day 1–3 | 1,105 | (15.4) | 201 | (13.8) | 0.05 | (15.2) | (16.1) | 0.03 | |
| Day > 4 | 600 | (8.4) | 100 | (6.8) | 0.06 | (8.1) | (8.0) | 0.01 | |
| NSAIDs, n, (%) | Day 0 | 446 | (13.2) | 96 | (14.2) | 0.02 | (14.0) | (14.1) | 0.00 |
| Day 1–3 | 2,398 | (33.4) | 471 | (32.3) | 0.03 | (33.3) | (34.9) | 0.03 | |
| Day > 4 | 1,638 | (22.8) | 280 | (19.2) | 0.09 | (22.2) | (20.4) | 0.04 | |
| Narcotic analgesic, n, (%) | Day 0 | 6,341 | (88.4) | 1,292 | (88.5) | 0.00 | (88.4) | (88.9) | 0.02 |
| Day 1–3 | 2,398 | (33.4) | 471 | (32.3) | 0.16 | (32.9) | (33.1) | 0.01 | |
| Day > 4 | 1,638 | (22.8) | 280 | (19.2) | 0.08 | (16.7) | (15.4) | 0.03 | |
| DOAC, n, (%) | Day 0 | 473 | (6.6) | 156 | (10.7) | 0.15 | (7.3) | (7.3) | 0.00 |
| Day 1–3 | 1,291 | (18.0) | 133 | (9.1) | 0.26 | (16.7) | (17.7) | 0.02 | |
| Day >4 | 398 | (5.5) | 77 | (5.3) | 0.01 | (5.5) | (5.3) | 0.01 | |
| Antiemetic, n, (%) | 5,818 | (81.1) | 1,216 | (83.3) | 0.06 | (81.4) | (81.7) | 0.01 | |
| *. SMD < 0.1 indicates good balance. ADL: activities of daily living; BMI: body mass index; DOAC: direct oral anticoagulants; NSAIDs: non-steroidal anti-inflammatory drug; SD: standard deviation; SMD: standardized mean difference; SVR: supervised rehabilitation; IPTW: inversed probability weighting. |
|||||||||
Table II shows the results for differences between the groups in ADL improvements, LOS, and postoperative complications. In terms of ADL improvements, weighted values differed between inpatients undergoing short SVR and those undergoing long SVR (17.1% vs 21.5%, SMD = 0.111, p < 0.001). Weighted LOS did not differ between the short SVR and long SVR groups (39.5% vs 38.6% for ≤ 14 days, 31.8% vs 35.1% for 15–21 days, 13.4% vs 11.4% for 22–28 days, and 15.3% vs 14.9% for ≥ 29 days; SMD = 0.022, p = 0.068), and neither did weighted postoperative complications (pneumonia: 0.0% vs 0.06%, SMD = 0.067, p = 0.127; ileus: 0.24% vs 0.25%, SMD=0.044, p = 0.396).
Table III shows the results of the multivariable logistic regression analysis of the differences in the degree of ADL improvement. ADL improvements were significantly associated with longer daily SVR durations (odds ratio (95% confidence interval (95% CI)): 1.42 (1.22–1.64), p < 0.001).
| Multivariable logistic regression | |||||||||||||||||||||||
| Odds ratio (95% CI) | p-value | ||||||||||||||||||||||
| Supervised rehabilitation | SVR short | Reference | < 0.001 | *** | |||||||||||||||||||
| SVR longer | 1.42 | (1.22 | 1.64) | ||||||||||||||||||||
| Age, years | ≤ 50 | Reference | |||||||||||||||||||||
| 51–74 | 1.23 | (0.92 | 1.68) | 0.169 | |||||||||||||||||||
| > 75 | 1.97 | (1.47 | 2.70) | < 0.001 | *** | ||||||||||||||||||
| Sex, female | 0.91 | (0.80 | 1.04) | 0.167 | |||||||||||||||||||
| Smoker | 1.04 | (0.91 | 1.19) | 0.535 | |||||||||||||||||||
| BMI | ≤ 18.5 | Reference | |||||||||||||||||||||
| 18.6–24.9 | 0.74 | (0.61 | 0.89) | < 0.001 | *** | ||||||||||||||||||
| 25–29.9 | 0.60 | (0.48 | 0.75) | < 0.001 | *** | ||||||||||||||||||
| > 30 | 1.36 | (1.00 | 1.83) | 0.045 | |||||||||||||||||||
| NA | 0.48 | (0.29 | 0.76) | 0.003 | *** | ||||||||||||||||||
| Charlson Index | 0 | Reference | |||||||||||||||||||||
| 1 | 1.04 | (0.91 | 1.18) | 0.559 | |||||||||||||||||||
| 2 | 1.10 | (0.92 | 1.31) | 0.292 | |||||||||||||||||||
| 3 | 0.92 | (0.60 | 1.35) | 0.669 | |||||||||||||||||||
| Cancer stage | I | Reference | |||||||||||||||||||||
| II | 1.18 | (1.02 | 1.36) | 0.030 | * | ||||||||||||||||||
| III | 1.23 | (1.07 | 1.42) | 0.004 | ** | ||||||||||||||||||
| Acetaminophen | day 0 | 1.31 | (1.10 | 1.54) | 0.002 | ** | |||||||||||||||||
| 1–3 | 0.85 | (0.71 | 1.01) | 0.065 | |||||||||||||||||||
| > 4 | 2.07 | (1.71 | 2.51) | < 0.001 | *** | ||||||||||||||||||
| NSAIDs | Day 0 | 0.87 | (0.72 | 1.04) | 0.132 | ||||||||||||||||||
| Day 1–3 | 0.89 | (0.77 | 1.03) | 0.110 | |||||||||||||||||||
| Day > 4 | 1.08 | (0.92 | 1.27) | 0.333 | |||||||||||||||||||
| Narcotic analgesic | Day 0 | 2.15 | (1.66 | 2.79) | < 0.001 | *** | |||||||||||||||||
| Day 1–3 | 1.21 | (1.07 | 1.38) | 0.003 | ** | ||||||||||||||||||
| Day 4 | 1.98 | (1.71 | 2.30) | < 0.001 | *** | ||||||||||||||||||
| DOAC | Day 0 | 1.33 | (1.08 | 1.63) | 0.007 | ** | |||||||||||||||||
| Day 1–3 | 0.94 | (0.79 | 1.10) | 0.427 | |||||||||||||||||||
| Day 4 | 1.24 | (0.98 | 1.56) | 0.072 | |||||||||||||||||||
| Antiemetic | Day 0 | 0.86 | (0.70 | 1.06) | 1.564 | ||||||||||||||||||
| *p < 0.05, **p < 0.01, ***p < 0.001. ADL: activities of daily living; BMI: body mass index; DOAC: direct oral anticoagulants; NSAIDs: non-steroidal anti-inflammatory drugs; SMD: standardized mean difference; SVR: supervised rehabilitation. |
|||||||||||||||||||||||
Fig. 2 shows the mean difference in daily SVR duration from postoperative days 0 to 14 stratified by SVR group. The duration of SVR per day in the long SVR group increased with time. In contrast, the duration of SVR per day in the short SVR group changed only slightly during the rehabilitation period.
Table IV shows the generalized linear model for daily SVR. There was a significant interaction between dates of rehabilitation and the SVR group, indicating that the amount of rehabilitation was higher in the longer SVR than in the shorter SVR, depending on the day of rehabilitation (coefficient (standard error; SE) = 0.22 (0.04), p < 0.001).
| Coefficient | SE | p-value | |
| Intercept | 23.73 | 0.12 | < 0.001*** |
| Rehabilitation days | 0.03 | 0.02 | 0.07 |
| SVR | 26.04 | 0.27 | < 0.001*** |
| Date of rehabilitation × SVR | 0.22 | 0.04 | < 0.001*** |
| ***p < 0.001. SE: standard error; SVR: supervised rehabilitation. |
|||
DISCUSSION
This study reveals that longer SVR after laparoscopic surgery in patients with colorectal cancer can promote postoperative ADL recovery compared with shorter SVR. Only 17% of the patients in this study underwent SVR of longer daily durations, but these patients showed greater improvements in ADL at 14 days after laparoscopic surgery than patients who underwent shorter daily SVR.
This study supports earlier findings that rehabilitation programmes can promote ADL recovery in patients with colorectal cancer (13, 16). Previous studies on postoperative rehabilitation in patients with colorectal cancer have mainly focused on effects related to early mobilization. The current study provides evidence of the effects of longer SVR as delivered in the healthcare system.
This study found that longer SVR is effective in promoting short-term recovery after colorectal cancer surgery. Previously, SVR was considered less beneficial for hospitalized patients undergoing laparoscopic surgery, regardless of the duration of the procedure, because of the generally short hospital stays following minimally invasive procedures. One systematic review on SVR for patients with colorectal cancer reported that rehabilitation could improve physical function in the short term (30). Moreover, longer hospital stays after surgery are associated with the development of pulmonary complications, skeletal muscle weakness, thromboembolism, and insulin resistance, for which rehabilitation is effective (12). Regarding the effects of postoperative rehabilitation, a review of cancer patients has shown that exercise improves cardiopulmonary function and decreases fatigue (14). The current study indicates that longer SVR can enhance short-term recovery of ADL compared with shorter SVR; however, the physiological effects of rehabilitation after colorectal cancer surgery are not entirely clear and need to be verified in future studies.
Another important finding of the current study is that the daily duration of SVR did not influence the occurrence of postoperative complications, such as ileus. Previous studies have investigated the impact of postoperative complications after surgery for colorectal cancer, and reported that the presence or absence of postoperative complications affects the short-term outcome of colorectal cancer resection (31). The fact that no difference in the occurrence of ileus has been observed, which has a significant impact on mortality, is important, as it highlights the safety of rehabilitation (32). Few studies have examined the appropriate amount and duration of postoperative SVR for cancer patients, and the secondary effects of rehabilitation require further clarification.
We assessed the average daily SVR duration of both groups from postoperative days 0 to 14, and found high variability in rehabilitation times in the long SVR group as the days passed. Longer SVR durations mean that that the amount of time patients spent exercising increased with each passing day, suggesting that the long SVR group might have needed to undergo more rehabilitation units because their recovery was deemed insufficient, or because hospitalization was prolonged. The advantage of SVR is that the rehabilitation activities can be tailored to the patient’s condition (15). It is thus possible that the fact that the mean number of rehabilitation sessions provided was higher in the long SVR group was a result of rehabilitation being tailored to the condition of the patients in this group.
Study limitations
This study has several limitations. The most important limitation is that the NND used for outcomes was used as an ADL assessment, although it has not been subjected to validation studies and its reliability is unclear. In addition, the assessment items were limited to ADLs around the hospital bed, which has a strong impact on the ceiling effect of the assessment. We did not have access to information on surgical methods and operation times, and could thus not take into consideration the severity of the surgery received by the patients in each rehabilitation group. Instead, the analyses were adjusted for postoperative ADLs and analgesics. In addition, because of the limitations of the patient database, we could not consider information related to ERAS, which involves factors such as food intake and catheter removal, and there may thus have been confounders that were not evaluated (33).
Conclusion
This study found that longer daily durations of SVR for colorectal cancer improved ADLs after laparoscopic surgery. We thus recommend SVR from the acute stage, with rehabilitation tailored to the patient’s condition.
ACKNOWLEDGEMENTS
We would like to thank the graduate students in our laboratory who helped with our analyses and gave us useful advice. We would also like to thank Editage (www.editage.jp) for English-language editing.
Conflicts of interest
The authors have no conflicts of interest to declare. The study founders had no influence on the design of the study, the interpretation of data, and the final conclusions drawn.
Funding
This study was supported by a Grant-in-Aid for Research on Policy Planning and Evaluation from the Ministry of Health, Labour and Welfare, Japan (20AA2005) and a Grant-in-Aid for Young Scientists (B) from the Japan Society for the Promotion of Science (JSPS KAKENHI, 21K10299).
REFERENCES
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68: 394–424.
- Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 2005; 6: 477–484.
- King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH, et al. Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 2006; 93: 300–308.
- Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 2005; 24: 466–477.
- Ni X, Jia D, Guo Y, Sun X, Suo J. The efficacy and safety of enhanced recovery after surgery (ERAS) program in laparoscopic digestive system surgery: A meta-analysis of randomized controlled trials. Int J Surg 2019; 69: 108–115.
- Sakamoto K, Tsukamoto R, Kawano S, Kawai M, Niwa K, Ishiyama S, et al. minimally invasive surgery for colorectal cancer. Juntendo Med J 2017; 63: 384–392.
- Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ 2001; 322: 473–476.
- Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 2009; 144: 961–969.
- Lee TG, Kang SB, Kim DW, Hong S, Heo SC, Park KJ. Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 2011; 54: 21–28.
- Rawlinson A, Kang P, Evans J, Khanna A. A systematic review of enhanced recovery protocols in colorectal surgery. Ann R Coll Surg Engl 2011; 93: 583–588.
- Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal Dis 2012; 14: 1009–1013.
- Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS((R))) Society Recommendations: 2018. World J Surg 2019; 43: 659–695.
- Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 2011; 254: 868–875.
- Vlug MS, Bartels SA, Wind J, Ubbink DT, Hollmann MW, Bemelman WA, et al. Which fast track elements predict early recovery after colon cancer surgery? Colorectal Dis 2012; 14: 1001–1008.
- Bartolo M, Zucchella C, Pace A, Lanzetta G, Vecchione C, Bartolo M, et al. Early rehabilitation after surgery improves functional outcome in inpatients with brain tumours. J Neurooncol 2012; 107: 537–544.
- Bousquet-Dion G, Awasthi R, Loiselle SE, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol 2018; 57: 849–859.
- Yadav R. Rehabilitation of surgical cancer patients at University of Texas M.D. Anderson Cancer Center. J Surg Oncol 2007; 95: 361–369.
- Fukawa Y, Kakuda W, Yoshida S, Zenta M, Itano O, Kiko R, et al. Clinical Impact of the introduction of an early rehabilitation protocol on infectious complications in patients after gastrointestinal cancer surgery. Prog Rehabil Med 2019; 4: 1–9.
- Van Vulpen JK, Velthuis MJ, Steins Bisschop CN, Travier N, Van Den Buijs BJ, Backx FJ, et al. Effects of an Exercise Program in Colon Cancer Patients undergoing Chemotherapy. Med Sci Sports Exerc 2016; 48: 767–775.
- Spence RR, Heesch KC, Brown WJ. Exercise and cancer rehabilitation: a systematic review. Cancer Treat Rev 2010; 36: 185–194.
- Galvao DA, Newton RU. Review of exercise intervention studies in cancer patients. J Clin Oncol 2005; 23: 899–909.
- Chikuda H, Yasunaga H, Horiguchi H, Takeshita K, Kawaguchi H, Matsuda S, et al. Mortality and morbidity in dialysis-dependent patients undergoing spinal surgery: analysis of a national administrative database in Japan. J Bone Joint Surg Am 2012; 94: 433–438.
- Matsuda S, Fujimori K, Fushimi K. Development of Casemix Based Evaluation System in Japan. Asian Pacific J Dis Manag 2010; 4: 55–66.
- Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin 2020; 70: 145–164.
- Deeks A, Lombard C, Michelmore J, Teede H. The effects of gender and age on health related behaviors. BMC Public Health 2009; 9: 213.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130–1139.
- Tomoya A, Naomi A, Kenshi H, Hiroshi T. Economic estimation of nursing services under the diagnostic procedure combination/per-diem payment system. J Nursing & Care 2013; 10.4172/2167-1168.S5-008: 1–5.
- Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015; 34: 3661–3679.
- Cramer H, Lauche R, Klose P, Dobos G, Langhorst J. A systematic review and meta-analysis of exercise interventions for colorectal cancer patients. Eur J Cancer Care (Engl) 2014; 23: 3–14.
- Law WL, Choi HK, Lee YM, Ho JW. The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol 2007; 14: 2559–2566.
- Grosso G, Biondi A, Marventano S, Mistretta A, Calabrese G, Basile F. Major postoperative complications and survival for colon cancer elderly patients. BMC Surg 2012; 12 Suppl 1: S20.
- Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 2011; 146: 571–577.