SHORT COMMUNICATION
EARLY MOBILIZATION OF PATIENTS WITH SUBARACHNOID HAEMORRHAGE: A NATIONAL SURVEY OF FRENCH INTENSIVE CARE UNITS
Adéla FOUDHAILI, PT1–3, Damien VITIELLO, PhD3 and Benjamin Glenn CHOUSTERMAN, MD, PhD2,4
From the 1Department of Physical Medicine and Rehabilitation, CHU Lariboisière, AP-HP, 2Université Paris Cité, Inserm, MASCOT, 3Université Paris Cité, Institut des Sciences du Sport-Santé de Paris and 4Department of Anesthesiology and Critical Care, CHU Lariboisière, AP-HP, Paris, France
Objective: To describe French intensive care unit practices regarding the mobilization of patients with subarachnoid haemorrhage.
Design: A cross-sectional nationwide survey study.
Subjects: Intensivists and physiotherapists or nurses from French intensive care units managing patients with subarachnoid haemorrhage.
Methods: An online questionnaire survey was distributed through the Neurocritical Care and Neuro Anesthesiology French Speaking Society.
Results: The response rate was 89%. Of these, 90% did not have a mobilization protocol for patients with subarachnoid haemorrhage. Sixteen percent of departments prohibited all forms of motor physiotherapy for a predefined period. Nineteen percent systematically prohibited out-of-bed mobilization, regardless of the severity of subarachnoid haemorrhage and in the absence of any complication, for a predefined period. The main factors that would delay or interrupt physiotherapy prescription were intracranial hypertension (79%), currently treated vasospasm (59%), and suspicion of vasospasm (44%). Ninety-one percent of the centres identified at least one complication that could be associated with standing upright. These mainly included decreased cerebral perfusion (71%), dislodged external ventricular or lumbar derivations (68%), and haemodynamic instability (65%).
Conclusion:
Mobilization of patients with subarachnoid haemorrhage is heterogeneous among French neuro-intensive care units and several barriers preclude improvement of mobilization practices. Interventional studies assessing mobilization practices, as well as education and training of staff, are crucial to ensure the proper management of patients with subarachnoid haemorrhage and to improve outcomes.
LAY ABSTRACT
No recommendations concerning the mobilization of patients with subarachnoid haemorrhage have been published to date. This survey examined mobilization practices of French intensive care units managing patients with subarachnoid haemorrhage. The study found that 90% of departments did not have a mobilization protocol for patients with subarachnoid haemorrhage and, consequently, the study found that practices were highly heterogeneous. It was also noted that there were concerns that early mobilization could be deleterious for these patients. Further studies are needed to determine the optimal modalities and timing of mobilization for these patients.
Key words: early ambulation; physical therapy modalities; subarachnoid haemorrhage; surveys and questionnaires.
Citation: J Rehabil Med 2024; 56: jrm17734. DOI: https://doi.org/10.2340/jrm.v56.17734.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Submitted: Jul 11, 2023; Accepted: Nov 7, 2023; Published: Jan 8, 2024
Correspondence address: Adéla Foudhaili, Department of Physical Medicine and Rehabilitation, CHU Lariboisière, AP-HP, University, 2 rue Ambroise Paré, Paris, F-75010 France. E-mail: adela.foudhaili@aphp.fr
Competing interests and funding: BC has been a member of an advisory board for Roche Diagnostics, has received speaking fees from Baxter, and has been awarded a research grant from Orion Pharma. The other authors have no conflicts of interests to declare.
Early mobilization in critically ill patients is a subject of increasing interest as it appears to be associated with improved outcomes (1–3). However, the best timing and modalities for mobilization remain uncertain, as studies investigating very early mobilization have shown a potential increase in adverse events in general intensive care unit (ICU) patients (4), and an association with a poorer functional prognosis in stroke patients (5).
To date, very few studies and only 1 randomized controlled trial have investigated the early mobilization of patients admitted to the ICU with subarachnoid haemorrhage (SAH) (6–11). Patients with SAH are often excluded from studies investigating early mobilization in patients with acute neurological injuries, as SAH is believed to differ greatly from other strokes (5). Indeed, several complications may worsen SAH patients’ outcomes, including cerebral vasospasm and delayed cerebral ischaemia (12), and their prevention often motivates prescription of bedrest. Guidelines published in 2023 for SAH management now suggest that implementing a mobilization protocol is reasonable (13). However, this is a moderate recommendation (class 2a) as no RCTs have been conducted in this specific setting. Consequently, the most efficient and safe way to mobilize patients with SAH has not been determined to date.
This lack of data in the literature promotes heterogeneity in practice. To date, no study has examined French mobilization practices for patients with SAH admitted to ICU. The French healthcare system is composed of closed ICUs, with specialized ICU physicians, while physiotherapists have general physiotherapy degrees, with or without postgraduate critical care training. Physiotherapy and mobilization are performed on a medical prescription.
In France, the range of incidence of SAH varies between 3 and 8/100,000 inhabitants. Overall mortality is approximately 40%, 70% of which occurs within the first week (14). Patients with SAH are admitted to 1 of 35 centres with neurosurgery, interventional neuroradiology, and neuro-intensive care departments. Our previous study reported a median (interquartile range) length of stay in the ICU of 15 (13–20) days (15). Regarding severity, our cohort had a median World Federation of Neurological Societies (WFNS) grade of 1 (1–3) and a median Fisher grade of 4 (4–4) (15).
The objectives of this study were to describe current practices in France and their determinants, and to identify the barriers associated with the implementation of early mobilization.
METHODS
The study was reported in accordance with the CROSS checklist (A Consensus-Based Checklist for Reporting of Survey Studies) (16).
Survey development
A cross-sectional survey by means of an online questionnaire was developed by a physiotherapist and a senior intensivist with in-depth knowledge and clinical experience of patients with SAH (AF and BGC).
The survey was tested by 5 intensivists and 4 physiotherapists, all of whom manage patients with SAH. Minor adjustments were made to improve clarity before sending the questionnaire.
The questionnaire comprised 18 items addressing the practices of mobilization of patients with aneurysmal SAH with few additional questions regarding the general organization of the ICU (Appendix SI). Mobilization was defined as all passive or active physiotherapy techniques, motor stimulation or installation at the edge of the bed, verticalization, transfer and installation in a chair, ambulation, and use of a cycle ergometer.
Population
The target population was the 35 French neuro-ICUs admitting patients with SAH on the list drawn up by the French Neuroradiology Society. Responses from intensive care units in which there was no physiotherapy provision were excluded, as were responses from foreign ICUs. The centres were asked to pair up an intensivist and a physiotherapist or nurse to answer the questionnaire. Responses were based on the responders’ clinical experience and beliefs.
Ethical considerations
Informed consent was assumed if responders completed and submitted their completed survey online. No patient data were collected. The names of the centres were used to estimate the response rate and to identify possible duplicates, but were removed when the data were analysed.
Survey administration
The questionnaire was designed via Google™ forms and distributed with the help of the Neurocritical Care and Neuro Anesthesiology French Speaking Society (ANARLF) through mailing campaigns and social networks. The survey was accessible online from February 2022 to June 2022. A general reminder was sent in April 2022, followed by individual reminders by telephone and/or e-mail in May 2022.
Statistical analysis
Data were analysed using descriptive statistics, reported as a number and percentages.
RESULTS
A total of 48 responses were collected. ICUs that did not take on patients with SAH (n = 2) were excluded. When multiple responses were received from the same centre, the first response was analysed (n = 8). Responses from foreign or unidentifiable centres (n = 7) were excluded. The study analysed responses from 31 ICUs out of the 35 targeted; a response rate of 89%.
The characteristics of respondents are shown in Table I. Most ICUs treated on average 50–100 patients with SAH annually (17/31, 55%). The most frequent patient/physiotherapist ratio was 5–10 patients (15/31, 48%) or 11–15 patients (11/31, 35%) for 1 physiotherapist. In most ICUs, patients deemed medically stable generally received 1 daily physiotherapy session (20/31, 65%).
Ninety percent of the departments surveyed (28/31) did not have a written mobilization protocol for patients with aneurysmal SAH. Sixteen percent (5/31) of departments prohibited all forms of motor physiotherapy for a predefined period (apart from the time needed for the aneurysm repair). Criteria delimiting this phase varied by services. Nineteen percent (6/31) of services systematically prohibited out-of-bed mobilization, regardless of SAH severity, and apart from any complication, for a 2–10-day period, and/or throughout the phase at risk of vasospasm. Sixteen percent (5/31) of services proscribed out-of-bed mobilization based on other criteria.
Fifty-eight percent (18/31) of services authorized chair installation within the first 5 days after aneurysm repair if allowed by clinical status, regardless of the WFNS grade. Twenty-six percent (8/31) of services systematically prohibited chair installation, whereas 13% (4/31) allowed it only for low-grade WFNS patients (Fig. 1). In 62% of services (16/26), there was no predefined maximum duration for chair-sitting sessions.
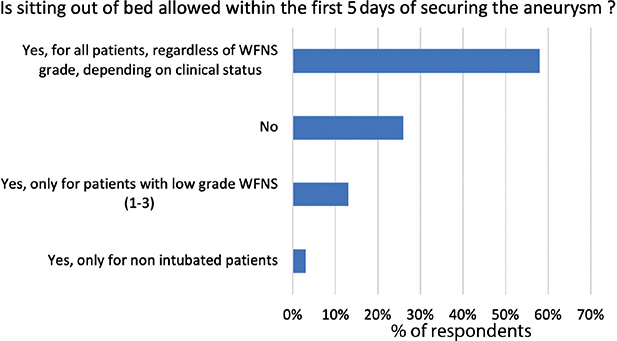
Fig. 1. Sitting out of bed in a chair within the first 5 days after securing the aneurysm. WFNS: World Federation of Neurological Societies.
The main factors that would delay or interrupt motor physiotherapy prescription were intracranial hypertension (27/31, 79%), currently treated vasospasm (20/31, 59%), suspicion of vasospasm (15/31, 44%), and the patient who cannot tolerate external ventricular derivation (EVD) clamping during mobilization (11/31, 32%).
Ninety-one percent (28/31) of the centres identified at least 1 complication that could be associated with standing upright. These mainly included decreased cerebral perfusion (24/31, 71%), dislodged external ventricular or lumbar derivations (23/31, 68%), and haemodynamic instability (22/31, 65%) (Fig. 2).
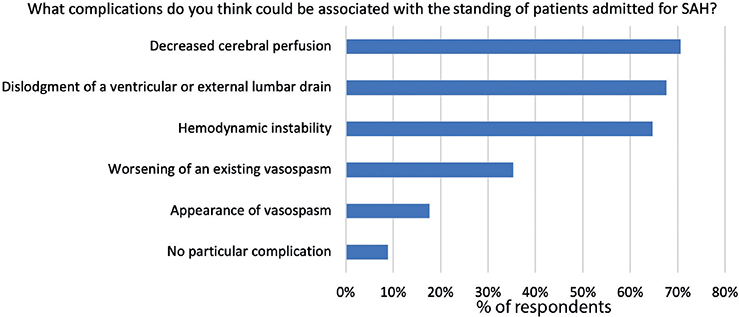
Fig. 2. Complications associated with the standing of patients with subarachnoid haemorrhage (SAH).
DISCUSSION
This study showed that early mobilization of patients with SAH was not standardized in French ICUs; 90% of services did not have an early mobilization protocol, and early mobilization is therefore largely heterogeneous. A recent survey by Hernandez et al. (17) found a similar result with 93% of respondents not having a mobility protocol for patients with SAH.
Patients with SAH, while brain injured, differ greatly from other types of strokes whether ischaemic or intracerebral haematoma. Stroke trials are therefore not transposable. This study set out new data about practices in this specific setting and exposed non-evidence-based barriers limiting patient mobilization. Similarly to the results of the current study, in the survey conducted by Hernandez et al. (17), physical therapists were more cautious and reduced the level of mobilization when patients had high-grade SAH or were intubated. While several observational studies assessing the safety of mobilization protocols did not report any mobilization-related EVD dislodgement (18), it remained a major concern for most respondents. The same concern was found in the European survey conducted by Hossain et al., in which the presence of EVD was associated with a restriction of mobilization (19). Regarding haemodynamic concerns, several studies have shown very few mobilization-related hypotensive events and no significant increase in intracranial pressure (18). The observational character of these studies may not provide sufficient evidence to reassure clinicians and may therefore contribute to the continuation of conservative practices. Conversely, few services have determined a maximum duration for chair installation. The AVERT study, which tested very early mobilization in stroke, showed that an increased duration of out-of-bed activities was detrimental, whereas an increased frequency was favourable (5).
In conclusion, the current study showed that mobilization of patients with SAH is heterogeneous among French neuro-ICUs, and that several barriers precluded the improvement of mobilization practices. Implementation and evaluation of EM protocols through interventional studies, as well as education and training of staff, is crucial to ensure proper mobilization of patients with SAH and to improve outcomes.
ACKNOWLEDGEMENTS
Informed consent was assumed if physiotherapists completed and submitted their completed survey online.
REFERENCES
- Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016; 388: 1377–1388. DOI: 10.1016/S0140-6736(16)31637-3
- Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009; 373: 1874–1882. DOI: 10.1016/S0140-6736(09)60658-9
- Patel BK, Wolfe KS, Patel SB, Dugan KC, Esbrook CL, Pawlik AJ, et al. Effect of early mobilisation on long-term cognitive impairment in critical illness in the USA: a randomised controlled trial. Lancet Respir Med 2023; 11: 563–572. DOI: 10.1016/S2213-2600(22)00489-1
- The TEAM Study Investigators and the ANZICS Clinical Trials Group. Early active mobilization during mechanical ventilation in the ICU. N Engl J Med 2022; 387: 1747–1758. DOI: 10.1056/NEJMoa2209083
- The AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet 2015; 386: 46–55. DOI: 10.1016/S0140-6736(15)60690-0
- Olkowski BF, Binning MJ, Sanfillippo G, Arcaro ML, Slotnick LE, Veznedaroglu E, et al. Early mobilization in aneurysmal subarachnoid hemorrhage accelerates recovery and reduces length of stay. J Acute Care Phys Ther 2015; 6: 47–55. DOI: 10.1097/JAT.0000000000000008
- Okamura M, Konishi M, Sagara A, Shimizu Y, Nakamura T. Impact of early mobilization on discharge disposition and functional status in patients with subarachnoid hemorrhage: A retrospective cohort study. Medicine (Baltimore) 2021; 100: e28171. DOI: 10.1097/MD.0000000000028171
- Milovanovic A, Grujicic D, Bogosavljevic V, Jokovic M, Mujovic N, Petronic Markovic I. Efficacy of early rehabilitation after surgical repair of acute aneurysmal subarachnoid hemorrhage: outcomes after verticalization on day 2–5 versus day 12 post-bleeding. Turk Neurosurg 2016; 27: 867–873. DOI: 10.5137/1019-5149.JTN.17711-16.1
- Karic T, Sorteberg A, Haug Nordenmark T, Becker F, Roe C. Early rehabilitation in patients with acute aneurysmal subarachnoid hemorrhage. Disabil Rehabil 2015; 37: 1446–1454. DOI: 10.3109/09638288.2014.966162
- Riordan MA, Kyle M, Dedeo C, Villwock MR, Bauer M, Vallano ML, et al. Mild exercise reduces cerebral vasospasm after aneurysm subarachnoid hemorrhage: a retrospective clinical study and correlation with laboratory investigation. In: Fandino J, Marbacher S, Fathi A-R, Muroi C, Keller E, editors. Neurovascular events after subarachnoid hemorrhage. Cham: Springer International Publishing; 2015, p. 55–61. DOI: 10.1007/978-3-319-04981-6_10
- Shimamura N, Matsuda N, Satou J, Nakano T, Ohkuma H. Early ambulation produces favorable outcome and non-demential state in aneurysmal subarachnoid hemorrhage patients older than 70 years of age. World Neurosurg 2014; 81: 330–334. DOI: 10.1016/j.wneu.2012.12.007
- Chou SH-Y. Subarachnoid hemorrhage. Continuum (Minneap Minn) 2021; 27: 1201–1245. DOI: 10.1212/CON.0000000000001052
- Hoh BL, Ko NU, Amin-Hanjani S, Hsiang-Yi Chou S, Cruz-Flores S, Dangayach NS, et al. 2023 Guideline for the management of patients with aneurysmal subarachnoid hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke 2023; 54: e314–e370. DOI: 10.1161/STR.0000000000000436
- Audibert G, Bousquet S, Charpentier C, Devaux Y, Mertes P-M. Hémorragie sous-arachnoïdienne: épidémiologie, prédisposition, présentation clinique. Annales Françaises d’Anesthésie et de Réanimation 2007; 26: 943–947. DOI: 10.1016/j.annfar.2007.09.006
- Foudhaili A, Barthélémy R, Collet M, De Roquetaillade C, Kerever S, Vitiello D, et al. Impact of early out-of-bed mobilization on functional outcome in patients with aneurysmal subarachnoid hemorrhage: a retrospective cohort study. World Neurosurg 2023: 175: e278–e287. DOI: 10.1016/j.wneu.2023.03.073
- Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med 2021; 36: 3179–3187. DOI: 10.1007/s11606-021-06737-1
- Hernandez, Sabrina, Thomas P, Udy A, Hodgson C. Early mobilisation of patients in the acute hospital setting following aneurysmal subarachnoid haemorrhage – a survey of current physiotherapy practice. N Z J Physiother 2019; 46: 113–132. DOI: 10.15619/NZJP/46.3.04
- Young B, Moyer M, Pino W, Kung D, Zager E, Kumar MA. Safety and feasibility of early mobilization in patients with subarachnoid hemorrhage and external ventricular drain. Neurocrit Care 2019; 31: 88–96. DOI: 10.1007/s12028-019-00670-2
- Hossain I, Younsi A, Castaño Leon AM, Lippa L, Tóth P Terpolilli N, et al. Huge variability in restrictions of mobilization for patients with aneurysmal subarachnoid hemorrhage – a European survey of practice. Brain Spine 2023; 3: 101731. DOI: 10.1016/j.bas.2023.101731