ORIGINAL REPORT
CHARACTERIZATION OF AN ITALIAN POPULATION WITH NEUROLOGICAL DISORDERS IN A REHABILITATION SETTING USING CLINFIT
Sara LIGUORI, MD, PhDs1*, Melissa SELB, MSc2,3, Antimo MORETTI, MD1, Marco PAOLETTA, MD1, Marco INVERNIZZI, MD, PhD4,5, Pietro FIORE, MD6, Giovanni IOLASCON, MD1, Francesca GIMIGLIANO, MD, PhD7 and The Italian Society of NeuroRehabilitation (SIRN) Residents Section Group
From the 1Department of Medical and Surgical Specialties and Dentistry, Luigi Vanvitelli University of Campania, Naples, Italy, 2Swiss Paraplegic Research, Nottwil, Switzerland, 3International Classification of Functioning, Disability and Health (ICF) Research Branch, Nottwil, Switzerland, 4Physical and Rehabilitative Medicine, Department of Health Sciences, University of Eastern Piedmont “A. Avogadro”, Novara, 5Dipartimento Attività Integrate Ricerca e Innovazione (DAIRI), Translational Medicine, Azienda Ospedaliera SS. Antonio e Biagio e Cesare Arrigo, Alessandria, 6Neurological Rehabilitation and Spinal Unit, Bari and 7Department of Mental and Physical Health and Preventive Medicine, Luigi Vanvitelli University of Campania, Naples, Italy
Objective: To examine the functioning profile of people with neurological disorders who access rehabilitation services through ClinFIT Generic-30.
Methods: The functioning profile of people with neurological disorders accessing rehabilitation services was examined using the ClinFIT Generic-30, and the results compared with existing core set (neurological health conditions acute and post-acute,stroke, Multiple Sclerosis, Traumatic Brain Injury,Spinal Cord Injury).
Results: Data for 364 people were analysed. The 10 most commonly impaired ICF categories included 3 for Body Functions (exercise tolerance functions (b455), mobility of joint functions (b710), and muscle power functions (b730)) and 7 for Activities and Participation (carrying out daily routine (d230), handling stress and other psychological demands (d240), changing basic body position (d410), maintaining a body position (d415), transferring oneself (d420), walking (d450), and moving around (d455)), while the ICF categories that were severely impaired (ICF qualifiers 3 and 4) in more than 30% of the study cohort were: muscle power functions (b730), carrying out daily routine (d230), walking (d450), moving around (d455), doing housework (d640), and assisting others (d660).
Discussion: The current study data suggests that ClinFIT Generic-30 appears to effectively identify impairments and/or restrictions, as perceived by individuals affected by selected health conditions.
Conclusion: ClinFIT Generic-30 is a tool that can be used to characterize functioning profile in people with different neurological disorders and to collect important information not addressed by the disease-specific core sets (neurological health conditions acute and post-acute,stroke, Multiple Sclerosis, Traumatic Brain Injury,Spinal Cord Injury).
LAY ABSTRACT
Neurological disorders are the leading cause of disability worldwide. ClinFIT is a tool that can be used by clinicians to assess functioning and disability in people with any health condition. It comprises categories that measure impairments in body functions (e.g. joint mobility), organs and other body structures, as well as the limitations/restrictions that people experience in performing everyday activities and participating in all areas of life (e.g. work), and the environmental factors (e.g. medication) which facilitate or pose a barrier to these experiences. Data for 364 people were analysed. The 10 most commonly impaired categories included 3 related to body functions and 7 to activities and participation. The categories severely impaired in more than 30% of the study participants were muscle power functions, carrying out daily routine, walking, moving around, doing housework and assisting others. In conclusion, ClinFIT Generic-30 is able to characterize the functioning profile in people with different neurological disorders.
Key words: functioning; International Classification of Functioning, Disability and Health; neurological disease; rehabilitation.
Citation: J Rehabil Med 2024; 56: jrm18262. DOI: https://doi.org/10.2340/jrm.v56.18262
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Submitted: Jul 18, 2023; Accepted: Nov 22, 2023; Published: Jan 18, 2024
Correspondence address: Sara Liguori, Department of Medical and Surgical Specialties and Dentistry, University of Campania “Luigi Vanvitelli”, Naples, IT-80100, Italy. E-mail: sara.liguori@unicampania.it
Competing interests and funding: The authors have no conflicts of interest to declare.
Neurological disorders can occur at all ages and represent the leading cause of disability and the second leading cause of death worldwide (1). According to data from the Global Burden of Disease 2017 Study, in Europe, neurological disorders represent the third cause of death and disability, accounting for approximately 1.1 million deaths and 21.0 million DALYs (disability-adjusted life-years) (2). Stroke is one of the major contributors, followed by dementia, and headache (2).
Considered the key health strategy of the 21st century, rehabilitation is an essential component of care of people with a neurological disorder. Physical and Rehabilitation Medicine (PRM) as the “medicine of functioning” aims to optimize the functioning of patients (3). As such, the World Health Organization’s (WHO’s) International Classification of Functioning, Disability and Health (ICF) is fundamental to PRM (4).
ICF is a comprehensive classification with more than 1400 categories. However, for its application in routine clinical practice, it is only necessary to use a short list of categories, either the ICF core sets for specific health conditions (5) or the ICF Generic-30 Set (formerly called rehabilitation set) that is useful for assessing functioning and disability of persons with any health condition along the continuum of care (6). Each condition-specific ICF core set has a brief version that is a smaller selection of categories from a larger comprehensive version. The International Society of PRM (ISPRM), in collaboration with National and Regional societies of PRM, has developed the ClinFIT, an ICF‑based clinical tool for the assessment of functioning characterized by simple, descriptions, adopting a friendly language for a more immediate and better understanding of the ICF categories (7–11). The ClinFIT can be tailored according to the needs of different rehabilitation services (along the continuum of care), patient populations (across age groups and health conditions), and countries (low‑, middle‑, and high‑income) (7).
To implement the use of the ICF in clinical practice and research among Italian residents in PRM, the Italian Society of PRM (SIMFER) promoted a project using ClinFIT based on the ICF Generic-30 Set (referred to as ClinFIT Generic-30 in this paper) to collect functioning data of people with any health condition who accessed outpatient rehabilitation services (12). Considering the complexity of neurological disorders and their high disability weight, the Italian Society of NeuroRehabilitation (SIRN) Residents’ section has proposed a similar project with a specific focus on people with neurological health conditions. The aim of this study was therefore to use ClinFIT Generic-30 to examine the functioning profile of people with neuro-logical disorders who access rehabilitation services.
MATERIAL AND METHODS
This cross-sectional study was designed and conducted by the 5 residents in PRM who had been elected as representatives of the SIRN Residents’ section instituted during the XVIII National Congress of SIRN held in Trieste, Italy, 5–7 April 2018, and working in 3 University Hospitals: Università della Campania “Luigi Vanvitelli”, Università di Foggia, and Università del Piemonte Orientale. The 5 trainees attended the final year of PRM specialties and they undertook a dedicated training to administer ClinFIT Generic-30, the training consisted of a 2-day theoretical-practical course on the basics of the ICF, to explain what ClinFIT is and how to apply it. Moreover, some of the trainees has participated in a previous study using ICF Generic-30 to assess people with any health condition who accessed outpatient rehabilitation services (12).
Adults (≥18 years old) with an acquired and/or degenerative neurological health condition who were referred to outpatient rehabilitation services or care units in Italy from November 2018 to November 2019 were consecutively included in the study. Exclusion criteria were inability to understand the study information and give informed consent.
All patients were invited by the PRM resident to participate in the study at admission to the outpatient services or care units.
Demographic (sex and age), clinical (diagnosis) and functioning data were collected during admission; information about ongoing rehabilitative treatment was not collected. To collect information about the functioning profile the Italian version of the ClinFIT Generic-30 (10) we performed once, when the patient was admitted to the outpatient rehabilitation services or care unit. This version has been previously validated and quality secured (10–12). To rate the severity of a problem in a specific aspect of functioning, the ClinFIT Generic-30 was applied using the ordinal-scaled scoring system provided in the ICF called “qualifiers”. Specifically, the generic qualifier was used for the body function categories (i.e. ICF categories that reflect the physiological and psychological functions of the body, such as energy and drive functions, sensation of pain and exercise tolerance functions) and the “performance” generic qualifier for the activity and participation categories, which considers the impact of environmental factors on what the person does or can do in his/her usual environment. The generic qualifiers are 0 for no problem, 1 for mild problem, 2 for moderate problem, 3 for severe problem, 4 for complete problem, 8 not specified, and 9 not applicable (4).
Data were analysed using descriptive statistics and presented as absolute numbers and percentages. The population was grouped according to the different health conditions. Severity was reported using the qualifiers, making a distinction whether the impairment/problem was mild/moderate (1–2) or severe/complete (3–4). A sub-analysis was performed for the sex distribution of qualifier 3–4, differentiating for the 7 identified health conditions. A comparison was made between the ClinFIT Generic-30 categories and the categories of the respective brief ICF core set for each of the 7 health condition, when available, in order to verify any differences between the functioning domains present in each tool. This study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (13).
The ethics committee of the Università della Campania “Luigi Vanvitelli” (Committee’s reference number 0017390/2020) approved the study protocol, and all participants read and signed an informed consent according to the Declaration of Helsinki. Data collection lasted from November 2018 to November 2019.
RESULTS
Data from 364 consecutively enrolled persons with a neurological health condition were collected and analysed. The mean age was 59.7 ± 17.8 years. The majority of the population was male (60.4%). Half of the participants came from the north of Italy (181) and the other half from the south of Italy (73 from Università di Foggia and 110 from Università della Campania “Luigi Vanvitelli”). None of the trainees reported any problems using ClinFIT. The study population was affected by 7 neurological health conditions: 181 stroke (ischaemic and haemorrhagic) (49.73%), 59 Parkinson’s disease (PD) (16.21%), 29 multiple sclerosis (MS) (7.97%), 16 traumatic brain injury (TBI) (4.40%), 13 spinal cord injury (SCI) (3.57%), 57 neuromuscular disorders (NMDs) (15.66%), and 9 patients underwent neurosurgical procedures for several reasons (NS) (2.47%). Fig. 1 shows the frequency of the neurological disorders included in this study cohort.
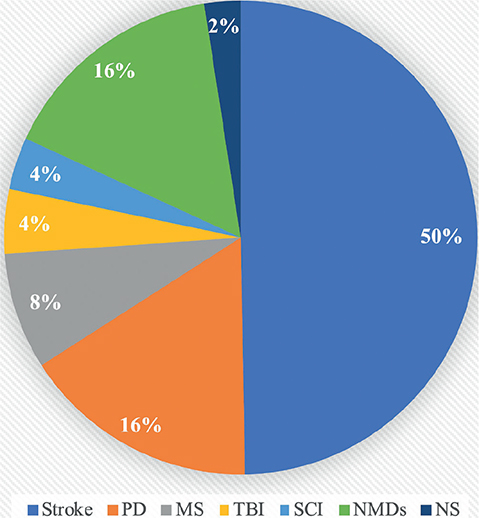
Fig. 1. Frequency of the neurological disorders included in this study cohort.
Fig. 2 shows the global functioning profile of the study cohort, expressed as absolute numbers and percentages of patients who reported the extent of a problem in functioning represented by a specific ICF category according to the qualifier rating. The 10 most commonly impacted ICF categories were 3 Body Function categories (exercise tolerance functions (b455), mobility of joint functions (b710), and muscle power functions (b730)), and 7 Activities and Participation categories (carrying out daily routine (d230), handling stress and other psychological demands (d240), changing basic body position (d410), maintaining a body position (d415), transferring oneself (d420), walking (d450), and moving around (d455)). More than 30% of the study cohort was severely impaired (ICF qualifiers 3 and 4) in the following ICF categories: muscle power functions (b730), carrying out daily routine (d230), walking (d450), moving around (d455), doing housework (d640), and assisting others (d660).
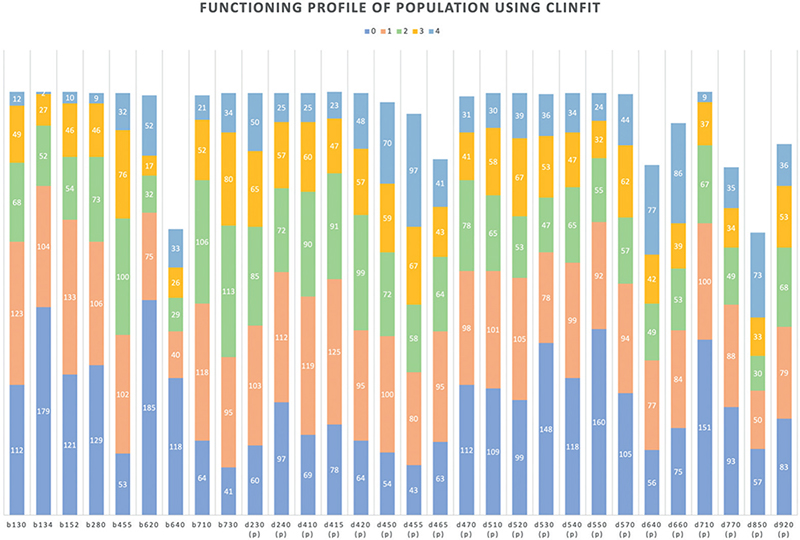
Fig. 2. Functioning profile of the population using the ClinFIT. Horizontal axis reports the ClinFIT categories; the vertical axis refers to the number of patients included.
The least compromised ICF categories (with a generic qualifier of 0 reported by more than 40% of the study population) were sleep functions (b134), urination functions (b620), toileting (d530), eating (d550) and basic interpersonal interactions (d710).
Table I reports the cumulative frequencies of the presence of any impairment/problem (qualifiers 1–4) or of a severe/complete impairment/problem (qualifier 3–4) for the 7 identified health conditions. Regarding the sex distribution of the qualifiers 3–4, a greater number of males reported a severe/complete impairment/problem for the following categories exercise tolerance functions (b455), sexual functions (b640), muscle power functions (b730), moving around (d455), washing oneself (d510), caring for body parts (d520), and preparation of meals (d630), with a discrepancy of >10 individuals between the 2 groups. For the energy and drive functions (b130) category, more females reported a severe/complete problem (36 females vs 25 males) (Fig. 3a). Similarly, in the stroke group, (Fig. 3b) a greater number of males reported a severe/complete impairment/problem for all the categories except sleep (b134), emotional functions (b152), pain (b280) and basic interpersonal interactions (d710). Fig. 3 shows the sex distribution of the qualifiers 3–4 for the overall cohort and each disease.
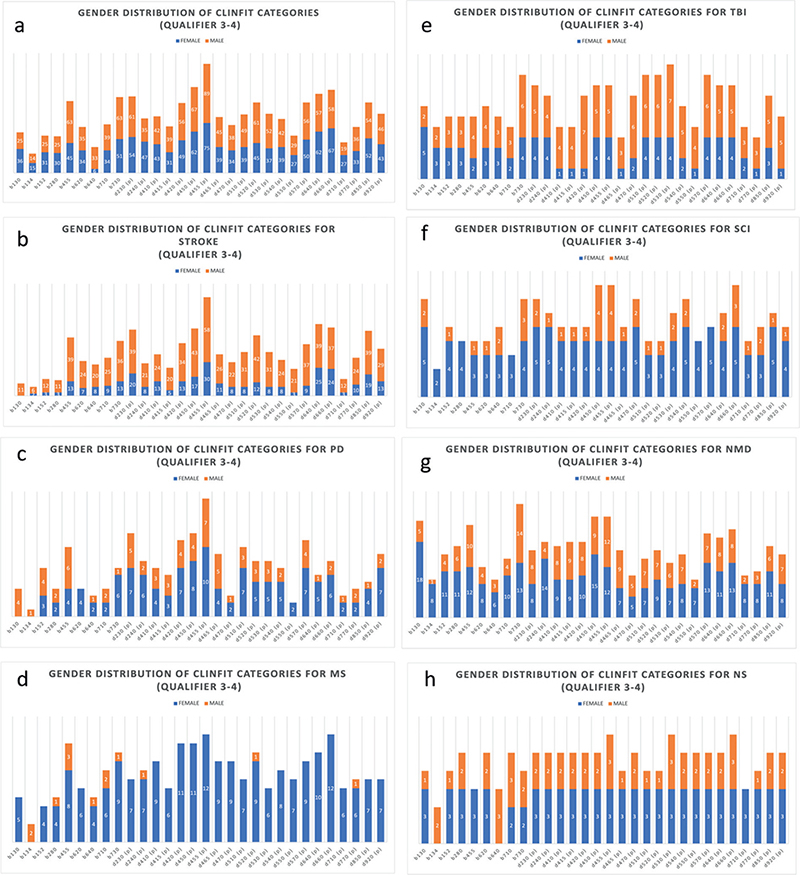
Fig. 3. Sex distribution of the ClinFIT qualifiers 3–4 for the whole population and for the 7 identified health conditions. Data were reported as absolute values; (a) total number N = 364; female N = 144, male N = 220; (b) total number N = 181; female N = 76, male N = 105; (c) total number N = 59, female N = 18, male N = 41; (d) total number N = 29; female N = 19, male N = 10; (e) total number N = 16 female, N = 5 male N = 11; (f) total number N = 13 female, N = 5 male N = 8; (g) total number N = 57 female, N = 18 male N = 39; (h) total number N = 9 female, N = 3 male N = 6. PD: Parkinson’s disease; MS: multiple sclerosis; TBI: traumatic brain injury; SCI: spinal cord injury; NMDs: neuromuscular disorders; NS: neurosurgical procedures.
Table II reports the ICF categories comparison between ClinFIT Generic-30 and ICF brief core set of stroke, multiple sclerosis (MS), traumatic brain injury (TBI), and spinal cord injury (SCI) (available as early post-acute and chronic phases).
DISCUSSION
This study aims to describe the functioning profile of people affected by neurological health conditions, using the ClinFIT Generic-30. In a SIMFER-supported project examining the functioning profile of people with any health condition who accessed outpatient rehabilitation services using the same tool (12), the data collected on the population with a neurological health condition was limited to only 41 people with PD (12).
Comparing the ClinFIT Generic-30 with the brief ICF core sets for neurological health conditions (stroke, MS, TBI, SCI early post-acute and chronic, and neurological health conditions acute and post-acute), 24 out of 30 ClinFIT Generic-30 categories are included in at least 1 of the disease-specific brief core sets and all 30 categories are included in at least 1 of the comprehensive versions of these same core sets (14–20). When specifically comparing the ClinFITGeneric-30 with the 18-category brief ICF core set for stroke, it was found that 6 ClinFIT Generic-30 categories are in the brief version (20). The only Generic-30 category that is not covered by the 130-category comprehensive version is assisting others (d660) which in the current study data collection was reported as a problem by 80.66% of the population and as a severe/complete problem by 45.30%. It is noteworthy that the following categories reported as problematic by more than 75% of the stroke population are not included in the brief version of the ICF core sets for stroke: emotional function (b152), exercise tolerance functions (b455), mobility of joints functions (b710), carrying out daily routine (d230), handling stress and other psychological demands (d240), changing basic body position (d410), maintaining a body position (d415), transferring oneself (d420), moving around (d455), using transportation (d470), caring for body parts (d520), looking after one’s health (d570), assisting others (d660), and basic interpersonal interactions (d710). In particular, carrying out daily routine (d230), moving around (d455), caring for body parts (d520), looking after one’s health (d570), doing housework (d640), assisting others (d660) and remunerative employment (d850) were reported as severe/complete problems by more than 40% of the current study sample of stroke patients. In 2010, Algurén et al. published a longitudinal cohort study analysing the functioning profile of 99 Swedish stroke survivors with the comprehensive ICF core set for stroke (21). In this study two-thirds of the study population reported an impairment/problem in exercise tolerance functions (b455), muscle power functions (b730), energy and drive functions (b130), and walking (d450). The same categories were also reported as an impairment/problem by more than 70% of the patients in our study (21). This suggests that the ClinFIT Generic-30 might be sufficient in consistently detecting the major impairments/problems in the stroke population.
This study also compared the ClinFIT Generic-30 categories with the ICF core set for MS. It was found that 8 of the ClinFIT Generic-30 categories are included in the19-category brief version (16). Twenty-seven out of the 29 people with MS included in our cohort reported an impairment in exercise tolerance functions (b455) and 10 of them reported the impairment to be severe/complete. This category is included only in the comprehensive version of the MS core set. One of the most common impairments reported by people with MS is fatigue. Fatigue has also been found to be one of the main causes of impaired quality of life in this population (22). There are 2 ICF categories that can describe the symptom of fatigue: energy and drive functions (b130), which is related to the mental aspects of fatigue and exercise tolerance functions (b455), which is related to the physical aspects of this symptom. In our data collection, 93.10% of patients with MS reported an impairment in exercise tolerance functions (b455), a much higher percentage than those complaining of an impairment in energy and drive functions (b130) (55.17%). ClinFIT Generic-30, compared with the brief specific ICF core set seems to address both components of fatigue in the MS population better.
Regarding the TBI core sets, 12 categories of the ClinFIT Generic-30 are part of the 23-category brief version (17). The categories that were reported as a severe/complete impairment/problem by more than half of our cohort and missing in the brief ICF core set for TBI were: muscle power functions (b730), looking after one’s health (d570), and assisting others (d660). All 16 people with TBI in our cohort reported the category intimate relationship (d770) as a problem, but this is not included in the brief core set (17.). It is important to note that post-TBI, patients and their intimate partners often experience drastic changes in their relationship. Several barriers to intimacy include injury-related changes, sexual difficulties and communication issues, thus making “intimate relationship” a noteworthy field of functioning to be addressed in this population, covered by ClinFIT Generic-30 (23).
Regarding the comparison of the ClinFIT Generic-30 with the 4 ICF core sets for SCI, 2 for the early post-acute phase (comprehensive and brief) and 2 for the chronic phase (18, 19), it was found that 11 categories are included in the early post-acute version (18), and 16 categories of ClinFIT Generic-30 are included in the brief version of the chronic phase core sets (19). There were 2 categories that were considered as impaired in all the 13 patients with SCI in the current sample: exercise tolerance functions (b455) and changing basic body position (d410), while moving around (d455) and assisting others (d660), were reported as a severe/complete problem by the majority of our cohort. In particular, assisting others (d660) is missing in both the early post-acute and chronic phase versions. Considering the availability of equipment that promotes individual independence or home changes to improve indoor accessibility, it is possible that a person with SCI can assist others and not only be assisted. This highlights how ClinFIT Generic-30 is able to address the functioning of neurological patient as a whole, including facets that can change over time or with environmental factors.
When looking at the functioning data of people with PD, it was found that only 3 ICF categories of the ClinFIT Generic-30 were reported as an impairment in more than 75% of the study population. These are: exercise tolerance functions (b455), mobility of joints functions (b710), and muscle power functions (b730). There is no validated core set for people with Parkinson’s disease (PD). However, Raggi et al., published a study examining the functioning profile of 96 people with PD using the ICF checklist and reported among the most relevant categories (perceived as an impairment by at least 50% of their cohort) 8 in the Body Function domain and 18 in the domain of Activities and Participation (24). Five of these 8 Body Function categories are also covered by ClinFIT Generic-30. However, only 1 of them, muscle power functions (b730), was reported as an impairment by more than half of the study cohort, while all 5 Body Functioning categories were reported as an impairment by more than half of the people with PD in the previous study conducted by Gimigliano et al. (12). Of the 18 categories in the Activity and Participation domain identified as most relevant by Raggi et al. (9), are also covered by ClinFIT Generic-30, of which 4 are reported as a problem by more than half of the current study cohort and 5 by the PD population in the study by Gimigliano et al. (12, 24). This suggests that ClinFIT Generic-30 could be used for a as generic first-line assessment to describe functioning also in this population.
With regard to NMDs, Bos et al. (25), proposed an ICF core set for people with NMDs based the results of their study to validate the ICF core set for chronic neurological conditions specifically for NMDs. ClinFIT Generic-30 contains 23 categories of this core set (7 Body Functions and 16 Activity and Participation categories). Among the 23 categories, the following were reported as impaired in over 75% of the current study cohort: energy and drive functions (b130), exercise tolerance functions (b455), and muscle power functions (b730). The ClinFIT Generic-30 category energy and drive functions (b130) is represented in Bos et al.’s core set with the more detailed category energy level (b1300). It is key to note that NMDs include different categories of disorders with a heterogeneous clinical scenario; in lack of a validated core set, the capability to catch functioning issues through ClinFIT could be extremely useful in these chronic patients. Finally, in our sub-analysis, a significant sex disparity was observed with regard to the qualifiers 3–4, i.e. significantly more male participants reported severe/complete impairments or problems than females, as depicted in Fig. 3. This may be explained by the larger sample size of males. The graphs illustrating the total and subpopulations show that the male sample size was consistently twice as large as the female sample size in almost all cases. However, when examining the MS cohort in graph d, comprising 19 females and 10 males, a distinct trend was noticed. The female group overwhelmingly exhibited qualifiers 3–4, except for b134, in which only 2 males reported severe or complete impairment/problems. These findings, although intriguing, do not allow us to draw any significant conclusions. In future studies, we intend to ensure a more balanced and consistent sample size to enable a more productive comparison.
The current study data suggests that the ClinFIT Generic-30 might be useful for generating the functioning profile of a person with diverse neurological health condition.
Globally, ClinFIT and its categories appear to effectively identify impairments and/or restrictions, as perceived by individuals affected by selected health conditions. These findings hold promise for the practical application of this tool in supporting clinical decision-making in rehabilitation settings.
In terms of user-friendliness of ClinFIT, the simple descriptions of the ICF categories provided by ClinFIT Generic-30 seem to make this tool easy to use, as shown in the aforementioned study on the use of ClinFIT Generic-30 by residents in PRM (12). Other than for clinical decision-making, there are other applications of the ClinFIT Generic-30. For example, it provides the possibility of making comparisons between the functioning of populations with different neurological disorders. Moreover, and, at the same time, this tool could be used to collect data for patients with neurological disabilities, for health service planning and management, resource allocation, development of policies and programmes, or for advocacy purposes. And since the use of the ICF in the rehabilitation planning of persons with neurological health conditions in terms of facilitating interdisciplinary teamwork has shown promise, despite not yet being fully integrated into daily clinical practice (26), we expect the ClinFIT would likewise be an asset in strengthening interdisciplinary teamwork. The functional descriptions collected by this tool allow for a consistent and personalized evaluation of medical needs as well as of general health and social participation of people with disabilities, facilitating the delivery of a holistic and tailored set of services and assistance.
Our data collection shows that, to cover the whole spectrum of functioning of a person with a specific neurological disorder, the use of the dedicated ICF core sets seems the most proper, context-cutting, and exhaustive option. Otherwise, if a specific core set is lacking, the ClinFIT Generic-30 could be an alternative tool to cover health condition-specific functioning (6).
Limitations
The main limitation of the current study is that it did not collect information about the course of the disease. Therefore, it is unclear how this might have impacted the functioning profile of our patient population. The cross-sectional design of the study could be interpreted as a limit regarding the lack of data about the functioning level of our cohort post-rehabilitation. The current ordinal scoring of ClinFIT could be considered a limitation, as it limits our ability to monitor changes in a patient’s functioning over time. With an ordinal scale, it is possible to indicate that a patient’s functioning has changed (improved or declined), but not the extent of the change. This is, however, possible with an interval scale. An interval scale would also enable us to compare the functioning of different patients. As shown by some ClinFIT studies (10, 11), it is possible to transform the ordinal-scaled scores to an interval-scaled scores. Lastly, failing to collect surgical history from the participants may be a study limitation, as having information about surgeries that participants underwent, especially neurosurgeries, may have enhanced our understanding of the functioning of the current study cohort. Finally, the lack of a specific core set of the post-neurosurgery ICF did not allow a comparison with the most impacted categories that emerged from the ClinFIT Generic-30 in this population.
Conclusion
The ClinFIT Generic-30 set seems to be a useful tool for capturing the functioning profile of people with different neurological conditions. The results of the current study and the corresponding functioning profile of an Italian population with neurological disorders generated by applying ClinFIT Generic-30 should help support the decision-making process in neurorehabilitation along the continuum of care, from the assessment and goal-setting to the selection of appropriate outcome measures and interventions.
ACKNOWLEDGEMENTS
The ethics committee of the Università della Campania “Luigi Vanvitelli” (Committee reference number 0017390/2020) approved the study protocol, and all participants read and signed an informed consent according to the Declaration of Helsinki.
This paper was presented as oral presentation during the XX congress of the Italian Society of NeuroRehabilitation.
The data associated with this paper are not publicly available, but are available from the corresponding author on reasonable request.
REFERENCES
- Feigin VL, Vos T, Nichols E, Owolabi MO, Carroll WM, Dichgans M, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol 2020; 19: 255–265.
- Deuschl G, Beghi E, Fazekas F, Varga T, Christoforidi KA, Sipido E, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020; 5: e551–e567. DOI: 10.1016/S2468-2667(20)30190-0
- Stucki G, Bickenbach J, Gutenbrunner C, Melvin J. Rehabilitation: the health strategy of the 21st century. J Rehabil Med 2018; 50: 309–316. DOI: 10.2340/16501977-2200
- WHO. International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization, 2001. [Accessed July 2023] Available from: http://www.who.int/classifications/icf/en/
- Selb M, Escorpizo R, Kostanjsek N, Stucki G, Üstün B, Cieza A. A guide on how to develop an International Classification of Functioning, Disability and Health Core Set. Eur J Phys Rehabil Med 2015; 51: 105–117.
- Prodinger B, Cieza A, Oberhauser C, Bickenbach J, Üstün TB, Chatterji S, et al. Toward the International Classification of Functioning, Disability and Health (ICF) rehabilitation set: a minimal generic set of domains for rehabilitation as a health strategy. Arch Phys Med Rehabil 2016; 97: 875–884. DOI: 10.1016/j.apmr.2015.12.030
- Frontera W, Gimigliano F, Melvin J, Li J, Li L, Lains J, et al. ClinFIT: ISPRM’s Universal Functioning Information Tool based on the WHO’s ICF. J Int Soc Phys Rehabil Med 2019; 2: 19–21.
- Prodinger B, Reinhardt JD, Selb M, Stucki G, Yan T, Zhang X, et al. Towards system-wide implementation of the International Classification of Functioning, Disability and Health (ICF) in routine practice: developing simple, intuitive descriptions of ICF categories in the ICF Generic and Rehabilitation Set. J Rehabil Med 2016; 48: 508–514. DOI: 10.2340/16501977-2066
- Selb M, Gimigliano F, Prodinger B, Stucki G, Pestelli G, Iocco M, et al. Toward an International Classification of Functioning, Disability and Health clinical data collection tool: the Italian experience of developing simple, intuitive descriptions of the Rehabilitation Set categories. Eur J Phys Rehabil Med 2017; 53: 290–298. DOI: 10.23736/S1973-9087.16.04250-7
- Mukaino M, Prodinger B, Yamada S, Senju Y, Izumi SI, Sonoda S, et al. Supporting the clinical use of the ICF in Japan – development of the Japanese version of the simple, intuitive descriptions for the ICF Generic-30 set, its operationalization through a rating reference guide, and interrater reliability study. BMC Health Serv Res 2020; 20: 66. DOI: 10.1186/s12913-020-4911-6
- Senju Y, Mukaino M, Prodinger B, Selb M, Okouchi Y, Mizutani K, et al. Development of a clinical tool for rating the body function categories of the ICF generic-30/rehabilitation set in Japanese rehabilitation practice and examination of its interrater reliability. BMC Med Res Methodol 2021; 21: 121.
- Gimigliano F, de Sire A, Gastaldo M, Maghini I, Paoletta M, Pasquini A, et al. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur J Phys Rehabil Med 2019; 55: 258–264. DOI: 10.23736/S1973-9087.18.05324-8
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344–349. doi: 10.1016/j.jclinepi.2007.11.008. PMID: 18313558.
- Ewert T, Grill E, Bartholomeyczik S, Finger M, Mokrusch T, Kostanjsek N, et al. ICF Core Set for patients with neurological conditions in the acute hospital. Disabil Rehabil 2005; 27: 367–373. DOI: 10.1080/09638280400014014
- Stier-Jarmer M, Grill E, Ewert T, Bartholomeyczik S, Finger M, Mokrusch T, et al. ICF Core Set for patients with neurological conditions in early post-acute rehabilitation facilities. Disabil Rehabil 2005; 27: 389–395. DOI: 10.1080/09638280400014022
- Coenen M, Cieza A, Freeman J, Khan F, Miller D, Weise A, et al. The development of ICF Core Sets for multiple sclerosis: results of the International Consensus Conference. J Neurol 2011; 258: 1477–1488. DOI: 10.1007/s00415-011-5963-7
- Laxe S, Zasler N, Selb M, Tate R, Tormos JM, Bernabeu M. Development of the International Classification of Functioning, Disability and Health core sets for traumatic brain injury: an International consensus process. Brain Inj 2013; 27: 379–387. DOI: 10.3109/02699052.2012.750757
- Kirchberger I, Cieza A, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the early post-acute context. Spinal Cord 2010; 48: 297–304. DOI: 10.1038/sc.2009.128
- Cieza A, Kirchberger I, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the long-term context. Spinal Cord 2010; 48: 305–312. DOI: 10.1038/sc.2009.183
- Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, Omar Z, et al. ICF Core Sets for stroke. J Rehabil Med 2004; Suppl 44: 135–141. DOI: 10.1080/16501960410016776
- Algurén B, Lundgren-Nilsson A, Sunnerhagen KS. Functioning of stroke survivors – a validation of the ICF core set for stroke in Sweden. Disabil Rehabil 2010; 32: 551–559. DOI: 10.3109/09638280903186335
- Braley TJ, Chervin RD. Fatigue in multiple sclerosis: mechanisms, evaluation, and treatment. Sleep 2010; 33: 1061–1067. DOI: 10.1093/sleep/33.8.1061
- Gill CJ, Sander AM, Robins N, Mazzei DK, Struchen MA. Exploring experiences of intimacy from the viewpoint of individuals with traumatic brain injury and their partners. J Head Trauma Rehabil 2011; 26: 56–68. DOI: 10.1097/HTR.0b013e3182048ee9
- Raggi A, Leonardi M, Ajovalasit D, Carella F, Soliveri P, Albanese A, et al. Disability and profiles of functioning of patients with Parkinson’s disease described with ICF classification. Int J Rehabil Res 2011; 34: 141–50. DOI: 10.1097/MRR.0b013e328344ae09
- Bos I, Stallinga HA, Middel B, Kuks JB, Wynia K. Validation of the ICF core set for neuromuscular diseases. Eur J Phys Rehabil Med 2013; 49: 179–187.
- Lexell J, Brogårdh C. The use of ICF in the neurorehabilitation process. NeuroRehabilitation 2015; 36: 5–9. DOI: 10.3233/NRE-141184