REVIEW
MAPPING THE COSTS AND SOCIOECONOMIC CHARACTERISTICS INVOLVED IN TRAUMATIC BRAIN INJURIES: A SCOPING REVIEW
Fanny CROZES, RN, PhDc1–3, Cyrille DELPIERRE, DR, PhD2 and Nadège COSTA, DR, PhD1,2
From the 1Health Economic Unit, University Hospital Center of Toulouse, Toulouse, 2EQUITY Research Team, Center for Epidemiology & Research in POPulation Health (CERPOP), UMR 1295, University Toulouse III Paul Sabatier, Toulouse, and 3Institute of Nursing Training, Toulouse University Hospital, Toulouse, France
Objective: To identify the articles in the existing literature that analyse healthcare costs according to the socioeconomic position (pre- or post-injury) for traumatic brain injury survivors. Secondary aims were to describe the types of costs and socioeconomic characteristics and to determine whether socioeconomic characteristics affect the risk of traumatic brain injury or whether the consequences of trauma alter living conditions post-injury.
Methods: This scoping review followed the methods proposed by Arksey and O’Malley. The literature search was performed in 5 databases.
Results: Twenty-two articles were included, published between 1988 and 2023. Only 2 articles (9%) followed the guidelines for economic evaluation of healthcare programmes and 2 articles (9%) evaluated socioeconomic position “completely” with 3 main individual measures of socioeconomic characteristics (i.e., education, income, and occupation). The relationship between costs and socioeconomic characteristics could vary in 2 ways in traumatic brain injury: socioeconomic disadvantage was mostly associated with higher healthcare costs, and the cost of healthcare reduced the survivors’ living conditions.
Conclusion: This work highlights the need for a detailed and methodologically sound assessment of the relationship between socioeconomic characteristics and the costs associated with trauma. Modelling the care pathways of traumatic brain injury would make it possible to identify populations at risk of poor recovery or deterioration following a TBI, and to develop specific care pathways. The aim is to build more appropriate, effective, and equitable care programmes.
LAY ABSTRACT
Victims of traumatic brain injuries often need care or help at the time of the trauma but also several months or years after the trauma. Here we are interested in the economic burden of trauma. We know that a disadvantaged person (low income, low level of education for example) is more likely to have a trauma and more complications. However, we do not know if deprivation changes the costs and trajectories of care and if delivered care is effective in the same way for everyone. This scoping review found that few studies measure costs according to people’s socioeconomic position. Available studies showed that the costs seem higher for a disadvantaged person, but also that the living conditions would be lower after the trauma (i.e., reduced social role or level of income or type of employment). There is therefore a need to carry out well-conducted research to correctly measure the costs according to these characteristics and to offer care adapted to individuals.
Key words: health economics; nurse; scoping; socioeconomic characteristics; TBI.
Citation: J Rehabil Med 2024; 56: jrm18311. DOI: https://doi.org/10.2340/jrm.v56.18311.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
Submitted: Sept 5, 2023; Accepted after revision: Jun 26, 2024; Published: Aug 5, 2024.
Correspondence address: Fanny Crozes, General Care Coordination, University Hospital Center of Toulouse, 2, rue Viguerie, FR-31059 Toulouse Cedex 9, France. E-mail: crozes.f@chu-toulouse.fr
Competing interests and funding: The authors have no conflicts of interest to declare.
The 2016 Global Burden of Disease Study (1) suggests that the overall incidence rate of traumatic brain injuries (TBI) has been estimated at 369 cases per 100,000 people per year, which represents approximately 27 million people affected. Other studies estimate the global incidence of TBI worldwide at between 73 and 939 cases per 100,000 people each year (2). This wide range of incidence estimation is partly due to income levels and prevention policies in the various countries, as well as to different data collection methodology (3, 4). TBI is a major cause of death, with 31% occurring during the initial hospital phase (5). This mortality persists with a rate of 27% 1 year after the trauma (6). Sequelae also lead to a 64% persistence of moderate disability at 1 year, difficulties in returning to work, and an altered quality of life (7), despite progress in rehabilitation (8).
Regarding the determinants of TBI, socioeconomic characteristics (in pre-injury or post-injury) have been shown to be associated with trauma or its consequences. The level of income, the level of education, or even isolation are linked to the occurrence of accidental acute events, such as falls and TBI (9–11). Disability related to TBI seems to be greater in patients who live in rural areas, which may be explained by difficult access to rehabilitation care (12). The literature highlights that TBI affects men and people under the age of 40 most commonly and severely; additionally, those with a traumatic head injury and a lower education level experience poorer health than those with a higher level of education (9, 13, 14).
TBI, and its severity, has significant medical and social consequences, and also constitutes an economic burden to the whole of society. Leibson et al. measured this extra cost to society up to 6 years after the injury by comparing people with brain injuries with a control population (15). The average extra cost of a TBI was US$22,000 during the acute phase and the extra cost persisted up to 6 years after the injury. The overall cost for all brain conditions is comparable to the sum of the costs associated with cardiovascular disease, cancer, and diabetes combined (16).
The consideration of costs according to social inequalities in health is essential, to measure their extent and also to estimate the cost burden on health systems attributable to social inequalities in order to rethink the societal model and deliver equitable care (17). Moreover, the view of health professionals is more in favour of equity or efficiency, depending on the country (18, 19). Decision-making of policy-makers needs to answer these questions concerning the optimal allocation of limited resources (20). Recent work has evaluated the relationship between the cost of care in the community or emergency department care, and social inequalities in health, particularly in European countries where the cost of care is a collective responsibility (21–24). Two main hypotheses can be made from the literature, i.e., (i) that social disadvantage accentuates comorbidities and makes care paths more complex and costlier, and (ii) that most disadvantaged people are at a greater risk of poor recovery and are therefore more likely to require more expensive care. But the literature considering both costs and social determinants is sparse, and so we still do not know whether geographical and socioeconomic characteristics modify the efficiency of the healthcare system. The questions of efficiency and equity therefore remain unanswered. However, the consideration of costs according to social inequalities in healthcare is essential, to measure their extent and also to estimate the cost burden on healthcare systems attributable to social inequalities in order to rethink the societal model and deliver equitable care (17).
Thus, the goal of this scoping review is to identify articles in the literature that analyse the healthcare costs for TBI survivors according to socioeconomic position, and summarize methods and results.
METHODS
According to Arksey and O’Malley (25), Anderson et al. (26), and Levac et al. (27), a scoping review can have four main purposes: (i) to examine the extent, range, and nature of -research activity; (ii) to determine the value of undertaking a full systematic review; (iii) to summarize and disseminate research findings; and (iv) to identify research gaps in the existing literature. Scoping reviews follow a rigorous methodology and allow an initial assessment of what has been done on the basis of heterogeneous data that do not allow a precise question to be answered like the systematic review. This work follows the specific PRISMA recommendations for scoping reviews (PRISMA-ScR).
Stage 1: Identification of the research question
Our research question was to identify the articles in the existing literature that analyse healthcare costs according to the socioeconomic position (pre-injury or post-injury) for TBI survivors. Then, 2 secondary objectives were pursued: (i) to describe the types of costs and socioeconomic characteristics present in the literature, and (ii) to determine whether socioeconomic characteristics affect the risk of TBI or whether the consequences of TBI alter the living conditions post-TBI.
Stage 2: Identifying relevant studies
In collaboration with a research librarian, we targeted different relevant databases and developed a search strategy using free-text terms for databases without thesauri and medical subject headings (MeSH) for databases with thesauri. Databases were selected based on the subject of this research. The literature search was performed in 5 different electronic databases to gather relevant literature: Medline, EMBase, Cochrane, International HTA database, and Web of Science. Note that the databases EMBase and International HTA database did not retrieve any new references.
All publications dated up to January 4, 2023 were included, with no limitations regarding the publication dates. The search terms are listed in Table SI. The type of publication was not filtered as recommended by O’Brien et al. (28). To be eligible for inclusion in this scoping review, articles were required to analyse healthcare costs according to the socioeconomic position of TBI survivors. Articles that assessed costs but not socioeconomic characteristics were excluded. Articles that assessed socioeconomic characteristics but not costs were excluded. Articles on injuries not specified as a head injury were excluded, as were those written in languages other than English or French. Lastly, books were excluded.
Stage 3: Selection of studies
The first researcher made an initial selection from the results obtained in the different databases. A first screening was done on the basis of the titles, then a second on the basis of the abstracts of the selected articles, to check that the articles used data related to costs and socioeconomic position. The full texts of the selected articles were then reviewed by 2 independent researchers. The exclusion of each article was based on a consensus of the 2 researchers. For the selected articles, the quality assessment (QualSyst tool (29)) of the articles was also done in a standardized way between the 2 researchers to reach consensus.
Stage 4: Charting data with critical appraisal
The data were extracted using a standardized form for each relevant article: first author, year of publication, study location, study design, patients’ characteristics, study sample, aims of the study, costs measures, socioeconomic characteristics measures, and the quality of the study. Socioeconomic characteristics and costs were described as presented in the articles and details of these variables are also specified in Table SII.
In order to deal with the heterogeneity of the articles and to propose elements of comparison, the economic variables were described and homogenized according to guidelines (30, 31). Direct costs are the resources used in the management of the injury or its adverse effects, including direct medical costs, directly related to the injury, as well as direct non-medical costs, related to the consequences of the management of the injury. Indirect costs are those costs that are indirectly related to the injury and have an impact on productivity. The intangible costs concern the consequences of the injury in terms of reduced well-being for the patient and family. If the perspective assumed is that of the payer, only direct costs are included. A patient perspective considers only costs that are relevant to patients, such as out-of-pocket or intangible costs. The perspective of the hospital considers costs attributable to institutions, such as equipment costs. The societal perspective includes all health effects and costs, including production losses due to illness. This is the most comprehensive perspective.
In the literature, 3 main individual measures are found to assess socioeconomic position, including income level, occupation or socio-professional category, and education level (32–35). These data are rarely collected routinely and are absent from healthcare databases. Therefore, an approximation of these individual data can be made on the basis of ecological indicators. Socioeconomic characteristics were identified and specified for each article. These characteristics have been collected and labelled for each article to enable comparison. Then, the type of measure was specified, such as individual characteristics and ecological indices. Individuals’ characteristics included education level, socio-professional category, income level, poverty rate, marital or living situation, race, or geographic region. The ecological indices use residential area variables to obtain an ecological index, such as household income by zip code or more specific indices related to deprivation level. Lastly, the assessment of socioeconomic individual characteristics was categorized as “partial” or “complete” based on the evaluation of 3 dimensions: education level, income, and socio-professional category. Also, an approximation of socioeconomic position can be made on the basis of ecological deprivation indices (36). The evaluation of ecological indicators was identified for each article (yes/no).
In accordance with guidelines for scoping reviews, the quality assessment of evidence can be performed where it assists with achieving the aim of the scoping review (28, 37). A data quality assessment method was then used, based on the critical appraisal tool QualSyst from Kmet et al. (29), which allows quantitative and qualitative articles to be systematically evaluated and averages of evaluation to be obtained, which then allow the quality of the sources to be subdivided into 4 categories: strong (score > 0.8), good (score between 0.79 and 0.6), adequate (score between 0.59 and 0.5), or poor (score < 0.5).
Stage 5: Collation, synthesis, and reporting results
The analysis of the meaning of the articles made it possible to position socioeconomic characteristics and costs as related to TBI or consequences of TBI. The articles acknowledge the temporality of events. A classification according to the temporality of the socioeconomic characteristics and costs in relation to the TBI has thus been done. It is important to specify that this is not a causal inference process but rather a description of the temporality of events based on literature data and their classification as pre-existing causal relationships or outcomes (see more about incorrect causal interpretation from Haber et al. (38)).
RESULTS
Our search produced 416 records. After the removal of duplicated records, 398 records were screened. A first screening on titles resulted in 180 records, with a second screening on abstracts leaving a total of 32 articles for assessment. Ten more articles were then excluded. Ultimately, 22 articles were included in this scoping review. A final update was made in January 2023 (a flowchart of the selection process according to PRISMA-ScR is shown in Fig. 1 (39–60)).
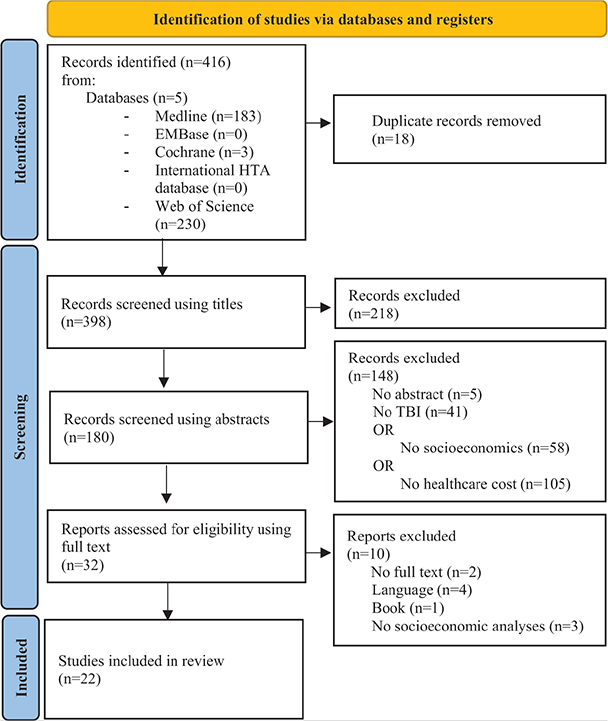
Fig. 1. Flow diagram of the selection process according to PRISMA-ScR.
Descriptive presentation of results
The descriptive results are presented in Table I. All the articles were published between 1988 and 2022. However, the topic was not very well explored in the period 1988–1999 (just a single article), and there was then an increasing trend in this research topic with 8 articles in 2000–2011 (36%) and 13 articles in 2012–2022 (59%). The majority of the studies were conducted in the USA (n = 17, 77%), Australia (n = 2, 9%), and Europe (n = 2, 9%). Most of the articles were quantitative studies (n = 20, 90%), with 14 (64%) adopting retrospective designs, using data from patient medical records and various databases (national registries or healthcare databases). Seven studies were prospective (32%), including 2 cross-sectional studies (9%), 1 qualitative exploratory survey (5%), and 1 literature review (5%). In 4 articles (18%), the objectives are general and do not mention economic or socioeconomic terms (48, 49, 54, 57). Regarding the methodological quality of the studies, 2 studies (9%) were rated as “adequate”, 9 as “good” (41%), and 11 as “strong” (50%).
Thematic organization of results
The labelling of data concerning costs and socioeconomic characteristics is presented in Table II, enabling the different variables used to be identified, harmonized, and compared with the studies. With reference to the cost typologies, 4 types of costs were found: direct medical costs, direct non-medical costs, indirect costs, and intangible costs. One typology defined as “other” concerned government assistance (States’ earned income tax credits, Federal income supplement programme or Government financial assistance established before or after TBI). Only 2 studies presented their perspective as recommended in guidelines for reporting cost analyses (9%). In the absence of this specification, the perspectives could be guessed, depending on the types of costs and orientations of the studies. The patient perspective was determined for 4 articles (18%), only 1 of which measured intangible costs (5%), the payer perspective for 8 articles (36%), and the societal perspective – the most complete perspective – for 10 studies (46%).
With regard to socioeconomic characteristics, 7 individual characteristics were used for the 22 articles and 2 ecological measures for 7 articles (32%), including a specific deprivation index (Index of Relative Socioeconomic Advantage and Disadvantage [IRSAD index]). According to the classification of the individual socioeconomic measures (“complete” or “partial”), only 2 articles measured the socioeconomic position “completely” (9%). For the 20 other articles, 5 did not explore any of the 3 main individual measures (23%).
Relationship between socioeconomic characteristics, TBI, and costs
Associations among socioeconomic characteristics, TBI incidence and complications, and costs described in papers were summarized. Table III conceptually classifies the articles according to 2 positions: the left column determined that socioeconomic characteristics were related to the occurrence of TBI and its costs. Most of the articles are classified in this position (n = 14, 64%). Although 3 articles did not find a significant association between socioeconomic characteristics, injury, and costs (14%) (40, 49, 60), the remaining 11 articles found a significant association between the most disadvantaged categories and increased costs, as well as a higher incidence or complications for the most disadvantaged (50%). Indeed, 6 articles described increased costs for the most disadvantaged (27%) (39, 44, 52, 53, 56, 59), and 7 articles described a more complex incidence or sequelae of injury, such as longer length of stay, development of complications, missed care, or increased mortality (32%) (41, 45, 48, 51–53, 59). The right column determined that socioeconomic characteristics were impacted by the occurrence of a TBI (and its costs). In this sense, the socioeconomic characteristics were modified and were therefore classified as consequences of the TBI and its costs (n = 8, 36%). Although Worthington (58) does not identify social role alteration during rehabilitation, 2 other articles point to increased divorce and decreased social interaction as a result of TBI (9%) (42, 47). Three other articles highlight the alteration of income, with a decrease in income and personal resources (43), taking out loans or the separation of property for the family (spouses and parents) to cover the costs associated with TBI (46), and over-indebtedness for TBI victims who have received rehabilitation (14%) (50).
Lastly, 5 articles highlight the impairment of occupation (or employment) with a threefold increase in the risk of job loss (47), an increased risk of absence from work (54), an increase in the number of people who are unemployed for up to 1 year (43), a change in employment for the family (spouses and parents) to cover the costs associated with TBI (46), a return to employment at 2 years for only half of pre-injury TBI and a wage at 2 years for only one-quarter of those who had a wage before the injury (55), and a decrease in productivity after TBI (23%) (42).
DISCUSSION
The purpose of this scoping review was to provide visibility on the association between socioeconomic characteristics and healthcare costs, in order to enable the evolution of care systems to remain relevant to the populations. Our work has identified very few studies analysing the costs of the care management of TBI victims according to their socioeconomic characteristics. This result highlights the lack of work integrating socioeconomic characteristics into efficiency for TBI management, which is a problem, considering the effect of social characteristics on the care pathway of TBI victims and the long-term consequences. The questions of efficiency and equity still remain unanswered.
Due to the heterogeneity of the articles that motivated the scoping review, all types of economic studies were included in the scoping (30), most of which were studies describing the costs of illness and none of which examined the efficiency of different strategies of care (e.g., cost–benefit analyses, cost–utility, etc.). Thus, the first common methodological element for all economic study designs was to identify the perspectives and cost typologies as recommended and which were missing in most cases (40, 44, 45, 47–49, 53, 55–58, 60). Some articles also sought to adopt a patient perspective to report on the economic consequences of TBI, whereby the out-of-pocket expenses could be a real debt for patients and their families. This may be the case in the USA, where people on low incomes do not have access to non-reimbursed care, so there will be a renunciation of care or even personal bankruptcy (61, 62). Intangible costs were also explored to highlight the impact of TBI in terms of reduced well-being for patients. These consequences can also have an impact on families, with the need to adapt the home, or to change or adapt their working hours in order to be more available to help with care or to cover costs. These results are in line with other authors who highlight the needs of families after the TBI of a relative (63, 64).
Regarding socioeconomic characteristics, we find that the vast majority of indicators used are individual measures but that very few articles explore the 3 main dimensions of socioeconomic position at an individual level (45, 55). We know that these individual variables are poorly recorded in routine care and, in a large proportion of articles, the retrospective design did not improve the quality of the collection and the approximation of socioeconomic position was therefore incomplete for most studies (36). In the absence of individual data, the socioeconomic approximation via ecological indices may be an alternative (32, 65). Currently, there are several validated and available deprivation indicators that allow, from an “easily accessible” variable, approximation of the socioeconomic position. Some US articles have used the household income by zip code as an ecological measure, based on income level (66). And only 1 article was able to use a specific ecological measure of deprivation constructed by crossing deprivation surveys and population census data (IRSAD index) (67).
The cross-analysis of costs and social characteristics allowed us to determine whether socioeconomic characteristics are associated with the occurrence of TBI or whether occurrence of a TBI alters the living conditions. Thus, a conceptual framework could be defined in which socioeconomic characteristics can either be related to the occurrence of a head injury or be impacted as a result of a head injury and its costs. TBI is not randomly distributed in the population and socioeconomic characteristics are involved in the occurrence of TBI. Many of the articles have highlighted that the incidence was higher, the recovery more complex, and the coverage of healthcare higher for the most disadvantaged categories (38–40, 43, 44, 47, 48, 51, 52, 55, 56, 58, 59). These results are in line with those of the authors who point out the higher incidence of TBI in disadvantaged populations (14, 68, 69). Moreover, the cost of care seems to vary according to the socioeconomic characteristics of individuals, but most of them highlight an increased cost of care for disadvantaged groups (39, 41, 44, 52, 53, 56, 59). Lastly, many of the articles highlight the fact that TBI and associated costs can affect living conditions, more particularly alteration of social role, alteration of level of income, and alteration of occupation or employment (42, 43, 46, 47, 50, 54, 55, 58). These results highlight the vulnerability of survivors who undergo long and complex rehabilitation processes with physical and cognitive rehabilitation and social support needs, sometimes for several years after their TBI. These results are consistent with recent results from Arigo and Haggerty (70) in the field of traumatic head injuries. They are also consistent with literature in the field of emergencies or hip fracture, where authors explain that the most disadvantaged populations have a higher cost of care and this relationship is partly due to a different state of health, with higher comorbidity and morbidity in this population (21–23). In a general population, Jayatunga et al. (24) highlight a social gradient, i.e., a gradual increase in costs as deprivation increases.
These elements once again call into question the assessment of severity, which is mainly based on clinical criteria at the time of initial management (use of the Glasgow coma scale). This assessment is currently contested as it is not a good indicator of the complex pathophysiology of TBI and disability (71). Indeed, although clinical assessment remains essential in guiding management and preventing complications, classification on these criteria is insufficient to guide prognosis and the therapies implemented are sub-optimal. Imaging, biomarkers, and pathology should be considered in the diagnostic criteria (72).
Occurrence of TBI appears to alter living conditions in our review. This work therefore suggests the need to carry out a detailed evaluation of the link between socioeconomic characteristics and the occurrence of TBI and to evaluate the costs associated with TBI according to these characteristics. Future work should focus on identifying populations at risk of poor recovery or deterioration following a TBI, and developing care pathways specifically for these groups, which acknowledge and work within the reality of the impact of socioeconomic position on recovery. The aim is then to construct more appropriate, effective, and equitable care programmes.
More generally, healthcare decisions should not be based solely on economic criteria, but should be modulated according to the socioeconomic characteristics of the users in order to integrate equity in these decisions. Efficiency and equity are closely linked. Indeed, if socioeconomic characteristics are not considered, healthcare programmes will only be efficient for part of the population and the care of the other users will require the implementation of additional interventions to compensate for the difference in efficiency between the different socioeconomic groups, and will therefore be more expensive. Some studies have demonstrated the added value in terms of cost-saving of taking these characteristics into account (74, 75).
Strength and limitations
The strength of this work lies in the detailed analysis of costs and socioeconomic characteristics, which allows these elements to be presented in an optimal and comparable way according to current standards. The scoping methodology has been followed in a systematic and rigorous way that permits the presentation of descriptive data from the selected studies and the analysis of their content. The weaknesses of this work are the lack of exhaustiveness of the databases consulted, even if they were targeted to answer the research question in a relevant way. Although searching by MeSH allows for more targeted results, free-text searching is essential for databases that do not have a thesaurus, but the exhaustiveness of the results remains limited. The language searched was filtered to French and English, and grey literature was not explored. These elements imply that some articles may have been missed. Lastly, evaluation of the quality of the data may be overestimated with the use of a general tool, the counterpart of which would be the lack of specificity to qualitative or economic evaluation of health care programmes’ methods.
Conclusion
To date, few articles have addressed the issue of socioeconomic characteristics in terms of risk or consequences of TBI and their costs. This lack is all the greater because the evaluation of these dimensions is suboptimal in these articles, which rarely follow the recommendations in relation to economic evaluation of healthcare programmes or the variables and indicators approximating deprivation are not used in a satisfactory manner. This work is a major step in highlighting the lack of evaluation of these dimensions, while their involvement and consequences seem to be important in the pathways of TBI patients. This scoping review could guide future research on the rigorous measurement of these indicators in order to model and design optimal care pathways according to individual characteristics.
REFERENCES
- GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 459. DOI: 10.1016/S1474-4422(18)30499-X
- Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung Y-C, Punchak M, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg 2018; 130: 1080–1097. DOI: 10.3171/2017.10.JNS17352
- Narain JP. Public health challenges in India: seizing the opportunities. Indian J Community Med Off Publ Indian Assoc Prev Soc Med 2016; 41: 85. DOI: 10.4103/0970-0218.177507
- Nyaaba GN, Stronks K, Aikins A de-Graft, Kengne AP, Agyemang C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: a synthesis of WHO country profile reports. BMC Public Health [serial on the Internet] 2017 [cited 2020 Oct 14]; 17. DOI: 10.1186/s12889-017-4199-6
- Asehnoune K, Lasocki S, Seguin P, Geeraerts T, Perrigault PF, Dahyot-Fizelier C, et al. Association between continuous hyperosmolar therapy and survival in patients with traumatic brain injury: a multicentre prospective cohort study and systematic review. Crit Care 2017; 21: 328. DOI: 10.1186/s13054-017-1918-4
- Myburgh JA, Cooper DJ, Finfer SR, Venkatesh B, Jones D, Higgins A, et al. Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. J Trauma Acute Care Surg 2008; 64: 854–862. DOI: 10.1097/TA.0b013e3180340e77
- Andelic N, Howe EI, Hellstrøm T, Sanchez MF, Lu J, Løvstad M, et al. Disability and quality of life 20 years after traumatic brain injury. Brain Behav 2018; 8: e01018. DOI: 10.1002/brb3.1018
- Andelic N, Bautz-Holter E, Ronning P, Olafsen K, Sigurdardottir S, Schanke A-K, et al. Does an early onset and continuous chain of rehabilitation improve the long-term functional outcome of patients with severe traumatic brain injury? J Neurotrauma 2011; 29: 66–74. DOI: 10.1089/neu.2011.1811
- Houngnandan AAB. Étude de l’association entre la sévérité des traumatismes crâniens et les inégalités sociales. 2014 [cited 2020 Sep 30]. Available from: https://papyrus.bib.umontreal.ca/xmlui/handle/1866/10824
- Pritchard E, Tsindos T, Ayton D. Practitioner perspectives on the nexus between acquired brain injury and family violence. Health Soc Care Community 2019; 27: 1283–1294. DOI: 10.1111/hsc.12770
- Santé Publique France. Épidémiologie des traumatismes crâniens en France et dans les pays occidentaux: Synthèse bibliographique, avril 2016. 2019: 66 p.
- Murphy J. Care of the patient with traumatic brain injury: urban versus rural challenges. Adv Emerg Nurs J 2004; 26: 231–236.
- Bonow RH, Barber J, Temkin NR, Videtta W, Rondina C, Petroni G, et al. The outcome of severe traumatic brain injury in Latin America. World Neurosurg 2018; 111: e82–e90. DOI: 10.1016/j.wneu.2017.11.171
- Ayton D, Pritchard E, Tsindos T. Acquired brain injury in the context of family violence: a systematic scoping review of incidence, prevalence, and contributing factors. Trauma Violence Abuse 2021; 22: 3–17. DOI: 10.1177/1524838018821951
- Leibson CL, Brown AW, Hall Long K, Ransom JE, Mandrekar J, Osler TM, et al. Medical care costs associated with traumatic brain injury over the full spectrum of disease: a controlled population-based study. J Neurotrauma 2012; 29: 2038–2049. DOI: 10.1089/neu.2010.1713
- Olesen J, Gustavsson A, Svensson M, Wittchen H-U, Jönsson B, CDBE2010 study group, et al. The economic cost of brain disorders in Europe. Eur J Neurol 2012; 19: 155–162. DOI: 10.1111/j.1468-1331.2011.03590.x
- Asamani JA, Alugsi SA, Ismaila H, Nabyonga-Orem J. Balancing equity and efficiency in the allocation of health resources: where is the middle ground? Healthc Basel Switz 2021; 9: 1257. DOI: 10.3390/healthcare9101257
- Li DG, Wong GX, Martin DT, Tybor DJ, Kim J, Lasker J, et al. Attitudes on cost-effectiveness and equity: a cross-sectional study examining the viewpoints of medical professionals. BMJ Open 2017; 7: e017251. DOI: 10.1136/bmjopen-2017-017251
- Pinho MM, Pinto Borges A. Relative importance assigned to health care rationing principles at the bedside: evidence from a Portuguese and Bulgarian survey. Health Care Manag 2017; 36: 334–341. DOI: 10.1097/HCM.0000000000000187
- Tardif P-A, Moore L, Boutin A, Dufresne P, Omar M, Bourgeois G, et al. Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: a retrospective multicenter cohort study. Injury 2017; 48: 94–100. DOI: 10.1016/j.injury.2016.10.042
- Glynn J, Hollingworth W, Bhimjiyani A, Ben-Shlomo Y, Gregson CL. How does deprivation influence secondary care costs after hip fracture? Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 2020; 31: 1573–1585. DOI: 10.1007/s00198-020-05404-1
- Asaria M, Doran T, Cookson R. The costs of inequality: whole-population modelling study of lifetime inpatient hospital costs in the English National Health Service by level of neighbourhood deprivation. J Epidemiol Community Health 2016; 70: 990–996. DOI: 10.1136/jech-2016-207447
- Colineaux H, Le Querrec F, Pourcel L, Gallart J-C, Azéma O, Lang T, et al. Is the use of emergency departments socially patterned? Int J Public Health 2018; 63: 397–407. DOI: 10.1007/s00038-017-1073-3
- Jayatunga W, Asaria M, Belloni A, George A, Bourne T, Sadique Z. Social gradients in health and social care costs: analysis of linked electronic health records in Kent, UK. Public Health 2019; 169: 188–194. DOI: 10.1016/j.puhe.2019.02.007
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. DOI: 10.1080/1364557032000119616
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst 2008; 6: 7. DOI: 10.1186/1478-4505-6-7
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci IS 2010; 5: 69. DOI: 10.1186/1748-5908-5-69
- O’Brien KK, Colquhoun H, Levac D, Baxter L, Tricco AC, Straus S, et al. Advancing scoping study methodology: a web-based survey and consultation of perceptions on terminology, definition and methodological steps. BMC Health Serv Res 2016; 16: 305. DOI: 10.1186/s12913-016-1579-z
- Kmet LM, Lee RC, Cook LS, Alberta Heritage Foundation for Medical Research. Standard quality assessment criteria for evaluating primary research papers from a variety of fields [serial on the Internet]. Edmonton, Alta.: Alberta Heritage Foundation for Medical Research; 2004 [cited 2021 Oct 13]. Available from: http://www.deslibris.ca/ID/200548
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005, 404 p.
- Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health J Int Soc Pharmacoeconomics Outcomes Res 2022; 25: 10–31. DOI: 10.1016/j.jval.2021.10.008
- Townsend P. Deprivation. J Soc Policy 1987; 16: 125–146. DOI: 10.1017/S0047279400020341
- Smith GD, Bartley M, Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ 1990; 301: 373–377.
- Galobardes B, Shaw M, Lawlor DA, Lynch JW. Indicators of socioeconomic position (part 1). J Epidemiol Community Health 2006; 60: 7–12. DOI: 10.1136/jech.2004.023531
- Galobardes B, Shaw M, Lawlor DA, Lynch JW. Indicators of socioeconomic position (part 2). J Epidemiol Community Health 2006; 60: 95–101. DOI: 10.1136/jech.2004.028092
- Lamy S, Molinié F, Daubisse-Marliac L, Cowppli-Bony A, Ayrault-Piault S, Fournier E, et al. Using ecological socioeconomic position (SEP) measures to deal with sample bias introduced by incomplete individual-level measures: inequalities in breast cancer stage at diagnosis as an example. BMC Public Health 2019; 19: 857. DOI: 10.1186/s12889-019-7220-4
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evid Implement 2015; 13: 141–146. DOI: 10.1097/XEB.0000000000000050
- Haber NA, Wieten SE, Rohrer JM, Arah OA, Tennant PWG, Stuart EA, et al. Causal and associational language in observational health research: a systematic evaluation. Am J Epidemiol 2022; 191: 2084–2097. DOI: 10.1093/aje/kwac137
- Boop S, Axente M, Weatherford B, Klimo P. Abusive head trauma: an epidemiological and cost analysis. J Neurosurg Pediatr 2016; 18: 542–549. DOI: 10.3171/2016.1.PEDS15583
- Dengler BA, Plaza-Wüthrich S, Chick RC, Muir MT, Bartanusz V. Secondary overtriage in patients with complicated mild traumatic brain injury: an observational study and socioeconomic analysis of 1447 hospitalizations. Neurosurgery 2020; 86: 374–382. DOI: 10.1093/neuros/nyz092
- Graves JM, Mackelprang JL, Moore M, Abshire DA, Rivara FP, Jimenez N, et al. Rural–urban disparities in health care costs and health service utilization following pediatric mild traumatic brain injury. Health Serv Res 2019; 54: 337–345. DOI: 10.1111/1475-6773.13096
- Hart T, Whyte J, Polansky M, Kersey-Matusiak G, Fidler-Sheppard R. Community outcomes following traumatic brain injury: impact of race and preinjury status. J Head Trauma Rehabil 2005; 20: 158–172. DOI: 10.1097/00001199-200503000-00004
- Johnstone B, Mount D, Schopp LH. Financial and vocational outcomes 1 year after traumatic brain injury. Arch Phys Med Rehabil 2003; 84: 238–241. DOI: 10.1053/apmr.2003.50097
- Kelly KA, Patel PD, Salwi S, Iii HNL, Naftel R. Socioeconomic health disparities in pediatric traumatic brain injury on a national level. J Neurosurg Pediatr 2021; 29: 335-341. DOI: 10.3171/2021.7.PEDS20820
- Klevens J, Schmidt B, Luo F, Xu L, Ports KA, Lee RD. Effect of the earned income tax credit on hospital admissions for pediatric abusive head trauma, 1995–2013. Public Health Rep Wash DC 1974 2017; 132: 505–511. DOI: 10.1177/0033354917710905
- McMordie WR, Barker SL. The financial trauma of head injury. Brain Inj 1988; 2: 357–364. DOI: 10.3109/02699058809150908
- Norup A, Kruse M, Soendergaard PL, Rasmussen KW, Biering-Sørensen F. Socioeconomic consequences of traumatic brain injury: a Danish nationwide register-based study. J Neurotrauma 2020; 37: 2694–2702. DOI: 10.1089/neu.2020.7064
- Piatt JH, Neff DA. Hospital care of childhood traumatic brain injury in the United States, 1997–2009: a neurosurgical perspective. J Neurosurg Pediatr 2012; 10: 257–267. DOI: 10.3171/2012.7.PEDS11532
- Ramey WL, Walter CM, Zeller J, Dumont TM, Lemole GM, Hurlbert RJ. Neurotrauma from border wall jumping: 6 years at the Mexican-American border wall. Neurosurgery 2019; 85: E502–E508. DOI: 10.1093/neuros/nyz050
- Relyea-Chew A, Hollingworth W, Chan L, Comstock BA, Overstreet KA, Jarvik JG. Personal bankruptcy after traumatic brain or spinal cord injury: the role of medical debt. Arch Phys Med Rehabil 2009; 90: 413–419. DOI: 10.1016/j.apmr.2008.07.031
- Reynolds WE, Page SJ, Johnston MV. Coordinated and adequately funded state streams for rehabilitation of newly injured persons with TBI. J Head Trauma Rehabil 2001; 16: 34–46. DOI: 10.1097/00001199-200102000-00006
- Salik I, Dominguez JF, Vazquez S, Ng C, Das A, Naftchi A, et al. Socioeconomic characteristics of pediatric traumatic brain injury patients. Clin Neurol Neurosurg 2022; 221: 107404. DOI: 10.1016/j.clineuro.2022.107404
- Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics 2006; 118: 483–492. DOI: 10.1542/peds.2005-2588
- Shafi R, Smith PM, Colantonio A. Assault predicts time away from work after claims for work-related mild traumatic brain injury. Occup Environ Med 2019; 76: 471–478. DOI: 10.1136/oemed-2018-105621
- Shigaki CL, Johnstone B, Schopp LH. Financial and vocational outcomes 2 years after traumatic brain injury. Disabil Rehabil 2009; 31: 484–489. DOI: 10.1080/09638280802240449
- Spitz G, McKenzie D, Attwood D, Ponsford JL. Cost prediction following traumatic brain injury: model development and validation. J Neurol Neurosurg Psychiatry 2016; 87: 173–180. DOI: 10.1136/jnnp-2014-309479
- Tilford JM, Aitken ME, Anand KJS, Green JW, Goodman AC, Parker JG, et al. Hospitalizations for critically ill children with traumatic brain injuries: a longitudinal analysis. Crit Care Med 2005; 33: 2074–2081. DOI: 10.1097/01.ccm.0000171839.65687.f5
- Worthington AD, Matthews S, Melia Y, Oddy M. Cost-benefits associated with social outcome from neurobehavioural rehabilitation. Brain Inj 2006; 20: 947–957. DOI: 10.1080/02699050600888314
- Yue JK, Upadhyayula PS, Avalos LN, Phelps RRL, Suen CG, Cage TA. Concussion and mild-traumatic brain injury in rural settings: epidemiology and specific health care considerations. J Neurosci Rural Pract 2020; 11: 23–33. DOI: 10.1055/s-0039-3402581
- Zonfrillo MR, Zaniletti I, Hall M, Fieldston ES, Colvin JD, Bettenhausen JL, et al. Socioeconomic status and hospitalization costs for children with brain and spinal cord injury. J Pediatr 2016; 169: 250–255. DOI: 10.1016/j.jpeds.2015.10.043
- Merritt CH, Taylor MA, Yelton CJ, Ray SK. Economic impact of traumatic spinal cord injuries in the United States. Neuroimmunol Neuroinflammation 2019; 6: 9. DOI: 10.20517/2347-8659.2019.15
- Wolff H, Gaspoz J-M, Guessous I. Health care renunciation for economic reasons in Switzerland. Swiss Med Wkly 2011; 141: w13165. DOI: 10.4414/smw.2011.13165
- Norup A, Perrin PB, Cuberos-Urbano G, Anke A, Andelic N, Doyle ST, et al. Family needs after brain injury: a cross cultural study. NeuroRehabilitation 2015; 36: 203–214. DOI: 10.3233/NRE-151208
- Røe C, Anke A, Arango-Lasprilla JC, Andelic N, Caracuel A, Rivera D, et al. The Family Needs Questionnaire-Revised: a Rasch analysis of measurement properties in the chronic phase after traumatic brain injury. Brain Inj 2020; 34: 1375–1383. DOI: 10.1080/02699052.2020.1802664
- Pornet C, Delpierre C, Dejardin O, Grosclaude P, Launay L, Guittet L, et al. Construction of an adaptable European transnational ecological deprivation index: the French version. J Epidemiol Community Health 2012; 66: 982–989. DOI: 10.1136/jech-2011-200311
- Thomas AJ, Eberly LE, Davey Smith G, Neaton JD, for the Multiple Risk Factor Intervention Trial (MRFIT) Research Group. ZIP-code-based versus tract-based income measures as long-term risk-adjusted mortality predictors. Am J Epidemiol 2006; 164: 586–590. DOI: 10.1093/aje/kwj234
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA) [serial on the Internet]. 2018 [cited 2023 Jan 4]. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~SOCIO-ECONOMIC%20INDEXES%20FOR%20AREAS%20(SEIFA)%202016~1
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 56–87. DOI: 10.1016/S1474-4422(18)30415-0
- Nunnari D, Bramanti P, Marino S. Cognitive reserve in stroke and traumatic brain injury patients. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 2014; 35: 1513–1518. DOI: 10.1007/s10072-014-1897-z
- Arigo D, Haggerty K. Social comparisons and long-term rehabilitation for traumatic brain injury: a longitudinal study. J Health Psychol 2018; 23: 1743–1748. DOI: 10.1177/1359105316669583
- Tenovuo O, Diaz-Arrastia R, Goldstein LE, Sharp DJ, van der Naalt J, Zasler ND. Assessing the severity of traumatic brain injury: time for a change? J Clin Med 2021; 10: 148. DOI: 10.3390/jcm10010148
- Majdan M, Brazinova A, Rusnak M, Leitgeb J. Outcome prediction after traumatic brain injury: comparison of the performance of routinely used severity scores and multivariable prognostic models. J Neurosci Rural Pract 2017; 8: 20–29. DOI: 10.4103/0976-3147.193543
- Saatman KE, Duhaime A-C, Bullock R, Maas AIR, Valadka A, Manley GT, et al. Classification of traumatic brain injury for targeted therapies. J Neurotrauma 2008; 25: 719–738. DOI: 10.1089/neu.2008.0586
- Kypridemos C, Collins B, McHale P, Bromley H, Parvulescu P, Capewell S, et al. Future cost-effectiveness and equity of the NHS Health Check cardiovascular disease prevention programme: microsimulation modelling using data from Liverpool, UK. PLoS Med 2018; 15: e1002573. DOI: 10.1371/journal.pmed.1002573
- Brown V, Ananthapavan J, Veerman L, Sacks G, Lal A, Peeters A, et al. The potential cost-effectiveness and equity impacts of restricting television advertising of unhealthy food and beverages to Australian Children. Nutrients 2018; 10: 622. DOI: 10.3390/nu10050622