ORIGINAL REPORT
CAREGIVING, PARTICIPATION, AND QUALITY OF LIFE OF CLOSEST NEXT OF KIN OF PERSONS LIVING WITH SPINAL CORD INJURY IN NORWAY
Annette HALVORSEN, MD1,2,3, Kristine PAPE, PhD3, Marcel POST, PhD4,5, Fin BIERING-SØRENSEN, PhD6, Monica ENGELSJORD7 and Aslak STEINSBEKK, PhD3
From the 1Clinic of Physical Medicine and Rehabilitation, Department of Spinal Cord Injuries, 2Department of Medical Quality Registries, St Olavs Hospital, Trondheim University Hospital, 3Department of Public Health and Nursing, Norwegian University of Science and Technology, Trondheim, Norway, 4Center of Excellence for Rehabilitation Medicine, UMC Utrecht Brain Centre, University Medical Centre Utrecht, University Utrecht and De Hoogstraat Rehabilitation, Utrecht, 5University of Groningen, University Medical Centre Groningen, Centre for Rehabilitation, Groningen, The Netherlands, 6Section for Spinal Cord Injuries, Department for Brain and Spinal Cord Injuries, Copenhagen University Hospital, Rigshospitalet and Institute for Clinical Medicine, University of Copenhagen, Denmark and 7User Representative, Oppdal, Norway
Objectives: To investigate how next of kin of persons with spinal cord injury (SCI) experience various life areas in terms of caregiving, participation, and quality of life, and the impact of personal characteristics of next of kin and SCI characteristics.
Design: Survey of next of kin linked to data on persons with SCI in the Norwegian SCI Registry.
Participants: A total of 73 next of kin identified by persons with SCI.
Methods: Outcome measures were caregiving (4 measures), participation (1 measure), and quality of life (2 measures).
Results: Participants (73% partners, 73% female, mean age 56.4 years) gave various support to the person with SCI and considered it important to care and were happy to do so. Three-quarters of participants reported good mental health and life satisfaction, while one-quarter reported high levels of caregiver strain, especially related to emotional adjustments. Higher levels of caregiver strain were reported by participants of working age (< 67 years), and by those with middle level education.
Conclusion: The majority of next of kin of persons living with SCI in Norway are doing well in most life areas. Caregiver strain may be reduced by strengthening the ability of next of kin to cope with emotional challenges.
LAY ABSTRACT
A spinal cord injury (SCI) often drastically disrupts the lives of both the individuals with SCI and the people surrounding them, such as family members. Caregiving for a loved one with SCI involves both physical and emotional investment. A survey was carried out of the caregivers of 73 persons living with SCI in Norway to assess their life situation. The study found that the majority of caregivers of persons living with SCI in Norway are doing well in most life areas. Three out of 4 caregivers reported good mental health and life satisfaction. All participants considered it important to care and most were happy to do so. Nevertheless, one-quarter reported high levels of strain, especially related to emotional adjustments. Most at risk for caregiver strain were participants of working age and those with secondary education. Caregiver strain may be reduced by strengthening the ability of the caregiver to cope with emotional challenges.
Key words: spinal cord injury; caregiver; caregiver burden; participation; quality of life; Norway.
Citation: J Rehabil Med 2022; 54: jrm00278. DOI: http://dx.doi.org/10.2340/jrm.v54.2162.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Feb 15, 2022; Epub ahead of print: Mar 9, 2022; Published: Apr 7, 2022
Correspondence address: Annette Halvorsen, Clinic of Physical Medicine and Rehabilitation, Department of Spinal Cord Injuries, St Olavs hospital, Trondheim University Hospital, Trondheim, Norway. E-mail: Annette.Halvorsen@stolav.no
Competing interests and funding: The authors have no conflicts of interest to declare. AH is the leader of NorSCIR, but had no role in granting access to or delivery of the NorSCIR data.
Spinal cord injury (SCI) often drastically disrupts the lives of both the individuals with SCI and the people surrounding them. Many next of kin (close relatives, spouses, etc.) provide extensive support to persons with SCI (1, 2). This support is often necessary for persons with SCI to continue living at home and to maintain their well-being (3). Previous studies have reported that between 25% and 50% of partners of persons with SCI experience high levels of caregiver burden (4, 5).
The level of caregiver burden can be influenced by caregiver characteristics, such as age, sex, level of education, occupation status, and the type of relationship between caregiver and care recipient (2, 4, 6). In addition, the personal and injury characteristics of the person with SCI receiving support impacts the support provided and the perceived caregiver burden (2). However, the majority of previous studies of next of kin are based on samples that are not representative of the population of next of kin of persons with SCI and on self-reported data on injury characteristics provided by the caregiver (2). Therefore, studies using clinical register data, which may be available from SCI quality registers, are needed to improve the trustworthiness of the data.
The demands placed on the next of kin of persons with SCI can affect various life areas. Next of kin can experience strained relationships, less control over life, increased stress, and financial difficulties (7–9). There are only a few studies on objective burden of support (1, 4, 10), caregiver participation (11), and positive caregiver experiences (12). These studies show that next of kin provide support in many different types of activities, and that the next of kin of persons with a more severe disability more often provide practical everyday support.
However, currently, most studies in this field are limited to measuring the impact of SCI on 1 or 2 life areas of next of kin, and the broader picture is thus lacking. The results of such a study with a broader approach can be used to identify groups of next of kin who are at risk.
Although Norway has a relatively good health and social system for persons with SCI (13) and the National Norwegian SCI registry (NorSCIR) provides a good overview of the SCI population (www.norscir.no), to date, no information about the next of kin of persons with SCI in Norway exists. This study utilized NorSCIR to recruit a representative sample with good-quality clinical data on SCI characteristics in order to study the life situation of closest next of kin of persons living with SCI in Norway.
This study aimed to describe the next of kin of persons with SCI in Norway and to identify how the personal characteristics of next of kin and the injury characteristics of the related person with SCI, influence different life areas of next of kin; caregiving (objective and subjective burden of care, and positive experiences), participation, and quality of life (QoL) (life satisfaction, and mental health).
METHODS
Study design
The study includes survey data from next of kin linked to data on persons with SCI in NorSCIR. It is part of a research project concerning participation and QoL among persons registered in NorSCIR between 2011 and 2017 and their next of kin.
Participants
During 2019, all persons in NorSCIR were invited to participate in the “Survey among persons with SCI”. Of the 651 invited persons with SCI, 339 participated (52%). All participants were asked to provide contact information for their designated next of kin so that the next of kin could be invited to participate in the “Next of kin survey”. Next of kin was defined in the questionnaire as “A person who provides unpaid support, or the one who is closest to you. Usually it is a partner or other close relative, such as parent, child or sibling”.
Procedures
A digital invitation was sent to all 92 designated next of kin. Those not registered with a digital mailbox or not answering the digital questionnaire were invited by post. Up to 2 reminders were sent to non-responders. To create awareness among those who were invited, general information about the study was published on the Facebook page and in the magazine of members of the Norwegian SCI consumer organization “LARS”.
Ethical approval for the study was obtained from the Regional Committee for Medical and Health Research Ethics in Central Norway (2018/294/REK midt).
Measures
Sociodemographic characteristics of next of kin. This information included sex, age, level of education (categorized as primary, middle and higher (college/university) level of education), personal income, vocational status (categorized as currently working or student, retirement pension, social welfare recipient, or other (homemaker, jobseeker)) status and type of relation to the person with SCI. Age was categorized into 3 groups (< 55, 55–67 and > 67 years), as the retirement age in Norway is 67 years. Personal income was categorized into 2 groups (below and above 500,000 Norwegian kroner per year (approximately 49,500 EUR)).
Spinal cord injury characteristics. Injury characteristics were obtained from NorSCIR, which contains data registered by clinicians using the definitions from the International SCI Core Data Set version 1.1 (14). Study variables included dates of discharge from rehabilitation care, cause of injury and neurological status at discharge from rehabilitation hospital. Causes were categorized as traumatic or non-traumatic. The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) was used to document neurological level of injury and the severity of SCI, as described by the American Spinal Injury Association (ASIA) Impairment Scale (AIS) (15). These characteristics were coded in 4 categories: Tetraplegia (C1–C8) AIS A, B or C; Tetraplegia (C1–C8) AIS D; Paraplegia (T1–S5) AIS A, B or C; Paraplegia (T1–S5) AIS D. None was registered with AIS E.
Outcome measures
Outcome measures were: caregiving (objective burden, subjective burden, and positive caregiver experience), participation, and quality of life, as described below.
Objective burden of care. The objective burden of care for next of kin was measured by a measure of types and frequency of support (1, 4). The measure includes 3 categories of support: activities of daily living (ADL) support (13 items), other practical support (9 items) and emotional support (2 items). Response categories are: never (1), sometimes (2), often (3) and always (4). The total score is the mean of the item scores (range 1–4). Translation of the questionnaire from Dutch to Norwegian was performed according to the guidelines from the World Health Organization (WHO) for the process of translation and adaptation of instruments (16).
Subjective burden of care. It has been recommended to measure subjective burden of care using 2 instruments that complement each other (17); 1 instrument that measures different dimensions of burden, and 1 instrument that measures the caregiver’s overall assessment of burden.
The Caregiver Strain Index (CSI) (18) evaluates strain related to care provision, by asking the responder to think of the person he/she is giving care to and to indicate if the following 13 dimensions apply to him/her (yes, no, not applicable), such as sleep disturbances, inconvenience, physical strain, and emotional adjustment. The total CSI score is calculated by summing up the “yes” responses, ranging from 0 to 13. Positive responses to 7 or more items on the index indicate a greater level of strain (4, 18). The CSI has been validated (18, 19) and the available Norwegian version was used (20).
The self-rated burden (SRB) (21) is a single question; “How demanding is it for you to provide care at the moment?”. It is scored on an 11-point scale, from 0 “not demanding at all” to 10 “much too demanding”. SRB is feasible and considered to be at least as valid as other measures of burden (21). It was translated into Norwegian for this study.
Positive caregiver experiences. To describe the positive experiences of caregiving, the current study used the 5 positive items that were added to the CSI in the Caregiver Strain Index Expanded (22). Positive experiences related to care provision are assessed by asking the responder to think of the person he/she is giving care to and to indicate if the subsequent 5 dimensions apply to him/her (yes, no, not applicable): such as I am happy to care, and I handle the care fine.
Participation. The Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-Participation) Frequency subscale was used to measure the frequency of, and time spent on participation in different activities (23). The USER-Participation showed good validity (23), can also be used in people without physical disabilities, such as next of kin, and the 3 scales can be used separately (24). The English version of the USER-Participation was translated into Norwegian using the same guidelines (16). The frequency scale consists of 2 parts. Part A comprises 4 items on the number of hours spent per week on vocational activities, with answering options ranging from not at all (scored 0), to 36 h or more (scored 5). Part B comprises 7 items on leisure and social activities frequency in the last 4 weeks, with answering options ranging from never (scored 0) up to 19 times or more (scored 5). The sum score based on all applicable items is converted to a 0–100 scale, with higher scores indicating higher levels of participation.
Quality of life. QoL was measured, using 2 constructs, as described in the literature (25–27); life satisfaction and mental health. Life satisfaction was measured with a selection of 5 items from the World Health Organization Quality of life assesment-BREF (WHOQOL-BREF) assessment covering satisfaction with overall QoL, health, daily activities, relationships, and living conditions (World Health Organization Quality of life assessment; WHOQOL-5) (28). Response options range from very poor/very dissatisfied (scored 1) to very good/very satisfied (scored 5) for each item, yielding a total score between 5 (very poor/dissatisfied) and 25 (very good/satisfied).
Mental health was measured with the Mental Health subscale of the Medical Outcomes Study Short Form Health Survey (MHI-5) (29). The MHI-5 consists of 5 items on emotional status concerning nervousness, sadness, peacefulness, depressed mood, and happiness. Respondents rated the frequency of each item during the previous 4 weeks on a 5-point scale. The score is converted to a total score between 0 (lowest mental health) and 100 (highest mental health).
Statistical analysis
Descriptive statistics were used to assess the personal characteristics of the participating next of kin, and injury characteristics of their relation with SCI. Characteristics of participants in the “Survey among persons with SCI” who did or did not have next of kin participating in the current study were compared to assess the representativeness of the next of kin sample.
In separate analyses, with objective burden, participation and each dimension of subjective burden (CSI and SRB) and QoL (WHO QoL5 and MHI-5) as dependent variables, the associations with characteristics of next of kin and the injury characteristics of their relation with SCI as independent variables were assessed. Multivariable linear regression analyses, adjusted for sex and age as a continuous variable, were carried out. Stata® version 16.0 (StataCorp, College Station, TX, USA) was used for all statistical analyses.
RESULTS
Of the 339 persons with SCI who participated in the “Survey among persons with SCI”, 92 persons (27%) provided contact information of their designated next of kin who were invited to participate in this study. Of the 92 persons invited to participate in the “Next of kin survey”, 73 participated (79%) (Fig. 1).
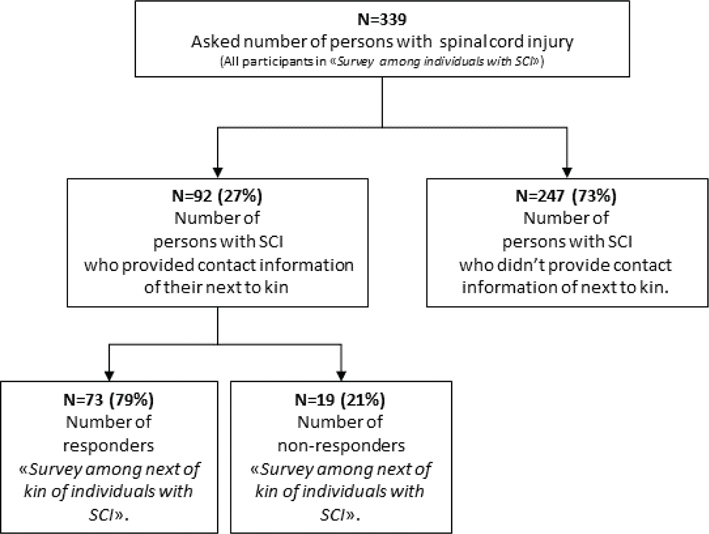
Fig. 1. Flow chart of participants in the survey of next of kin of individuals with spinal cord injury (SCI).
Of the related persons with SCI, 59% had a traumatic SCI, 34% had tetraplegia AIS D and the mean time since discharge from primary rehabilitation was 4.2 years (standard deviation (SD) 1.8, range 1–8 years), at the time of the study (Table I). No significant differences in the characteristics of the persons with SCI were observed between those with vs without related to next of kin participating in this study (Table I).
| Characteristics of persons with SCI | Participating* (N = 73) | Asked persons with SCI** (N = 266) | p-valuea for comparison of responders with asked persons with SCI |
| Age, years, Mean (SD) | 59 (17.2) | 57 (15.9) | 0.5734 |
| Sex, N (%) | 0.118 | ||
| Male | 47 (64) | 196 (74) | |
| Female | 26 (36) | 70 (26) | |
| Impairment groups (Neurological level and AIS), N (%) | 0.292 | ||
| Tetraplegia, AIS A–C | 10 (14) | 24 (9) | |
| Tetraplegia, AIS D–E | 25 (34) | 77 (29) | |
| Paraplegia, AIS A–C | 18 (25) | 58 (22) | |
| Paraplegia, AIS D–E | 20 (27) | 103 (39) | |
| Unknown or not applicable | 0 (0) | 4 (2) | |
| Time since discharge, years, Mean (SD) | 4.2 (1.8) | 4.5 (1.9) | 0.3467 |
| Cause of injury, N (%) | 0.847 | ||
| Traumatic | 43 (59) | 160 (60) | |
| Non-traumatic | 30 (41) | 106 (40) | |
| *Persons with SCI related to next of kin participating in the current study. | |||
| **Persons with SCI who were asked to provide contact information for next of kin. | |||
| ap-value from t-test for continuous and χ2 test for categorical, with Fisher’s exact test for impairment groups. | |||
| SCI: spinal cord injury; SD: standard deviation; AIS: American Spinal Injury Association Impairment Scale. | |||
Descriptive characteristics of the next of kin are shown in Table II. Mean age at the time of the survey was 56 years (median 59 years, range 20–79 years), 73% were female, and 55% had a high level of education (college/university). The majority were a spouse or partner of the person with SCI (73%), and 72% lived together (Table II).
Caregiving – objective burden of care
The mean support score for all respondents was 1.6 (SD 0.5) on a 1–4 scale (Table III). Next of kin of persons with tetraplegia AIS A–C reported providing more support than next of kin of persons with less severe disability.
| Characteristics | Objective burden | Subjective burden | Participation | Quality of life | |||||||||
| Support Score (Range 1–4) | Caregiver Strain Index (CSI) (Range 0–13) | Caregiver burden (SRB) (Range 0 –10) | USER-P frequency (Range 0-100) | Life satisfaction (WHO QoL-5) (Range 5–25) | Mental health (MHI-5) (Range 0–100) | ||||||||
| Variable | N (%) | Mean (95% CI) | p-value | Mean (95% CI) | p-value | Mean (95% CI) | p-value | Mean (95% CI) | p-value | Mean (95% CI) | p-value | Mean (95% CI) | p-value |
| Mean score (SD) | 1.6 (0.5) | 3.7 (3.4) | 3.2 (2.8) | 39.3 (9.0) | 19.9 (2.9) | 78.0 (13.8) | |||||||
| Demographic and social variables next of kin | |||||||||||||
| Age-groups, years | |||||||||||||
| < 55 | 28 (38) | 1.5 (1.3–1.7) | Ref | 4.3 (3.0–5.5) | Ref | 2.8 (1.8–3.9) | Ref | 38.6 (35.3–41.9) | Ref | 19.0 (17.9–20.1) | Ref | 75.0 (69.9–80.1) | Ref |
| 55–67 | 29 (40) | 1.7 (1.6–1.9) | 0.102 | 4.3 (3.1–5.5) | 0.991 | 3.5 (2.5–4.6) | 0.352 | 42.0 (38.7–45.3) | 0.153 | 20.3 (19.2–21.3) | 0.106 | 78.4 (73.4–83.5) | 0.344 |
| > 67 | 16 (22) | 1.6 (1.3–1.8) | 0.878 | 1.7 (0.1–3.4) | 0.017c | 3.3 (1.9–4.6) | 0.627 | 35.8 (31.4–40.2) | 0.311 | 21.0 (19.6–22.4) | 0.029c | 82.5 (75.7–89.3) | 0.084 |
| Sex | |||||||||||||
| Male | 20 (27) | 1.7 (1.4–1.9) | Ref | 2.7 (1.2–4.2) | Ref | 2.2 (1.0–3.5) | Ref | 39.8 (35.7–43.9) | Ref | 20.2 (18.9–21.5) | Ref | 76.5 (70.4–82.6) | Ref |
| Female | 53 (73) | 1.6 (1.5–1.7) | 0.709 | 4.1 (3.2–5.0) | 0.124 | 3.6 (2.8–4.3) | 0.072 | 39.2 (36.7–41.7) | 0.808 | 19.8 (19.0–20.6) | 0.650 | 78.6 (74.8–82.3) | 0.572 |
| Level of education | |||||||||||||
| Primary | 8 (11) | 1.3 (0.9–1.6) | Ref | 1.7 (0–4.0) | Ref | 3.3 (1.3–5.3) | Ref | 33.5 (27.2–39.8) | Ref | 19.2 (17.2–21.3) | Ref | 81.8 (72.0–91.6) | Ref |
| Middle | 25 (34) | 1.8 (1.6–2.0) | 0.005c | 4.6 (3.3–5.9) | 0.034c | 3.6 (2.5–4.8) | 0.773 | 37.2 (33.7–40.7) | 0.303 | 19.2 (18.0–20.4) | 0.954 | 77.3 (71.8–82.8) | 0.427 |
| Higher | 40 (55) | 1.6 (1.4–1.7) | 0.122 | 3.6 (2.5–4.7) | 0.147 | 2.9 (2.0–3.8) | 0.687 | 41.8 (39.0–44.6) | 0.019c | 20.5 (19.6–21.4) | 0.264 | 77.7 (73.3–82.1) | 0.456 |
| Vocational status | |||||||||||||
| Currently working or student | 46 (63) | 1.6 (1.4–1.8) | Ref | 3.9 (2.8–5.0) | Ref | 3.0 (2.1–3.8) | Ref | 41.3 (38.6–44.0) | Ref | 19.9 (18.9–20.9) | Ref | 77.5 (73.1–81.9) | Ref |
| Retirement pension | 20 (27) | 1.5 (1.3–1.8) | 0.651 | 3.1 (1.2–4.9) | 0.504 | 3.2 (1.8–4.7) | 0.762 | 38.7 (34.1–43.3) | 0.370 | 20.4 (18.8–22.0) | 0.629 | 79.7 (72.2–87.2) | 0.652 |
| Social welfare recipient | 7 (10) | 2.0 (1.6–2.4) | 0.064 | 4.7 (2.1–7.3) | 0.575 | 4.6 (2.5–6.7) | 0.162 | 28.1(21.6–34.5) | < 0.001c | 18.8 (16.5–21.0) | 0.361 | 76.7 (66.1–87.2) | 0.885 |
| Personal income (Norwegian kroner per year) | |||||||||||||
| Below 500,000 | 36 (51) | 1.7 (1.5–1.8) | Ref | 3.5 (2.3–4.7) | Ref | 3.3 (2.4–4.2) | Ref | 37.8 (35.1–40.6) | Ref | 19.4 (18.4–20.3) | Ref | 79.6 (74.9–84.2) | Ref |
| 500,000 and above | 34 (49) | 1.6 (1.4–1.8) | 0.551 | 4.0 (2.8–5.2) | 0.566 | 3.1 (2.1–4.0) | 0.733 | 42.2 (39.3–45.0) | 0.034c | 20.5 (19.4–21.5) | 0.123 | 77.1 (72.3–81.9) | 0.468 |
| Relation to patient | |||||||||||||
| Partner | 53 (73) | 1.7 (1.5–1.8) | Ref | 4.1 (3.2–5.0) | Ref | 3.4 (2.6–4.2) | Ref | 38.2 (35.7–40.7) | Ref | 19.8 (19.0–20.6) | Ref | 77.9 (74.1–81.7) | Ref |
| Family or other | 20 (27) | 1.5 (1.2–1.7) | 0.106 | 2.8 (1.2–4.3) | 0.153 | 2.6 (1.4–3.9) | 0.300 | 42.3 (38.2–46.4) | 0.101 | 20.2 (18.9–21.6) | 0.593 | 78.3 (72.0–84.5) | 0.927 |
| Injury characteristics of the related person with SCI | |||||||||||||
| Time since discharge | |||||||||||||
| 4 years or less | 36 (49) | 1.6 (1.5–1.8) | Ref | 3.5 (2.4–4.7) | Ref | 3.1 (2.2–4.0) | Ref | 39.0 (35.9–42.0) | Ref | 19.7 (18.8–20.7) | Ref | 79.2 (74.7–83.8) | Ref |
| More than 4 years | 37 (51) | 1.6 (1.5–1.8) | 0.999 | 3.9 (2.8–5.0) | 0.620 | 3.3 (2.4–4.2) | 0.744 | 39.7 (36.7–42.7) | 0.731 | 20.1 (19.1–21.1) | 0.594 | 76.8 (72.3–81.3) | 0.460 |
| Impairment groups (level and AIS) | |||||||||||||
| Tetraplegia A,B,C | 10 (14) | 2.1 (1.8–2.4) | Ref | 4.7 (2.6–6.8) | Ref | 3.5 (1.8–5.3) | Ref | 43.2 (37.4–49.0) | Ref | 20.9 (19.0–22.7) | Ref | 73.2 (64.6–81.9) | Ref |
| Tetraplegia D | 25 (34) | 1.4 (1.2–1.6) | < 0.001c | 2.5 (1.1–3.8) | 0.072 | 2.3 (1.2–3.4) | 0.216 | 38.5 (34.8–42.2) | 0.180 | 20.5 (19.3–21.7) | 0.712 | 77.0 (71.5–82.5) | 0.471 |
| Paraplegia A,B,C | 18 (25) | 1.7 (1.5–1.9) | 0.012c | 3.5 (2.0–5.1) | 0.362 | 3.7 (2.4–5.0) | 0.877 | 39.2 (34.9–43.6) | 0.276 | 19.0 (17.6–20.4) | 0.104 | 78.9 (72.5–85.4) | 0.295 |
| Paraplegia D | 20 (27) | 1.6 (1.4–1.8) | 0.003c | 5.0 (3.5–6.4) | 0.842 | 3.7 (2.5–4.9) | 0.888 | 38.5 (34.4–42.6) | 0.192 | 19.6 (18.4–20.9) | 0.274 | 80.8 (74.7–86.9) | 0.157 |
| USER-P freq: Frequency scale of the Utrecht Scale for Evaluation of Rehabilitation-Participation; WHOQoL-5: World Health Organization Quality of life assessment; MHI-5: Mental Health subscale of the Medical Outcomes Study Short Form Health Survey; SCI: spinal cord injury; AIS: American Spinal Injury Association Impairment Scale; Ref: reference. | |||||||||||||
| aAll variables except sex and age were adjusted for sex, age. | |||||||||||||
| bN vary from 69 to 73 for each variable due to missing data, or preferring not to answer. | |||||||||||||
| cp-value < 0.05 from linear regression. | |||||||||||||
The types and frequencies of support given by next of kin are described in Table IV. Regarding support for ADL, most support was given in preparing meals (44%). This was followed by providing outdoor transportation and various “helping hands” throughout the day. Generally, less support was reported regarding “other practical support”, where most support was given when visiting a doctor (16%). Emotional support in terms of comforting and learning to live with SCI was given often or always by more than one-quarter of next of kin.
Caregiving – subjective burden of care
The mean overall SRB score was 3.2, and the mean total CSI score was 3.7 (Table III). CSI item scores are shown in Table V. The most frequently endorsed item was “emotional adjustments” (55%), followed by “Some behaviour is upsetting” (51%). Approximately one-quarter (19 persons) of the next of kin reported a high level of caregiver strain (CSI score ≥ 7 points).
Caregiving – positive caregiver experiences
Nearly all of the next of kin responded that they found it important to care and were happy to do so, and perceived that their care was appreciated (97%) (Table VI). Most (64%) reported having enough time for themselves, but this proportion was considerably lower (30%) among next of kin caring for a person with the most severe impairment (tetraplegia AIS A–C).
Participation
The mean USER-Participation Frequency score was 39.3 (Table III). The mean vocational sub-score was 30.0 (SD 11.9), and the mean leisure and social activity sub-score 48.7 (SD 13.5) (detailed scores in Table SI).
Quality of life
For life satisfaction, the mean WHO QoL-5 score was 19.9 (Table III, detailed scores in Table SII). Four in 5 (78%) rated their QoL good or very good. For mental health, the mean MHI-5 score was 78.0 (Table III, detailed scores in Table SIII).
Regression analyses
Table III shows the results of the regression analyses. Only a few of the characteristics showed significant associations with the various life areas. Next of kin in the retirement age group (> 67 years) reported higher life satisfaction (WHOQoL-5) and less caregiver strain (CSI) compared with those in the other age groups. Those having a middle level of education provided more support and had higher levels of caregiver strain (CSI) compared with those with a primary and a higher level of education. Female next of kin tended to report higher levels of overall burden (SRB) than males. The frequency of participation increased with higher levels of education and higher income. Next of kin who were social welfare recipients showed lower participation scores compared with those working.
Being the next of kin of a person in impairment group tetraplegia AIS A–C (most severe disability) was associated with reporting higher objective burden of care. Otherwise, no consistent patterns were found between SCI injury characteristics and the life areas reported by next of kin.
DISCUSSION
In this survey of 73 next of kin, investigating how they experience various life areas, 3 out of 4 next of kin reported good mental health and life satisfaction. All participants considered it important to care, and almost all were happy to do so. Nevertheless, one-quarter of next of kin experienced high levels of subjective burden, as measured by CSI, especially related to emotional adjustments.
Only a few of the studied characteristics showed significant associations with different life areas, such as that those of working age and having a middle level of education had higher levels of caregiver strain, and that female next of kin tended to express higher levels of overall burden than males. The only SCI injury characteristic associated with a life area of next of kin was that next of kin of a person in the impairment group tetraplegia AIS A–C (most severe disability) reported a higher objective burden of care.
Life areas most influenced
A literature review regarding the impact of SCI on the QoL of family members showed that depression, anxiety, and reduced satisfaction with life were commonly reported (9). This is in contrast with the findings of the current study, in which 4 in 5 (78%) next of kin rated their QoL good or very good, and their mean mental health score was similar to this score among the general population in Norway (MHI-5 score of 79.5) (30). Furthermore, many reported positive caregiving experiences. Although few studies have investigated whether caregiving represents meaning and purpose (31), it has been shown that partners of persons with SCI who indicated positive effects of caregiving report better mental health (32). More research on the positive aspects of caregiving in future research is therefore warranted to increase awareness and to clarify how this contributes to the QoL of caregivers.
ADL and other practical support were given more often by next of kin of persons with serious disability, while fewer differences were seen between the groups with regard to emotional support. Similar findings were reported in 2 Dutch studies (1, 4). Although next of kin in the current study provided less support to persons with a less severe injury, compared with a previous study including only those who use wheelchairs (4), the proportions that provided support with outdoor transportation were similar (approximately 1 in 4). One reason is that outdoor transportation may be more challenging for disabled people in Norway, due to the demographics of Norway, with long distances, and long winters with much snow.
This study showed that emotional support was one of the types of support provided most, and emotional adjustments were the most frequently perceived strain, but that the severity of the SCI did not seem to influence either. Similar results have been found in other caregiver studies, e.g. advanced cancer (20), but this has not been reported in other SCI studies. This finding could be explained by an association between mental health of the patient and mental health of the next of kin (4), as they have a close relationship and are likely to influence each other.
Impact of next of kin characteristics
Next of kin of working age and with a middle level of education experienced more subjective burden compared with those who were retired or with higher or lower education. This is the opposite of the findings of a study by Post et al., in which the researchers concluded that the increasing age of partners was a significant predictor of caregiver burden (1). A possible explanation is that elderly persons with SCI in Norway receive paid support more often than those in the Netherlands, thus reducing the burden on next of kin. Alternatively, the use of different measures could have caused this difference. A literature review on the common determinants of caregiver burden in Western countries showed that the age of the caregiver was not a consistent predictor of caregiver burden (33).
One-quarter of the current participants experienced high levels of burden, lower than the 43% in a study among Dutch persons with SCI using a wheelchair (4), but similar to the results from another Dutch SCI study (5). The current finding, that female carers tended to report higher levels of overall burden, was also found in a literature review (33) and other SCI caregiver studies (1). This sex difference in caregiving burden could be related to women experiencing more secondary stressors (relational and financial problems, problems combining different tasks) (34).
Impact of SCI characteristics
Objective burden was the only life area of the next of kin that was influenced by the severity of the injury. Being the next of kin of a person with most severe disability (tetraplegia AIS A–C) was associated with reporting higher objective burden of care compared with next of kin of a person with less severe disability (paraplegia A–D or tetraplegia D). This finding is in line with findings from another study, which found that partners of individuals with tetraplegia provided support more often (4). However, they did not distinguish between the level of completeness (AIS A, B, C or D) within the tetraplegia group (4). Notably, next of kin of persons with paraplegia D tended to report almost similar results for subjective burden of care compared with next of kin of persons with tetraplegia AIS A–C. This finding was unexpected because other studies have indicated a strong association between the severity of disability, level of neurological injury, and the subjective burden of care (1, 35, 36). An explanation could be that individuals with less severe disability experience similar “hidden disabilities”, such as incontinence and pain, as their more severely disabled counterparts (37).
Other factors influencing life areas
Life areas of next of kin could be influenced by other factors, such as secondary conditions, coping -behaviour, mood or occupational status of the person with SCI. Findings in the study of Conti et al. from Italy indicated that a reduction in secondary SCI conditions, such as chronic pain and urinary tract infections, was related to less caregiver burden (38). Khazaeipour et al. found in a study from Iran that caregivers’ burden was lower when the related person with SCI had a job (36). Thus, more research is needed to gain a more comprehensive understanding of how the life of those who are next of kin to a person with SCI is experienced and of which factors influence this.
Study strengths and limitations
This is the first study of next of kin of patients with SCI in Norway. The main strength is the comprehensive approach, covering several life areas and the linkage between patient data from a national medical SCI quality registry and survey data. In contrast to the majority of other SCI caregiver studies that are based on self-reported injury data provided by the caregiver (2), the current study collected injury data from a national medical SCI quality registry, hence these data are provided by clinicians. The current study combined the variables of the neurological level of injury and severity of the SCI into the recommended impairment categories (39). We have not found any SCI studies using this classification in relationship with caregiver burden. The involvement of a user representative as a member of our research team, who used personal experience to provide input to all steps, from the study design to reporting the results, has ensured an additional perspective on the findings and contributes toward providing people with SCI and their next of kin a voice in the research process.
This study has some limitations. Only 27% of the persons with SCI provided contact information for their next of kin and, consequently, the sample size was small. It might be that persons with SCI with a poor relationship with their next of kin were less interested in providing contact information. The non-responder analysis, however, showed that the persons with SCI whose next of kin participated were reasonable representative of persons with SCI in the register. However, the generalizability of the findings is hampered by the low response rate.
CONCLUSION
A significant majority of next of kin of persons with SCI experience that it is important to provide care, and they are happy to do so. Strengthening the experience of positive aspects of caregiving may enhance better mental health of next of kin. Nevertheless, one-quarter of next of kin in the current study experienced high levels of caregiver strain, especially regarding the need for emotional adjustments. Most at risk of caregiver strain are those of working age (< 67 years), and those with middle level of education. In order to reduce the subjective burden of care, it seems necessary to increase the ability of next of kin to cope with the emotional challenges related to their caregiver role. Interventions, such as caregiver counselling, could be useful to achieve this. Injury characteristics had only a minor impact on the various aspects of the lives of next of kin caregivers. Although more research is needed, the findings of this study indicate that there are aspects of the life of the closest next of kin of a person with SCI that should be considered during SCI patient rehabilitation, in order to support the everyday life of caregivers.
ACKNOWLEDGEMENTS
The authors thank all the study participants for their time and effort in responding to the questionnaire, and all persons with SCI who were willing to ask their closest next of kin to participate and to provide contact information. We further thank the 3 SCI specialized centres, at Haukeland University Hospital, St Olavs University Hospital and Sunnaas Rehabilitation Hospital, for registration in NorSCIR, the steering committee of Norwegian SCI registry (NorSCIR) for providing access to the data, and Ann Louise Pettersen for providing the data delivery. Thanks are due to Albert Verhagen, Ingrid Riphagen, Wilma van de Veen, and Lars-Magnus Halvorsen for their contribution to the translations. The funding for the research project that this study was part of was provided by the Dam Foundation (grant number 2018/FO198620), the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology (NTNU) (grant number 18/420) and the joint research committee between St Olavs Hospital HF and the Faculty of Medicine and Health Sciences at NTNU (grant number 2018/42795).
REFERENCES
- Post MWM, Bloemen J, de Witte LP. Burden of support for partners of persons with spinal cord injuries. Spinal Cord 2005; 43: 311–319.
- Smith EM, Boucher N, Miller WC. Caregiving services in spinal cord injury: a systematic review of the literature. Spinal Cord 2016; 54: 562–569.
- Bickenbach J, Officer A, Shakespeare T, von Groote P, et al. International perspectives on spinal cord injury. Geneva: World Health Organization; 2013. report number: 9241564660.
- Scholten EWM, Kieftenbelt A, Hillebregt CF, de Groot S, Ketelaar M, Visser-Meily JMA, et al. Provided support, caregiver burden and well-being in partners of persons with spinal cord injury 5 years after discharge from first inpatient rehabilitation. Spinal Cord 2018; 56: 436–446.
- Backx APM, Spooren AIF, Bongers-Janssen HMH, Bouwsema H. Quality of life, burden and satisfaction with care in caregivers of patients with a spinal cord injury during and after rehabilitation. Spinal Cord 2018; 56: 890–899.
- Adhikari SP, Gurung G, Khadka B, Rana C. Factors influencing depression in individuals with traumatic spinal cord injury and caregivers’ perceived burden in a low-income country: a cross-sectional study. Spinal Cord 2020; 58: 1112–1118.
- Boschen KA, Tonack M, Gargaro J. The impact of being a support provider to a person living in the community with a spinal cord injury. Rehabil Psychol 2005; 50: 397–407.
- Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. The Gerontologist 1986; 26: 260–266.
- Lynch J, Cahalan R. The impact of spinal cord injury on the quality of life of primary family caregivers: a literature review. Spinal Cord 2017; 55: 964–978.
- Gemperli A, Rubinelli S, Zanini C, Huang J, Brach M, Pacheco Barzallo D. Living situation of family caregivers of persons with spinal cord injury. J Rehabil Med 2020; 52: jrm00124.
- Ellenbogen PS MM, Jackson MN, Barret K. The impact of spinal cord injury on the employment of family caregivers. J Vocational Rehabil 2006; 1: 35-44.
- Charlifue SB, Botticello A, Kolakowsky-Hayner SA, Richards JS, Tulsky DS. Family caregivers of individuals with spinal cord injury: exploring the stresses and benefits. Spinal Cord 2016; 54: 732–736.
- Strom V, Manum G, Leiulfsrud A, Wedege P, Rekand T, Halvorsen A, et al. People with spinal cord injury in Norway. Am J Phys Med Rehabil 2017; 96: S99–S101.
- DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International Spinal Cord Injury Core Data Set. Spinal Cord 2006; 44: 535–540.
- Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
- Organization WH. Process of translation and adaptation of instruments. Available from: http://www.who.int/substance_abuse/research_tools/translation/en/ 2009
- van Exel NJ, Brouwer WB, van den Berg B, Koopmanschap MA, van den Bos GA. What really matters: an inquiry into the relative importance of dimensions of informal caregiver burden. Clin Rehabil 2004; 18: 683–693.
- Robinson BC. Validation of a Caregiver Strain Index. J Gerontol 1983; 38: 344–348.
- Post MW, Festen H, van de Port IG, Visser-Meily JM. Reproducibility of the Caregiver Strain Index and the Caregiver Reaction Assessment in partners of stroke patients living in the Dutch community. Clin Rehabil 2007; 21: 1050–1055.
- Lohne V, Miaskowski C, Rustoen T. The relationship between hope and caregiver strain in family caregivers of patients with advanced cancer. Cancer Nurs 2012; 35: 99–105.
- van Exel NJ, Scholte op Reimer WJ, Brouwer WB, van den Berg B, Koopmanschap MA, van den Bos GA. Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: a comparison of CSI, CRA, SCQ and self-rated burden. Clin Rehabil 2004; 18: 203–214.
- Al-Janabi H, Frew E, Brouwer W, Rappange D, Van Exel J. The inclusion of positive aspects of caring in the Caregiver Strain Index: tests of feasibility and validity. Int J Nurs Stud 2010; 47: 984–993.
- Post MW, van der Zee CH, Hennink J, Schafrat CG, Visser-Meily JM, van Berlekom SB. Validity of the Utrecht Scale for Evaluation of Rehabilitation-Participation. Disabil Rehabil 2012; 34: 478–485.
- Cox V, Schepers V, Ketelaar M, van Heugten C, Visser-Meily A. Participation restrictions and satisfaction with participation in partners of patients with stroke. Arch Phys Med Rehabil 2020; 101: 464–471.
- van Leeuwen CM, Kraaijeveld S, Lindeman E, Post MW. Associations between psychological factors and quality of life ratings in persons with spinal cord injury: a systematic review. Spinal Cord 2012; 50: 174–187.
- Post M, Noreau L. Quality of life after spinal cord injury. J Neurol Phys Ther 2005; 29: 139–146.
- Halvorsen A, Pape K, Post MWM, Biering-Sorensen F, Mikalsen S, Hansen AN, et al. Participation and quality of life in persons living with spinal cord injury in Norway. J Rehabil Med 2021; 53: jrm00217.
- Geyh S, Fellinghauer BA, Kirchberger I, Post MW. Cross-cultural validity of four quality of life scales in persons with spinal cord injury. Health Qual Life Outcomes 2010; 8: 94.
- van Leeuwen CM, van der Woude LH, Post MW. Validity of the mental health subscale of the SF-36 in persons with spinal cord injury. Spinal Cord 2012; 50: 707–710.
- Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry 2003; 57: 113–118.
- Baker A, Barker S, Sampson A, Martin C. Caregiver outcomes and interventions: a systematic scoping review of the traumatic brain injury and spinal cord injury literature. Clin Rehabil 2017; 31: 45–60.
- Fekete C, Tough H, Siegrist J, Brinkhof MW. Health impact of objective burden, subjective burden and positive aspects of caregiving: an observational study among caregivers in Switzerland. BMJ Open 2017; 7: e017369.
- Lindt N, van Berkel J, Mulder BC. Determinants of overburdening among informal carers: a systematic review. BMC Geriatr 2020; 20: 304.
- Swinkels J, Tilburg TV, Verbakel E, Broese van Groenou M. Explaining the gender gap in the caregiving burden of partner caregivers. J Gerontol B Psychol Sci Soc Sci 2019; 74: 309–317.
- Nogueira PC, Nasbine Rabeh SA, Larcher Caliri MH, Spadoti Dantas RA, Haas VJ. Burden of care and its impact on health-related quality of life of caregivers of individuals with spinal cord injury. Rev Lat Am Enfermagem 2012; 20: 1048–1056.
- Khazaeipour Z, Rezaei-Motlagh F, Ahmadipour E, Azarnia-Ghavam M, Mirzababaei A, Salimi N, et al. Burden of care in primary caregivers of individuals with spinal cord injury in Iran: its association with sociodemographic factors. Spinal Cord 2017; 55: 595–600.
- Gerhart K, Johnson R, Whiteneck G. Health and psychosocial issues of individuals with incomplete and resolving spinal cord injuries. Spinal Cord 1992; 30: 282–287.
- Conti A, Clari M, Nolan M, Wallace E, Tommasini M, Mozzone S, et al. The relationship between psychological and physical secondary conditions and family caregiver burden in spinal cord injury: a correlational study. Top Spinal Cord Inj Rehabil 2019; 25: 271–280.
- Biering-Sørensen F, DeVivo M, Charlifue S, Chen Y, New P, Noonan V, et al. International spinal cord injury core data set (version 2.0) – including standardization of reporting. Spinal Cord 2017; 55: 759–764.