
Table I. Demographic and injury details of participants (n = 21)
From the 1Sydney Medical School, University of Sydney, New South Wale and 2Royal Melbourne Hospital, The University of Melbourne, Melbourne, Australia
Objective: To examine the validity of the Comprehensive and Brief International Classification of Functioning, Disability and Health (ICF) Core Sets for Traumatic Brain Injury for patients with traumatic brain injury living in the community in Australia.
Design: Qualitative methodology using focus groups and individual interviews.
Patients: Community-dwelling adult persons with traumatic brain injury.
Methods: Patients sustaining traumatic brain injury with post-traumatic amnesia between September 2009 and August 2013, selected from the Royal Melbourne Hospital Trauma Registry, were invited to participate in the study. Participants were asked structured questions based on the ICF framework. Digital recordings of the discussions were transcribed in full for linking to the ICF categories.
Results: Saturation of data was reached after 5 groups involving 21 participants. Participants identified as relevant 77.7% (n = 108/139) and 100% (n = 23/23) of the Comprehensive and Brief ICF Core Sets for traumatic brain injury, respectively. Additional ICF categories identified in 2 or more groups were: b180 “experience of self and time functions”; b250 “taste function”; b265 “touch function”; b530 “weight maintenance function”; b780 “sensation related to muscles and movement”; and d650 “caring for household objects”.
Conclusion: The study found additional ICF categories to consider and supports the use of the ICF Core Sets for traumatic brain injury in Australian adults in the community.
Key words: brain injury; traumatic; rehabilitation; qualitative research; focus groups; self-report.
Accepted Jul 2, 2021; Epub ahead of print Jul 9, 2021
J Rehabil Med 2021; 53: jrm00218
Correspondence address: Pearl Chung, Sydney Medical School, University of Sydney, New South Wales, Australia. E-mail: Pearl.Chung@Sydney.edu.au
Doi: 10.2340/16501977-2860
Patients with traumatic brain injuries were invited to discuss the problems and barriers they faced after their injuries. Participants were living at home in Victoria, Australia, and provided their responses to the researchers for the “patient perspective”. The discussions were compared with the comprehensive and abbreviated lists of issues (known as the International Classification of Functioning, Disability and Health (ICF) Core Sets for Traumatic Brain Injury). These lists are intended to represent the lived experience of brain injury survivors. Overall, the current lists were found to be adequate for use in similar patient populations. Additional items to consider for the comprehensive list were also identified as potentially relevant. These included sensory or perception problems and difficulties with completing domestic tasks.
Traumatic brain injury (TBI) is a significant cause of death and disability in all age groups. TBI affects approximately 69 million individuals per year worldwide (1). In Australia, the incidence of TBI is estimated to be 99.1–107 per 100,000 person-years (2, 3). Multidisciplinary rehabilitation for TBI optimizes modifiable biopsychosocial factors to improve personal and social functioning through compensatory and remediatory mechanisms. Researchers and clinicians should seek to understand the lived experience of patients with TBI, in order to provide person-centred rehabilitation programmes of relevance to the patient.
Qualitative studies using open-ended questions encourage participants to focus on issues of interest and related concepts considered relevant by the participant. However, these studies are labour intensive and challenging to conduct. Cognitive problems can affect the validity of self-reports in TBI, but research in other diseases affecting cognition, such as Alzheimer’s disease, identified the importance of incorporating patient perspectives in understanding psychological and social contributors to behaviours and effects of treatment (4).
The World Health Organization (WHO) recommends using the International Classification of Functioning, Disability and Health (ICF) to describe physiological, personal and social functioning in disability (5). The ICF uses a nested alphanumeric classification system to present a relational understanding of functioning and disability for ICF components of Body Functions, Body Structures, Activities and Participation, and Environmental Factors (5). For example, a TBI survivor may experience difficulties at work due to problems with multitasking. The disability (d8451 “maintaining a job” in Participation) relates to the activity limitations (d220 “undertaking multiple tasks” in Activities) and the impairments (b164 “higher-level cognitive functions” in Body Functions), which are also related to:
Thus, the ICF framework presents the relationship between the relevant components of disability.
ICF Core Sets are collections of ICF categories of relevance to a health condition or a healthcare context (6). In 2010, the Comprehensive and Brief ICF Core Sets for TBI were developed through an international, multi-stage decision-making and consensus process involving patients, caregivers, health professionals and researchers (7). The Comprehensive ICF Core Set for TBI lists 139 ICF categories for multidisciplinary assessment of TBI, while the Brief ICF Core Set for TBI lists 23 ICF categories for epidemiological studies or clinical encounters (8, 9).
The ICF Core Sets for TBI represents the spectrum of TBI severities and the continuum of care following TBI (7). Validation studies ensure the relevance of ICF Core Sets and identify any missed concepts through focus groups or individual interviews. Validation studies for ICF Core Sets for other health conditions include rheumatoid arthritis, fibromyalgia and stroke (10–13). In TBI, validation studies were conducted in patients with mild TBI in Norway (14), and patients and caregivers for all TBI severities in Italy (15). The objective of the current study is to examine the validity of the ICF Core Sets for TBI for patients with TBI living in the community in Australia.
A qualitative methodology was used to interview persons with TBI through focus groups and individual interviews. The study was approved by the Melbourne Health Research Ethics Committee (HREC 2013.224) in 2013. The study was completed in 2015.
Participants
The Royal Melbourne Hospital (RMH) is a Level 1 trauma centre in Victoria, Australia. The RMH Trauma Registry was searched to identify adult patients who sustained a major trauma (as defined by death; admission to intensive care unit for more than 24 hours requiring a period of mechanical ventilation; injury to 2 or more body systems and Injury Severity Score over 12; or urgent surgery for an intracranial, intrathoracic or intra-abdominal injury, or pelvic or spinal fractures). From the surviving patients with major trauma, patients with a documented period of post-traumatic amnesia (PTA) with TBI, who were admitted between 1 September 2009 and 30 August 2013, were identified. The registry contributes to the state-wide trauma registry according to the Victorian State Trauma Registry Patient inclusion criteria. It was possible to search for PTA in the registry because PTA was a coded complication of trauma. All identified persons were invited by post and provided with a written consent form. From respondents, potential participants were selected using a maximum variation strategy based on age, sex, time since injury, and place of residence for remoteness (16). All participants were contacted by phone before their participation in the study to discuss the nature of the research and to confirm the informed consent. Participants expressing difficulty with attending focus groups at the RMH at Royal Park Campus, due to travel or scheduling reasons, were offered individual interviews in person or via phone. There was no monetary reimbursement for time or travel.
Sample size
Each group consisted of 3–6 participants. Saturation of data was required to determine the sample size (17). Saturation was anticipated at 5 groups, based on a previous validation study using a comparable methodology (11).
Data collection
Pre-injury demographic (age, sex, postcode) and injury details (admission date, cause and mechanism of injury, Glasgow Coma Scores, and injuries sustained), and acute hospitalization data (length of stay, discharge outcomes) were available in the RMH Trauma Registry. All additional pre- and post-injury outcomes were self-reported by the participants. Participants were asked about living arrangements, marital status, educational level, employment status, alcohol and substance use, and psychiatric diagnoses. The information was collected from the participants when confirming consent by phone before the focus group to ensure confidentiality.
All focus groups were conducted by the same moderator (PC), who is a medical doctor with training in qualitative research methodologies and research among vulnerable populations. Accompanying caregivers were asked to wait at another venue. Exceptions were made if it was considered that the participant would feel vulnerable without the caregiver. Caregivers were permitted to observe the session and discouraged from making any comments. All groups began with an introduction in non-technical English language to outline the session. Attendees were asked to maintain confidentiality and to refrain from discussing injury details, in order to minimize psychological distress. Rest breaks were offered. The concept of ICF was introduced with the visual aid of a Microsoft PowerPoint 2010 presentation. The ICF-based approach was used for open-ended questions (11). The moderator verbally presented the questions in sequence for all ICF chapters covered by the Comprehensive ICF Core Set for TBI. The wording of the questions was replicated from previous validation studies (11, 12).
[Body Functions] If you think about the {insert chapter heading) of your body and mind, what does not work the way it is supposed to?
◦ What do you find helpful or supportive?
◦ What barriers do you experience?
At the end, the moderator summarized the discussion and presented the Comprehensive ICF Core Set for TBI to the participants. Participants were invited to verify and amend the findings and add comments, as prompted by the presentation of the Comprehensive ICF Core Set for TBI. Individual interviews were conducted at the hospital or on the phone. All procedures for personal interviews were as for the focus groups, with no visual aid for phone interviews.
Focus group discussions and individual interviews were digitally recorded with a Philips LFH0895 Voice Tracer Meeting Recorder, (Philips, Australia) and transcribed verbatim. All potential identifiers (name, age, places, and dates), individual injury descriptions, and comments by the moderator or caregivers were not transcribed with notation made to the effect on the transcript. Personal interviews were pooled into the allocated groups and reordered according to ICF chapter headings at the point of transcription to prevent individual re-identifications. Meaning condensation procedure was applied to divide the data into meaning units, which is a standard process in the validation of ICF Core Sets (11, 12). Each statement containing 1 meaning unit was assigned 1 unique identification number for reference purposes.
Qualitative analysis
The qualitative analysis involved the identification of meaning units for inclusion and exclusion. Meaning units were excluded from ICF linking if the change following TBI was neither problematic nor beneficial from the patient perspective (e.g. “I made new friends after losing my old friends”)b. Some meaning units could not be linked to an ICF category because they referred to Personal Factors or because the concepts not covered or not defined within the ICF. Meaning units were also excluded from ICF linking if other injuries or pre-existing health conditions caused a problem. Unclear statements (e.g. “I have that problem too”, “I can’t do that”, “My friends thinks I’m okay”) were also excludeda.
aThese are hypothetical examples and are not the actual words of the participants in the study.
Linking to ICF
Each concept was linked to the most precise ICF category according to the linking rules using all levels of ICF classifications (18, 19). ICF designations for personal factors (“pf”); not definable concepts (“nd”); and not covered concepts (“nc”) were not used in the linking, for practicability.
Confirmation of the ICF Core Sets for traumatic brain injury
From the ICF linking process, all ICF categories were simplified to the respective 2-level ICF classification for comparison with the ICF Core Sets for TBI, which use 2-level ICF classification (except for 1 item in the Brief ICF Core Set for TBI). Also, ICF categories within d5 “self-care” were converted to a 1-level ICF classification for matching with the Brief ICF Core Set for TBI, which uses d5 “self-care” to represent all self-care related concepts. An ICF category was confirmed as relevant if it was identified in 1 or more focus groups. Given the broad spectrum of problems in TBI, it was hypothesized that 70% or more (i.e. 98 or more of the 139 categories) of the Comprehensive ICF Core Set for TBI and 100% (23 of the 23 categories) of the Brief ICF Core Set for TBI would be confirmed by the focus groups.
Saturation of data
Saturation of data was defined as the point at which the number of new categories identified by an additional focus group was less than 5% of the cumulative number of ICF categories identified from the Comprehensive ICF Core Set for TBI.
Additional ICF categories
New ICF categories at 2-level classification were presented as additional categories if these were identified in 2 or more groups and were not included in the Comprehensive ICF Core Set for TBI.
Peer-review of ICF linking
Peer-review involved reviewing the text analysis and independent ICF linking of a sample of transcribed data. From the full transcription, 15% of meaning units were randomly selected by their unique identification number using the Microsoft Excel 2010’s random number generator. The meaning units were linked to a 2-level classification in the ICF through the independent peer-review process by FK or BA for agreement with the ICF linking by PC. Kappa statistic for agreement was calculated using IBM SPSS v23 (IBM SPSS Statistics, Armonk, NY).
Participants
A total of 21 patients were included for participation. Potential participants who responded after the study reached saturation were excluded from the study. The study was conducted in 3 focus groups (n = 14) and 2 pooled-analyses of interviews (n = 7) to maximize variation within the groups (Table I). The focus group discussions lasted 69–83 min (mean 76 min), and individual interviews lasted 18–47 min (mean 33 min).

Table I. Demographic and injury details of participants (n = 21)
Data collection
The median age of participants was 59 years at injury (interquartile range (IQR) 47–66 years) and 76% of participants were male (n = 16) (Table I). All categories of rurality, education levels and pre-injury health status were represented by the participants. The majority of injuries were sustained in transport accidents (n = 11) and fall from heights (n = 8), with 38% of the injuries being compensable. All categories of TBI severities using GCS were represented in the study, including 29% with severe TBI, 24% with moderate TBI and 67% with a mild TBI. Participants had an acute hospital length of stay of 14 days (median, IQR 9–18 days) before being discharged to another health facility (n = 13) or home (n = 8). At the time of the study, participants were 2.6 years from injury (median IQR 1.9–4.0 years). All participants were living in the community in private residences, including 4 participants who lived alone. Eighteen participants were working at the time of the injury. Over half of the participants reported a change in occupational status due to the injury. Participants worked reduced hours (n = 3) or did not return to work (n = 9). A diagnosis of depression or anxiety was reported by 10 (48%) of the study participants, including 6 participants who were diagnosed with depression or anxiety following the TBI.
Qualitative analysis and linking to ICF
The qualitative analysis found 1,142 meaning units. From these, 810 meaningful concepts were linked to ICF categories, with 92–236 ICF categories identified per group. After accounting for repeated ICF categories, the study identified a total of 217 unique ICF categories (Table II). These were in Body Functions (n = 88); Body Structures (n = 5); Activities and Participation (n = 70); and Environmental Factors (n = 54). Most frequently linked categories were: b144 “memory functions” (n = 33); b126 “temperament and personality functions” (n = 23); b134 “sleep functions” (n = 21); e115 “products and technology for personal use in daily living” (n = 21); e310 “immediate family” (n = 18); b164 “higher-level cognitive functions” (n = 17); and b280 “sensation of pain” (n = 16).

Table II. Identified International Classification of Functioning, Disability and Health (ICF) categories by ICF components
Saturation of data
The saturation of data was reached at 5 groups (Fig. 1), with the fifth group contributing an additional 4 (3.8%) ICF categories from the Comprehensive ICF Core Set for TBI.

Fig. 1. Saturation of data for the Comprehensive International Classification of Functioning, Disability and Health (ICF) Core Set for traumatic brain injury (TBI).
Confirmation of the ICF Core Sets for traumatic brain injury
A total of 108 of the 139 (77.7%) ICF categories of the Comprehensive ICF Core Set for TBI and all 23 categories (100%) of the Brief ICF Core Set for TBI were identified in the study (Table II). The coverage of the Comprehensive ICF Core Set for TBI in the study were 70.5% for Activities and Participation; 76.9% for Environmental Factors; 89.2% for Body Functions; and 100% in Body Structures. The full lists of items covered are presented according to the ICF components in Tables III–V. Eleven ICF categories were identified as relevant in all 5 groups in the study. Eight of these, which were included in the Brief ICF Core Set for TBI, were: b152 “emotional functions”; b280 “sensation of pain”; d350 “conversation”; d450 “walking”; d845 “acquiring, keeping and terminating a job”; d920 “recreation and leisure”; e115 “products and technology for personal use in daily living”; and e120 “products and technology for personal indoor and outdoor mobility and transportation”. Three ICF categories identified by all focus groups, but not included in the Brief ICF Core Set for TBI, were: b126 “temperament and personality functions”; b134 “sleep functions”; and d240 “handling stress and other psychological demands”.

Table III. Coverage of the International Classification of Functioning, Disability and Health (ICF) Core Sets for traumatic brain injury (TBI) for Body Functions and Structures
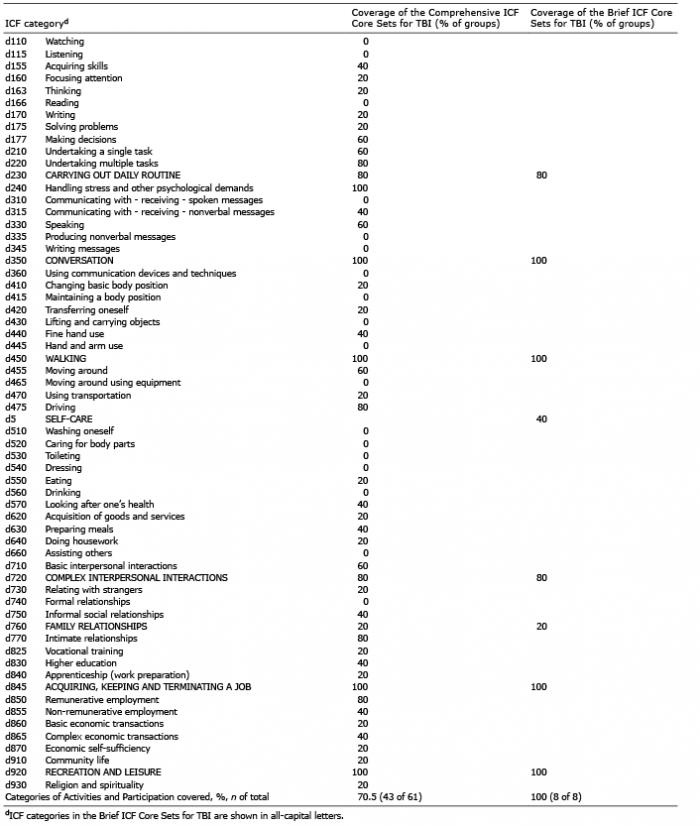
Table IV. Coverage of the International Classification of Functioning, Disability and Health (ICF) Core Sets for traumatic brain injury (TBI) for Activities and Participation

Table V. Coverage of the International Classification of Functioning, Disability and Health (ICF) Core Sets for traumatic brain injury (TBI) for Environmental Factors
Additional ICF categories
The overall coverage of issues experienced by the focus groups using the Comprehensive ICF Core Set for TBI was 49.8%, with 37.5% in Body Functions; 40% in Body Structures; 61.4% in Activities and Participation; and 55.6% in Environmental Factors (Table II). From the concepts not covered in the Comprehensive ICF Core Set for TBI, 6 2-level ICF categories were identified by 2 or more groups, but were missing in the Comprehensive ICF Core Set for TBI. These were: b180 “experience of self and time functions”; b250 “taste function”; b265 “touch function”; b530 “weight maintenance function”; b780 “sensation related to muscles and movement”; and d650 “caring for household objects” (Table VI). In ICF, b780 “sensation related to muscles and movement” refers to muscle stiffness, spasms and involuntary contractions, which is separate from b260 “’proprioceptive’ function”.
Peer review of ICF linking
A total of 173 meaning units underwent peer- review (15.1%). ICF linking at 2-level classification resulted in a Cohen’s kappa statistic of 0.602 for agreement and a chance agreement of 0.00276, which suggests moderate inter-rater agreement (20).

Table VI. Additional International Classification of Functioning, Disability and Health (ICF) categories identified in 2 or more groups
This is the first study in the validation of the ICF Core Sets for TBI in Australia. The study found that Australian community-dwelling persons with TBI identified 77.7% and 100% of the categories of the Comprehensive and Brief ICF Core Sets for TBI, respectively, as relevant to their experience.
The study participants discussed a broad range of issues affecting their lives following TBI, with 810 meaningful concepts linked to 217 unique ICF categories. The breadth of the concepts identified in this study exceeded previous studies, which identified 108 ICF categories in patients with mild TBI (n = 17) (14); 144 ICF categories in patients with all TBI severities (n = 41) (15); and 129 ICF categories in caregivers of patients with all TBI severities (n = 41) (15).
The study identified additional concepts of potential relevance to TBI survivors not included in the ICF Core Sets for TBI. Some of the missed concepts in the Comprehensive ICF Core Set for TBI were subjective problems or experiences. Missed concepts included sensory functions of taste, touch and muscle stiffness or spasms. Altered or distorted taste functions usually accompany impaired smell functions (b255 “smell function” in the Comprehensive ICF Core Set for TBI), but gustatory disorder following TBI is often a separate phenomenon in patients (21). From the patient’s perspective, the distorted taste is a different challenge to anosmia. It can exacerbate problems with cooking and appetite and result in unintentional weight gain or excessive consumption of alcohol or salt. Altered touch sensation and muscle stiffness are known issues in TBI, but it is difficult to assess, quantify and treat the patients’ subjective symptoms. These symptoms probably differ from pain or spasms with spasticity and dystonia. There may be additional subjective and quality of life benefits in ensuring that clinicians acknowledge and optimize the care of sensory problems following TBI. Participants also described their experience of adjusting to living through a period of amnesia, where there were gaps in memories lasting for weeks to months at times. The concept of b180 “experience of self and time functions” is expected to affect all persons emerging from PTA. There may be a role for dedicated psychological interventions to help patients adjust to this experience. There were 3 ICF categories that were not included in the Brief ICF Core Set for TBI, but were identified as relevant in all 5 groups. These were b126 “temperament and personality functions”; b134 “sleep functions”; and d240 “handling stress and other psychological demands”. These are, again, subjective issues with unclear aetiology and treatment options from the clinicians’ perspectives.
Some categories within the Comprehensive ICF Core Sets for TBI were not identified as relevant in this study. Some issues may not be reported in persons with mild to moderate injuries. For example, d166 “reading” and d310 “communicating with – receiving – spoken messages” could be difficult following mild TBI with post-concussive symptoms, but d110 “watching” and d115 “listening” may not be reported as a problem. Other problems are time-limited issues in TBI recovery and resolve with time, except in catastrophic injuries or injuries with focal ischaemia or haemorrhage, including d445 “hand and arm use”, d510 “washing oneself” and d560 “drinking”. Finally, patients may not be aware of specific problems in their experience or due to decreased awareness; for example, with b555 “endocrine functions” or d335 “producing nonverbal messages”, respectively.
Most categories in the Environmental Factors of the Comprehensive ICF Core Set for TBI were identified as relevant (76.9%). Participants in the study experienced significant changes to their physical, social and attitudinal environment, especially with occupational and social roles. However, many of the changes were not described as a facilitator of, or a barrier to, functioning from the patient’s perspective, but merely as a change. The reason for this is not clear, but it is possible that participants’ perceptions changed or adapted with time as a part of an acceptance process. The study also provided insight into the complex nature of family interactions, as participants recognized the importance of the immediate family for decreasing disability (e310 “ immediate family” – facilitator in 80%, barrier in 20%), but the attitudes of the immediate family were often perceived to be a barrier to functioning (e410 “individual attitudes of immediate family members” – barrier in 60%). This highlights the importance of addressing the physical and attitudinal environment of a TBI survivor as separate issues. Multidisciplinary rehabilitation in persons with TBI often requires a family member’s involvement as a caregiver for safety and social functioning (22). Additional care and support are encouraged for TBI survivors’ family members, recognizing that adjustment can be challenging for the patient and families, with altered relationships and social roles due to supervision needs, emotional difficulties, and work capacity loss.
Study limitations
The study was limited in the range of complexities and adverse outcomes of TBI because participants responding to the invitation lived in the community, had access to the same residential address, were able to consent, and communicated verbally. The data collection may have been affected by some participants not having access to the visual presentation and being interviewed individually. Participants of this study were selected from Victoria, with limited generalisability to other states and territories of Australia. Using PTA as selection criteria likely resulted in excluding persons with extremely severe injuries (where PTA testing may not have commenced during the acute trauma admission). Major trauma definition may have excluded persons with isolated mild TBIs.
Conclusion
This study provided patient perspectives for the validation of the ICF Core Sets for TBI in the Australian community-dwelling persons with TBI with a period of PTA, and included all severities of TBI. This study supports the use of the ICF Core Sets for TBI in comparable populations. Additional ICF categories were identified as relevant and could be included in research in comparable populations.
This paper was submitted by Dr Pearl Chung for completion of a PhD (Section III, Chapter 10) (23) and presented as a poster at the International Brain Injury Association Eleventh World Congress on Brain Injury (24). The authors thank the study participants; the Royal Melbourne Hospital Trauma Registry; Dr Bhasker Amatya for assistance with the data analysis; and Associate Professors Ian Baguley, Associate Professor Louisa Ng and Dr Clayton King for feedback.
The authors have no conflicts of interest to declare.