ORIGINAL REPORT
COMPARISON OF OUTCOMES OF TWO DIFFERENT CORTICOSTEROID INJECTION APPROACHES FOR PRIMARY FROZEN SHOULDER: A RANDOMIZED CONTROLLED STUDY
Zhibo DENG, MM1#, Zhi LI, MM1#, Xiangwei LI, MM1, Zhongqiu CHEN, MM2, Chen SHEN, MM1, Xianding SUN, MD, PhD1, Han SHU, MD1, Jiangping WU, MM1 and Kaiying TANG, MD1
From the 1Center for Joint Surgery, Department of Orthopedic Surgery, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China, 2Department of Information Center, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China
#These authors contributed equally to this work.
Objective: Corticosteroid injection is a common treatment for primary frozen shoulder, but controversy remains regarding whether different injection approaches to the glenohumeral joint have similar clinical benefits.
Design: Randomized controlled clinical trial.
Patients: A total of 60 patients with primary frozen shoulder were divided randomly into either anterior or posterior approach groups.
Methods: Both groups received a 5-mL drug injection, including 1 mL 40 mg/mL triamcinolone acetonide and 4 mL 2% lidocaine. Follow-up time-points were 4, 8 and 12 weeks post-injection. Outcome measures included visual analogue scale score, Constant-Murley score, and passive range of motion of the shoulder joint.
Results: All outcome measures improved over the follow-up period compared with those of previous follow-up time-points within the groups. The primary finding was that the visual analogue scale score in the anterior group was better than that in the posterior group at each follow-up time-point (all p < 0.05). In addition, improvement in function score and external rotation was faster and significant in the anterior group in the early stages (p = 0.02).
Conclusion: The anterior approach achieves more satisfactory results in pain control and offers better recovery of functional activity than posterior approach in the early period for primary frozen shoulder.
LAY ABSTRACT
Although many studies have been published in recent years on corticosteroid injection in the glenohumeral joint for primary frozen shoulder, the injection approaches described by current reports are not consistent and not described in detail, which is not conducive for their use to be repeated by clinicians. Meanwhile, controversy remains regarding whether different approaches have similar clinical outcomes. This study used a modified anterior approach based on anatomical landmarks, taking the acromioclavicular joint as a reference, to accurately and quickly complete the injection process. The study showed that the anterior approach could reduce pain severity more significantly than the regular posterior approach, and this advantage can be maintained for 3 months. Meanwhile, the function score of the anterior approach could recover to the maximum more quickly. In addition, recovery of external rotation in the anterior approach was faster and greater that for the posterior approach.
Key words: frozen shoulder; adhesive capsulitis; anterior approach; posterior approach; corticosteroid injection.
Citation: J Rehabil Med 2023; 55: jrm00361. DOI: https://doi.org/10.2340/jrm.v55.2201.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Nov 8, 2022; Published: Jan 3, 2023
Correspondence address: Kaiying Tang, Center for Joint Surgery, Department of Orthopedics, The Second Affiliated Hospital of Chongqing Medical University, Linjiang Road No.76, Yuzhong District, Chongqing 400010, China. E-mail: 304248@hospital.cqmu.edu.cn
Competing interests and funding: The authors have no conflicts of interest to declare.
Primary frozen shoulder (PFS), also known as adhesive capsulitis of the shoulder, is a common chronic musculoskeletal disorder with an occult onset and a long disease course (1). The incidence rate is approximately 2–5% among the general population (2). Diabetes and autoimmune diseases also contribute to its occurrence (3). The main symptoms of frozen shoulder are shoulder pain and limitation of shoulder activity (4), which seriously affect the patient’s daily life and work (5).
Owing to the severe restriction of the diseased shoulder’s function, people have used various treatment methods for PFS. Glenohumeral joint corticosteroid injection can not only significantly reduce the pain score (6, 7), but also improve the range of motion (ROM) of the shoulder joint (8). Although the anterior approach (AA) and posterior approach (PA) are both simple and common puncture routes for glenohumeral joint injection, the optimal injection approach remains controversial. The PA is further from the patient’s vison, with more humanization, and is thus more widely used in clinical practice (9). In 2011, Tobola et al. (10) found that the accuracy of contrast medium injection also differs between 3 different approaches: the AA (64.7%), PA (45.7%) and supraclavicular approach (45.5%). Meanwhile, the accuracy of the glenohumeral joint injections did not depend on the experience level of the operator. This observation is in contrast to the findings of Mattie et al. (11), that the accuracy of glenohumeral injections is dependent on the skills and level of experience of the provider. Different accuracies will cause the mixed drugs to not diffuse evenly throughout the entire articular capsule surface, which will yield different therapeutic effects. In 2020, Elnady et al. (12) proposed that, for frozen shoulders, ultrasound-guided hydrodilatation through the AA is practically and functionally more effective than the traditional PA. In 2021, Rijs et al. (13) also proved in a prospective trial that, after injecting contrast agent into the glenohumeral joint through the AA and PA without ultrasound guidance, the accuracy of the AA was higher than that of the PA. However, there have been no prospective clinical studies comparing the clinical effects of the AA and PA (13).
No differences in pain or functional results are apparent between landmark-based and ultrasound-guided corticosteroid injections for the treatment of PFS, however, operation with ultrasound guidance is often costly and time-consuming (14). Therefore, glenohumeral joint corticosteroid injection based on anatomical landmarks has gradually become mainstream. In order to explore the best injection approach, the current study aimed to determine whether the anatomically landmarked AA for glenohumeral joint corticosteroid injection is superior to the PA for patients with PFS.
METHODS
Study type
This was a prospective randomized controlled trial (RCT), conducted in accordance with the principles of the Declaration of Helsinki. All participants signed an informed consent form before participation and voluntarily accepted random grouping. The study was approved by the ethics committee and was registered with the Clinical Trial Registration Center (ChiCTR) (registration number: ChiCTR2100048130) before the start of the trial. The trial lasted approximately 3 months. The study flow chart is shown in Fig. 1.
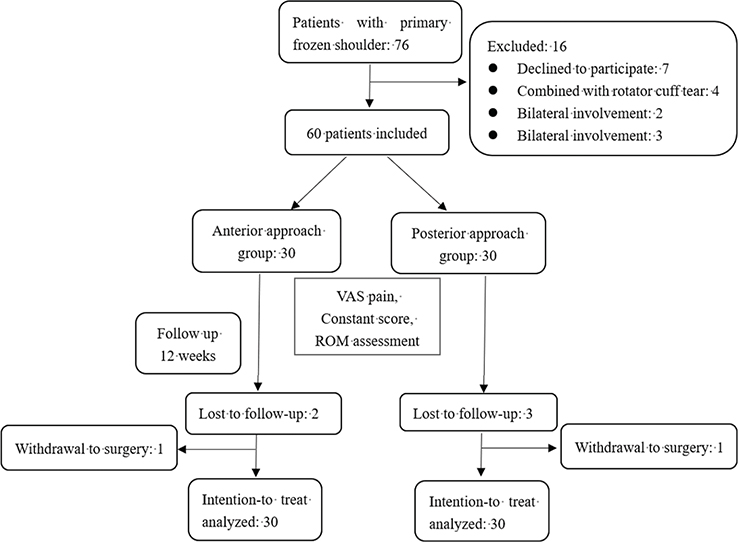
Fig. 1. Flow chart of patient randomization and follow-up. VAS: visual analogue scale; ROM: range of motion.
Patient inclusion criteria
Patients with unilateral PFS treated at our hospital (Department of Orthopedics, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China) from 31 July 2020 to 31 July 2021 were considered for inclusion.
Inclusion criteria were: (i) age ≥ 18 years with unilateral shoulder pain and limited movement diagnosed with PFS; (ii) duration of pain ≤ 9 months and visual analogue scale (VAS) score ≥ 3 (out of 10); (iii) limitation of movement, i.e. active and passive movement of the affected shoulder joint limited by more than 30° relative to the contralateral shoulder joint in at least 2 directions(abduction, flexion, external rotation, and internal rotation); and (iv) routine shoulder X-ray and/or magnetic resonance imaging (MRI) examinations to exclude other pathologies, such as rotator cuff tears, rotator cuff tendinosis, biceps tendinitis, calcified tendinitis, labial lesion and osteoarthritis.
Exclusion criteria were: (i) shoulder pain secondary to rheumatic disease, trauma, or infectious arthritis; (ii) injection of corticosteroids on the affected side in the past 3 months; (iii) any contraindications associated with steroid injections (e.g. poor glycaemic control and accompanying infectious diseases); and (iv) inability to understand and cooperate with the investigators or provide informed consent.
Sample size estimation
Before randomization, prospective power analysis was used to estimate the sample size. The main results were VAS scores. The assumptions regarding the values and variances of the VAS scores are based on a previous study on frozen shoulder by Buchbinder et al. (15). Assuming a 90% test efficiency between the 2 groups (β = 0.10, α = 0.05), the mean difference was 2 points (minimal clinically important difference of VAS in shoulder pain (16)), and the standard deviation was 2 points. Our test efficacy analysis showed that at least 22 patients in each group were required to obtain significant differences in the VAS score. Assuming a dropout rate of 20%, at least 28 participants in each group were required.
Randomization method
First, a data expert used a computer to generate a column of random numbers, which were divided into 2 groups from the middle. The first group represented the AA group, and the second group represented the PA group. Patients were included in the first or second group in an orderly manner. The assignment was performed by another independent researcher who knew nothing about the details of the treatment. The operator only performed the injection therapy and did not participate in the follow-up and data analysis stages. Follow-up measurements and data analysis were performed by other researchers.
Treatment process
All patients were locally injected by a trained joint surgeon (KT) with a 22 gauge 6-cm long needle to exclude the differences caused by different operators. The volumes of all mixed liquids were 5 mL, including 1 mL 40 mg/mL triamcinolone acetonide + 4 mL 2% lidocaine. After the injection, the same rehabilitation manual (17) (Appendix S1) was issued to guide patients in performing shoulder joint functional exercise. The self-exercise programme was composed of flexion, abduction, external rotation and internal rotation under mild active training, and each exercise was performed 15–20 times during a period of 15 min 3 times a day. The programme lasted for 12 weeks, and patients were excluded if the exercise was not strictly performed during follow-up. In addition, any extra drugs or physiotherapy were prohibited. The detailed injection steps are as follows:
Anterior approach group. As described by Rijs et al. (13), the patient was placed in the sitting position, the upper limb was placed on the thigh on the same side and rotated outward as much as possible, and the elbow joint was placed in the flexion position. The in vitro anatomical landmarks of the shoulder joint were touched in order, and the coracoid process, the inner and outer edges of the acromion, the anterolateral angle of the acromion, the spine of the scapula and the acromioclavicular joint were marked with a pen. After routine disinfection with povidone iodine, the needle was inserted in the soft point between the coracoid process and the anterolateral angle of the acromion, approximately 1 cm below the acromioclavicular joint and 0.5 cm outside the plane of the acromioclavicular joint space (Fig. 2A). Simultaneously, the needle was tilted downward at 30° to the horizontal plane and inward at approximately 10° to the sagittal position. When the needle struck the humeral head, it was tilted inward slightly, and the mixed liquid was then injected with little resistance.
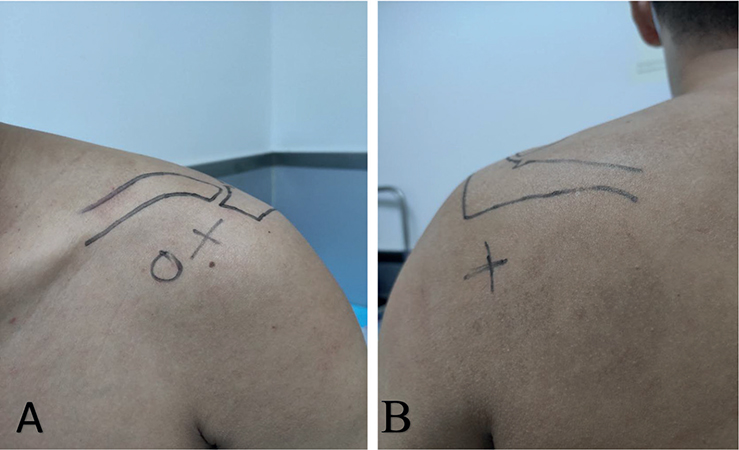
Fig. 2. (A, B) Photographs of anterior approach and posterior approach with the anatomical landmark. Black dot: coracoid process. Black cross indicates the target point of the needle in the injection approach.
Posterior approach group. The patient was placed in the sitting position, and the forearm was placed on the opposite shoulder to fully open the shoulder joint. The in vitro anatomical marks of the shoulder joint were touched in sequence, and the coracoid process, the inner and outer edges of the acromion and the posterolateral angle of the acromion, namely, the spine of the scapula, were marked with a pen. The soft point was 2–3 cm inferior and medial to the posterolateral angle of the acromion (Fig. 2B). After routine skin disinfection, the needle was inserted toward the coracoid process. When there was no effusion during withdrawal, the mixed drug could be injected.
All participants had to stay in the hospital outpatient room for at least 20 min to detect and record any acute adverse reactions after injection, including dizziness, skin flushing and local bleeding. Late adverse events, including menstrual disorder, infection, personality change, and skin pigmentation, were also examined during follow-up.
Outcome measures
The results were collected before treatment and at the 4th, 8th and 12th weeks after injection. Pain severity by VAS and Constant-Murley shoulder score (Constant score) were the primary outcome measures. Secondary outcomes included passive range of motion (ROM) and complications. The detailed scoring rules are as follows: VAS scores range from 0 to 10, with 0 being “painless” and 10 being “the worst pain imaginable”. The Constant score, as the scoring system of the European Shoulder Association, is one of the most widely used shoulder function scores in the world. Out of 100 points, the objective evaluation indices included shoulder ROM and muscle strength (65 points), and the subjective evaluation indices included pain and functional activity (35 points). Higher scores indicate better functional outcomes. Measurement of ROM included passive abduction, flexion, external rotation, and internal rotation of the affected shoulder joint. Each direction was measured 3 times with a goniometer, in a standing position, and the mean value was taken for statistical analysis.
Data analysis
SPSS 25.0 (IBM Corp, Chicago, IL, USA) was used for statistical analysis. Quantitative data are expressed as the mean ± standard deviation (x ± SD), and qualitative data are expressed as percentages. Repeated-measures analysis of variance (ANOVA) was performed to define the overall effect of the measurements at different time-points within the group. The normality of the data was tested by the Kolmogorov–Smirnov test. If normality was rejected, the non-parametric test was used. The differences in continuous variables between the 2 groups were analysed using the independent sample t-test or the Mann–Whitney U test (for non-parametric date), and the dichotomous variables between the 2 groups were analysed using the χ2 test. p < 0.05 was considered statistically significant, with no adjustment for multiple comparisons. To reduce the impact of bias, intention-to-treat (ITT) was used to analyse the follow-up data.
RESULTS
A total of 76 patients with PFS met the inclusion criteria, but 60 patients ultimately signed informed consent forms and were willing to receive randomized treatment. There were 30 patients in the AA group and 30 in the PA group. No significant differences were found in baseline demographic and clinical characteristics between the 2 groups (Table I). Among the 60 patients, 5 were lost to follow-up (3 due to occupational mobility and 2 due to COVID-19). In addition, 2 patients chose surgical treatment due to dissatisfaction with the effectiveness of the treatment. Ultimately, 27 patients in the AA group and 26 patients in the PA group completed all follow-ups (Fig. 1). Moreover, there was no significant difference between the 2 groups in any of the baseline assessments, including the VAS pain score, Constant score and joint ROM (abduction, flexion, external rotation and internal rotation) (p ≥ 0.05) (Table II).
Pain
The results showed improvement in the VAS scores in both groups at follow-up after injection compared with baseline measurements. There was a significant difference between groups (p = 0.000). In addition, the VAS scores in the AA group at 4 weeks (3.15 ± 1.06 vs 4.30 ± 1.84), 8 weeks (2.63 ± 0.85 vs 4.03 ± 1.50) and 12 weeks (1.97 ± 1.13 vs 3.13 ± 1.59) were significantly lower than those in the PA group (all p < 0.05) (Table II).
Functional outcomes
The results showed that the Constant scores after injection improved in both groups compared with the scores recorded in the pretreatment period. A significant difference was also noted between groups (p = 0.000). The Constant scores in the AA group were significantly higher at 4 weeks (65.67 ± 9.67 vs 56.13 ± 9.93) and 8 weeks (72.1 ± 9.9 vs 65.9 ± 10.3) (p < 0.001 and p = 0.02, respectively) (Table II).
Range of motion
All ROM parameters increased over time, and the pre-treatment-to-post-treatment improvement in ROM was statistically significant in both groups. Between-group improvement was also significant (all p < 0.01). In addition, external rotation function in the AA group was significantly better than that in the PA group at 4 weeks (51.1 ± 14.7 vs 43.5 ± 10.0, p = 0.02). There was no significant difference in flexion, abduction or internal rotation function between the 2 groups at any follow-up time-point (Table II).
Complications
One patient in the AA group was sweating and became flustered during the injection process, but recovered after the injection was stopped. These effects were considered to be caused by needle syncope. No other complications were observed in either group.
DISCUSSION
To the best of our knowledge, this is the first prospective RCT to compare anterior and posterior injections of corticosteroids in patients with PFS. The study showed that glenohumeral joint corticosteroid injection from both the AA and PA can remarkably relieve the symptoms of patients with PFS. However, compared with the PA, the AA reduced the VAS score more effectively, and this advantage lasted for 3 months. Furthermore, the Constant score in the AA group recovered to the maximum more quickly. In addition, recovery of external rotation in the AA group was achieved more rapidly and with greater effect. The AA injection group showed better clinical efficacy based on safety guarantees. These results enrich the rationale for a strategy of early non-surgical treatment for PFS and promote the development and popularization of non-ultrasound-guided shoulder intraarticular injections.
The pathophysiology of PFS is initial inflammation, especially around the joint capsule, coracohumeral ligament (CHL) and rotator interval (RI), followed by adhesion and fibrosis of the synovium (18). Considering the unique progression of PFS and the anti-inflammatory effects of corticosteroids, early glenohumeral joint corticosteroid injection has been proven to have an outstanding effect on relieving symptoms (19, 20).
Although many studies have emerged in recent years on corticosteroid injection in the glenohumeral joint for PFS (14, 21, 22), the injection approaches described by current reports are not consistent or described in detail, which is not conducive for their use to be repeated by clinicians. Ultrasound-guided injections are widely used in patients with shoulder conditions to improve accuracy (14, 23). However, an RCT in 2021 (14) revealed that there was no significant difference in the clinical outcome between the anatomical landmark group and the ultrasound-guided group. Combined with the cost of time and money due to ultrasound-guided injection, it remains controversial whether ultrasound-guided technology is worth recommending (24, 25). The current study used a modified AA for injection without ultrasound guidance, which has been proven to have the same accuracy for the glenohumeral joint as the standard PA (13). Using the acromioclavicular joint as a reference, this approach can accurately and quickly complete the injection process.
The AA and PA are common blind injection routes and have been researched in recent years to explore a relatively better route (9). Esenyel et al. (26) found that high accuracy can be obtained without ultrasound-guided injection for glenohumeral joint injection. In a cadaver study, researchers (27) confirmed that the accuracy of anterior injection into the glenohumeral joint was low (only 26.8%) and most of the liquid was injected into the deltoid muscle. However, Sethi et al. (28) showed through cadaveric research that the accuracy of the AA is higher than that of the PA. During shoulder arthroscopic surgery, Kraeutler et al. (29) verified that the accuracy of the AA was as high as 93.3%. Due to above controversy, there are still few studies on the difference in clinical efficacy between the AA and PA. Therefore, the aim of the current RCT was to provide a theoretical basis for this dispute.
Our conclusions agree with those of Elnady et al. (12), identifying the AA as the better choice. More importantly, it is worth noting that, even though the PA has a higher accuracy (27), it may not be necessary for better clinical efficacy. Hall et al. (30) have shown that, even after successful extraction of synovial fluid from the glenohumeral joint, nearly half of the injections were injected outside the joint, but it was unexpected that patients with extra-articular injection experienced similar treatment effects as intra-articular injection. Based on the current clinical study and another study, accurate placement of the injection needle in the glenohumeral joint may not be a prerequisite for enhanced clinical results (14). Ogul et al. (31) demonstrated that more contrast medium leakage was found when the injection was performed through the AA near the RI. Our injection approach was similar to that in this study, and we presumed that the AA could cause corticosteroid leakage in the RI. The RI is an important lesion site in PFS (32). At the time of injection, regarding both the leakage of the mixed drug in the RI and the penetration of the mixed drug from the anterior joint capsule to the RI, the AA was obviously better. Therefore, the AA can yield better clinical results in terms of the VAS and functional outcomes. Meanwhile, regarding the difference between the results of VAS and ROM in the AA group, we believe that it is also related to the RI. The CHL, the main structure in the RI, plays an important role in the external rotation of the shoulder joint (33). Thickening of the CHL, as one of the lesions in the frozen shoulder, restricts movement of the shoulder joint in all directions, especially internal rotation. Hence, the limitation of external rotation is also a characteristic sign of PFS (34). Although steroid dispersion into the joint cavity resulted in a similar improvement in the flexion, abduction, and internal rotation for both groups, the recovery in external rotation was better in the AA group. With reproducibility and advantages in clinical results, the use of glenohumeral injections by anterior approach with an anatomical landmark in clinical practice should be considered. However, it is worth noting that the experience of the operator is also an important condition that cannot be ignored in the injection process.
However, some potential deficiencies warrant discussion. First, there was no control group that received a placebo injection. A control group would increase the credibility of the trial. Secondly, 1 patient in the AA group became flustered and started sweating during the injection process, but recovered after the injection was stopped. Although there was no significant difference between the 2 groups, it was necessary to explain the process to patients before injection to avoid fear of the needle. Thirdly, due to the lack of minimal clinically important differences in ROM, it is unclear whether there were clinical differences even though there were significant differences in early follow-up results between the 2 groups. Thus, more multicentre prospective large-sample trials are needed in the future to assess the validity and accuracy of these findings. However, the sample size of 60 patients (30 in the AA group and 30 in the PA group) satisfied the power analysis, rendering the results reliable. Moreover, all operations were performed by experienced clinicians to ensure accurate results.
CONCLUSION
The current study revealed that the VAS scores in the AA group were lower than those in the PA group at 4, 8 and 12 weeks (all p < 0.05), and the external rotation ROM in the AA group was significantly better than that in the PA group at 4 weeks (p = 0.02). Glenohumeral joint corticosteroid injection using the AA based on anatomical landmarks has the advantages of a convenient operation, short injection time and better effect and is worth popularizing in clinical practice.
ACKNOWLEDGEMENTS
The authors are accountable for all aspects of this study. The study was conducted in accordance with the Declaration of Helsinki (revised 2013). The study was approved by the ethics committee of the Second Affiliated Hospital of Chongqing Medical University (registration number ChiCTR2100048130). Written informed consent was obtained from the patients.
This study was supported by research grants from the Chongqing Science and Technology Commission and Health Commission project (2021MSXM058).
This is a prospective randomized controlled study (RCT). The original datasets are available from the corresponding author on reasonable request.
REFERENCES
- Ricci M. Adhesive capsulitis: a review for clinicians. Jaapa 2021; 34: 12–14.
- de la Serna D, Navarro-Ledesma S, Alayón F, López E, Pruimboom L. A comprehensive view of frozen shoulder: a mystery syndrome. Front Med (Lausanne) 2021; 8: 66–78.
- Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J 2016; 6: 26–34.
- Cheng X, Zhang Z, Xuanyan G, Li T, Li J, Yin L, et al. Adhesive capsulitis of the shoulder: evaluation with us-arthrography using a sonographic contrast agent. Sci Rep 2017; 7: 45–62.
- Robinson C, Seah K, Chee Y, Hindle P, Murray I. Frozen shoulder. J Bone Joint Surg Br 2012; 94: 1–9.
- Sun Y, Zhang P, Liu S, Li H, Jiang J, Chen S, et al. Intra-articular steroid injection for frozen shoulder: a systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. Am J Sports Med 2017; 45: 2171–2179.
- Challoumas D, Biddle M, McLean M, Millar NL. Comparison of treatments for frozen shoulder: a systematic review and meta-analysis. JAMA Netw Open 2020; 3: 11–38.
- Lee D, Yoon S, Lee M, Kwack K, Rah U. Capsule-preserving hydrodilatation with corticosteroid versus corticosteroid injection alone in refractory adhesive capsulitis of shoulder: a randomized controlled trial. Arch Phys Med Rehabil 2017; 98: 815–821.
- Kim DY, Lee SS, Nomkhondorj O, Cho MG, Lee JJ, Hwang JT, et al. Comparison between anterior and posterior approaches for ultrasound-guided glenohumeral steroid injection in primary adhesive capsulitis: a randomized controlled trial. J Clin Rheumatol 2017; 23: 51–57.
- Tobola A, Cook C, Cassas KJ, Hawkins RJ, Wienke JR, Tolan S, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg 2011; 20: 1147–1154.
- Mattie R, Kennedy DJ. Importance of image guidance in glenohumeral joint injections: comparing rates of needle accuracy based on approach and physician level of training. Am J Phys Med Rehabil 2016; 95: 57–61.
- Elnady B, Rageh E, Hussein M, Abu-Zaid M, Desouky D, Ekhouly T, et al. In shoulder adhesive capsulitis, ultrasound-guided anterior hydrodilatation in rotator interval is more effective than posterior approach: a randomized controlled study. Clin Rheumatol 2020; 39: 3805–3814.
- Rijs Z, de Groot P, Zwitser E, Visser C. Is the anterior injection approach without ultrasound guidance superior to the posterior approach for adhesive capsulitis of the shoulder? a sequential, prospective trial. Clin Orthop Relat Res 2021; 10: 47–58.
- Cho C, Min B, Bae K, Lee K, Kim D. A prospective double-blind randomized trial on ultrasound-guided versus blind intra-articular corticosteroid injections for primary frozen shoulder. Bone Joint J 2021; 103-B(2): 353–359.
- Buchbinder R, Hoving JL, Green S, Hall S, Forbes A, Nash P. Short course prednisolone for adhesive capsulitis (frozen shoulder or stiff painful shoulder): a randomised, double blind, placebo controlled trial. Ann Rheum Dis 2004; 63: 1460–1469.
- Kanto K, Lähdeoja T, Paavola M, Aronen P, Järvinen TLN, Jokihaara J, et al. Minimal important difference and patient acceptable symptom state for pain, Constant-Murley score and Simple Shoulder Test in patients with subacromial pain syndrome. BMC Med Res Methodol 2021; 21: 45–54.
- Lin HH, Huang TF, Ma HL, Liu CL. Body mass index and active range of motion exercise treatment after intra-articular injection in adhesive capsulitis. J Chin Med Assoc 2013; 76: 225–228.
- Hand GC, Athanasou NA, Matthews T, Carr AJ. The pathology of frozen shoulder. J Bone Joint Surg Br 2007; 89: 928–932.
- Yoon SH, Lee HY, Lee HJ, Kwack KS. Optimal dose of intra-articular corticosteroids for adhesive capsulitis: a randomized, triple-blind, placebo-controlled trial. Am J Sports Med 2013; 41: 1133–1139.
- Ranalletta M, Rossi LA, Bongiovanni SL, Tanoira I, Elizondo CM, Maignon GD. Corticosteroid injections accelerate pain relief and recovery of function compared with oral NSAIDs in patients with adhesive capsulitis: a randomized controlled trial. Am J Sports Med 2016; 44: 474–481.
- Oh JH, Oh CH, Choi JA, Kim SH, Kim JH, Yoon JP. Comparison of glenohumeral and subacromial steroid injection in primary frozen shoulder: a prospective, randomized short-term comparison study. J Shoulder Elbow Surg 2011; 20: 1034–1040.
- Hopewell S, Keene DJ, Marian IR, Dritsaki M, Heine P, Cureton L, et al. Progressive exercise compared with best practice advice, with or without corticosteroid injection, for the treatment of patients with rotator cuff disorders (GRASP): a multicentre, pragmatic, 2 × 2 factorial, randomised controlled trial. Lancet 2021; 398: 416–428.
- Prestgaard T, Wormgoor MEA, Haugen S, Harstad H, Mowinckel P, Brox JI. Ultrasound-guided intra-articular and rotator interval corticosteroid injections in adhesive capsulitis of the shoulder: a double-blind, sham-controlled randomized study. Pain 2015; 156: 1683–1691.
- Balazs CGC. In frozen shoulder, US-guided versus blind administration of intra-articular corticosteroid injections increased accuracy of injections but did not improve clinical outcomes at 12 weeks. J Bone Joint Surg Am 2021; 103: 2144–2148.
- Soh E, Li W, Ong KO, Chen W, Bautista D. Image-guided versus blind corticosteroid injections in adults with shoulder pain: a systematic review. BMC Musculoskelet Disord 2011; 12: 137–152.
- Esenyel CZ, Ozturk K, Demirhan M, Sonmez M, Kahraman S, Esenyel M, et al. Accuracy of anterior glenohumeral injections: a cadaver study. Arch Orthop Trauma Surg 2010; 130: 297–300.
- Sethi PM, Kingston S, Elattrache N. Accuracy of anterior intra-articular injection of the glenohumeral joint. Arthroscopy 2005; 21: 77–80.
- Sethi PM, El Attrache N. Accuracy of intra-articular injection of the glenohumeral joint: a cadaveric study. Orthopedics 2006; 29: 149–152.
- Kraeutler MJ, Cohen SB, Ciccotti MG, Dodson CC. Accuracy of intra-articular injections of the glenohumeral joint through an anterior approach: arthroscopic correlation. J Shoulder Elbow Surg 2012; 21: 380–383.
- Hall S, Buchbinder R. Do imaging methods that guide needle placement improve outcome? Ann Rheum Dis 2004; 63: 1007–1008.
- Ogul H, Bayraktutan U, Ozgokce M, Tuncer K, Yuce I, Yalcin A, et al. Ultrasound-guided shoulder MR arthrography: comparison of rotator interval and posterior approach. Clin Imaging 2014; 38: 11–17.
- Mengiardi B, Pfirrmann CW, Gerber C, Hodler J, Zanetti M. Frozen shoulder: MR arthrographic findings. Radiology 2004; 233: 486–492.
- Sun Y, Liu S, Chen S, Chen J. The effect of corticosteroid injection into rotator interval for early frozen shoulder: a randomized controlled trial. Am J Sports Med 2018; 46: 663–670.
- Akkaya H, Söker E, Dilek O, Söker G, Gülek B. Evaluation of magnetic resonance imaging findings in adhesive capsulitis: which quantitative findings are most valuable? Rev Assoc Med Bras (1992) 2021; 67: 1719–1723.