ORIGINAL REPORT
EFFECTS OF VISUAL FEEDBACK DURING BALANCE TRAINING ON KNEE FUNCTION AND BALANCE ABILITY IN POSTOPERATIVE PATIENTS AFTER KNEE FRACTURE: A RANDOMIZED CONTROLLED TRIAL
Tian ZHANG, MD1,2, Bing QIU, MS3, Hong Ju LIU, MD1, Jing XU, MS1, Da Xing XU, MD2, Zhi Yi WANG, MD4 and Wei NIU, MD, PhD2
From the 1Department of Rehabilitation Medicine, Guizhou Orthopedics Hospital, Guiyang, 2Second Clinical College, Guangzhou University of Chinese Medicine, Guangzhou, 3Department of Joint Surgery, Guizhou Orthopedics Hospital and 4Second Affiliated Hospital, Guizhou University of Traditional Chinese Medicine, Guiyang, China
Objective: To investigate the effects of visual feedback training on knee function and balance ability in postoperative patients with knee fracture.
Methods: A clinical randomized controlled trial with 104 participants, randomly assigned (1:1) to a visual feedback training group or a control group. Eligible participants were evaluated using Lysholm scores, the Tinetti scale, and the evaluation module of TecnoBody® to demonstrate dynamic balance function in a standing position before treatment and after 4 and 8 weeks of treatment.
Results: Both visual feedback training and control groups improved significantly in the Lysholm and Tinetti scores after 8 weeks. Compared with the control group, the TecnoBody® tests included centre of pressure path length, and the area over centre of pressure movement, both of which significantly improved in the visual feedback training group at 8 weeks after treatment. There was no difference between the 2 groups in terms of their Lysholm scores and Tinetti gait before the intervention and 4 weeks after treatment.
Conclusion: Applying visual feedback training in conjunction with traditional rehabilitation strategies may improve knee function and motor control in postoperative patients with knee fracture. Although visual feedback training does not have a short-term effect on knee function and gait, this method could be a useful addition for rehabilitation of knee fracture patients.
LAY ABSTRACT
This study used the TecnoBody® (PK-254P, Bergamo, Italy) to evaluate balance in the standing position of all participants. This equipment provides data on the centre of pressure path length and the area over which the centre of pressure moves. The Lysholm score was used to assess knee function, and the Tinetti scale to assess motor control. Applying visual feedback training in conjunction with traditional rehabilitation strategies could decrease postural sway and increase motor control in postoperative patients with knee fracture, as well as subsequently improve knee function and balance ability. There were no adverse effects due to the combined rehabilitation programme.
Key words: visual feedback training; knee function; balance ability; motor control; postoperative patients with knee fracture.
Citation: J Rehabil Med 2022; 54: jrm00281. DOI: http://dx.doi.org/10.2340/jrm.v54.2209.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Feb 21, 2022; Epub ahead of print: March 24, 2022; Published: May 11, 2022
Correspondence address: Tian Zhang, Second Clinical College, Guangzhou University of Chinese Medicine, Airport Road 12, Baiyun District, Guangzhou, Guangdong and Hong Ju Liu, Department of rehabilitation medicine, Guizhou Orthopedics hospital, Guiyang, China. E-mails: zhangtian12002@aliyun.com, 296115887@qq.com
Competing interests and funding: The authors have no conflicts of interest to declare.
The knee joint is the most complex trochlear joint. When injured, the knee joint may sustain compound injuries, such as meniscus injury, synovium injury, cruciate ligament, and collateral ligament injury. A high demand for orthopaedic surgery can lead to a lack of attention to proper rehabilitation of postoperative fracture patients. A lack of effective knee proprioception training and balance ability training may result in instability of the knee joint, thereby subjecting patients to potential re-injury during standing and walking (1). Therefore, administration of rehabilitation after knee surgery is important and necessary.
Balance plays an important role in function, as it allows individuals to maintain posture and respond to perturbations; it encompasses balance control when movement is present and is a key aspect of overall balancing ability (2). One strategy for balance training is for participants to stand on a force platform while providing continuous visual feedback on the centre of pressure (COP), while instructing them to minimize movement of the COP during quiet standing (3). The overall principle of such visual feedback training (VFT) is to collect data on the force and direction of a patient’s lower limbs on the balance plate, monitor the position of the plantar COP, tilt angle, and movement trajectory, and then provide visual feedback via the computer screen (4). Thus, patients undertake balance training during the rehabilitation period using real-time feedback, in the form of moving images on the computer screen corresponding to changes in tilt angle and plantar COP (5). Previous studies have shown that provision of visual feedback regarding COP displacement can enhance the ability of synchronous activities in the peripheral neuromuscular system, and may subsequently improve the dynamic stability of the body (6). In addition, a rehabilitative plan based on balance training can significantly enhance proprioceptive sensation and function of the knee joint. A meta-analysis confirmed that strengthening proprioceptive training could significantly reduce the incidence of knee joint re-injury, by reducing inhibition and increasing stimulation of the proprioceptors (7). However, most studies focus on post-stroke patients, and data on VFT in aiding balance training during knee joint rehabilitation is lacking. Hence, there is a need for research into the clinical application of VFT in lower extremity injuries.
In routine training, patients usually assess their standing balance state subjectively through their own sensations and the guidance of therapists. The addition of VFT can compensate for the loss of proprioception after injury, and can significantly improve the effect of rehabilitation (8). Therefore, 30 min of VFT was added to our rehabilitation programme for postoperative patients with knee fracture, using the TecnoBody® system (PK-254P, Bergamo, Italy) to perform VFT and determine changes in knee function, motor control, and balance ability.
MATERIAL AND METHODS
Participants
Individuals were screened and recruited from the resident patient and outpatient department of rehabilitation at Guizhou Orthopedics Hospital, China, between July 2018 and June 2019. A total of 127 patients who had undergone surgery for knee fracture were admitted to the rehabilitation ward and screened. Among them, 12 did not meet the study inclusion criteria and were excluded, 7 declined to participate, and 4 had limited mobility and were thus unable to complete stand balance testing or training. Therefore, 104 individuals were eligible and completed the full 8 weeks of the clinical trial. Participants were eligible if they were 20–70 years old, had radiographically confirmed knee fracture, and had received internal fixation surgery. Exclusion criteria were: inflammatory conditions after surgery; history of hip or ankle injury (within the last 3 months); bilateral injury of lower limbs; inability to ambulate without a gait aid; and individuals with any neurological, musculoskeletal, or other conditions affecting movement, balance, and maximal strength of the lower extremity. All participants agreed to this trial voluntarily and gave written informed consent prior to testing. The study was approved by the clinical research ethics board of Guizhou Orthopedics Hospital. A detailed flow diagram of the trial design is shown in Fig. 1.
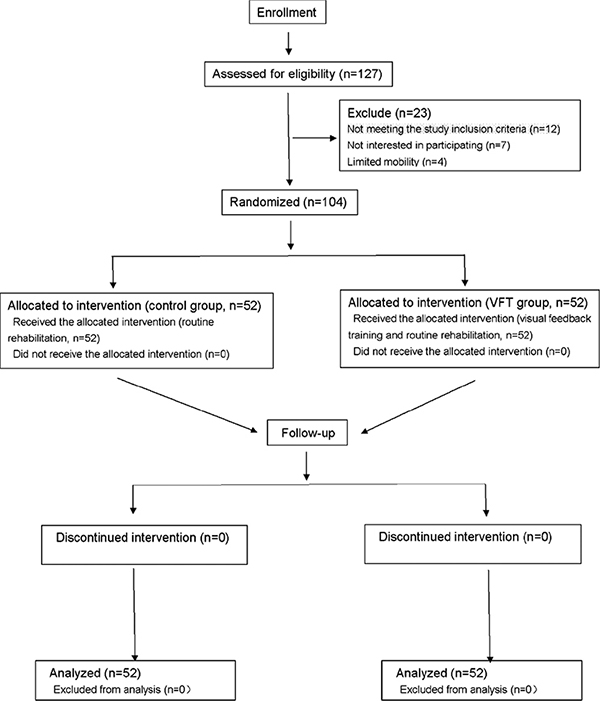
Fig. 1. Flow diagram of patient recruitment and enrolment. VFT: visual feedback training.
Design and setting
This study was a clinical randomized controlled trial with outcomes assessments at 4 and 8 weeks, comparing 2 groups: treatment and control. The trial was registered with the Chinese Clinical Trial Registry (registration number: ChiCTR2000028827). Eligible participants were enrolled and allocated via a randomization system for clinical research using a 1:1 ratio to a treatment group who received visual feedback training (VFT group), or a control group who undertook routine rehabilitation only (control group). The VFT intervention was delivered by a qualified physiotherapist with 6 years of experience in physical therapy. All testing sessions were conducted by 1 rehabilitative physician and 1 research assistant, who were also in charge of the recruitment process. The research assistant and statistician, responsible for gathering and processing data on outcome measurements, were blinded to the treatment grouping.
Intervention
Both groups received routine rehabilitation and TecnoBody® assessments following surgery for knee fracture. The training regimen included ankle pump training, isometric contraction of affected limb muscles, active and passive knee joint stretch training in different positions, and progressive muscle resistance training. In the third week, all eligible participants began weight-bearing activities, including standing with handrails or against the wall, and walking with aids or sticks on plane movement. In addition to the above intervention, the VFT group used the TecnoBody® device for VFT, employing the balance training module; the tilt angle range of the electronic balance plate was set to ± 15° in the front, back, left, and right (Fig. 2). This training module included single- or double-foot control in a straight line and circumference. To perform VFT, the patient’s injured lower limb was placed on the balance plate. Meanwhile, the distance of movement, which is the length and area of the patient’s body’s centre of pressure (COP) movement when it swings in different directions, was traced on the computer monitor. The monitor simultaneously displayed a moving track that followed the route, corresponding to the change in tilt (Figs 3 and 4). The training time for each track was set according to the condition of the injured limb; settings were once a day, 20–30 min each time, 5 times a week. At the end of the trial, both VFT and control groups were evaluated using the Lysholm score, Tinetti gait, and the value of the TecnoBody® test before intervention and after 4 and 8 weeks of treatment.

Fig. 2. Schematic diagram of ankle movement on balance plate.
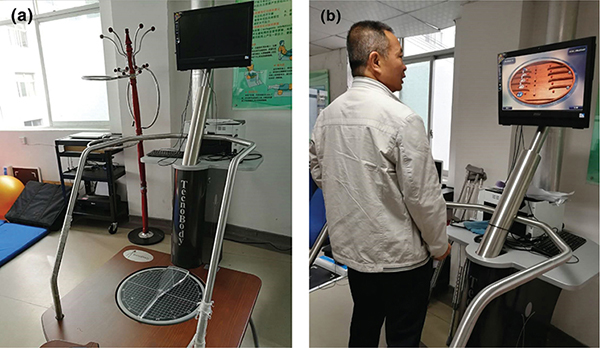
Fig. 3. (a) Tecnbody® device. (b) A patient in the visual feedback training (VFT) group receiving VFT.
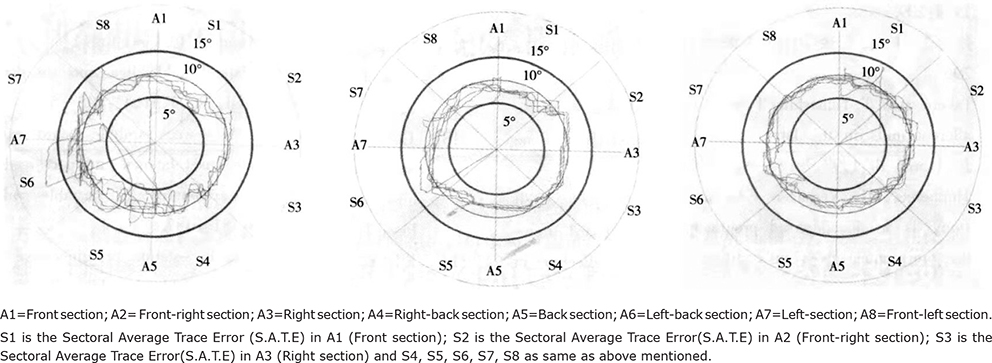
Fig. 4. Motion trajectory images demonstrating foot centre of pressure (COP) on moving track length and moving track area of a patient in the visua feedback training (VFT) group before treatment and after 4 and 8 weeks of treatment.
Outcome measures
Knee function (9). Lysholm score (100 points), which includes the following: claudication, 5 points; supporting, 5 points; interlocking, 15 points; stability, 25 points; pain, 25 points; swelling, 10 points; climbing stairs, 10 points; squatting, 5 points. The total score is proportional to knee joint function; higher scores indicate better knee function.
Balance ability (10). The TecnoBody® system was used to evaluate balance in the standing position for all participants. This equipment provides data on the COP path length and the area over which the COP moves. Smaller values indicate greater stability of lower limbs and balance ability.
Walking ability (10). The Tinetti-HAMA-T scale was used to assess motor control. It contains gait analysis (HAMA-G, 12 points) consisting of starting step, step length and height, step symmetry, step continuity, path, trunk stability, and the step width, and balance test (HAMA-B, 16 points), which consists of sitting balance, getting up, trying to get up, standing balance immediately after getting up, sitting balance immediately after sitting down, nudging, nudging after closing the eyes, and sitting after closing the eyes and turning 360° (9 total aspects). Together, these 2 parts have a total score of 28 points, with a score < 24 indicating balance and walking impairment and < 19 indicating higher risk of falling.
Statistical analysis
All outcomes were measured by the same physical therapist on the day before intervention and the days immediately after completion of 4 weeks and 8 weeks of training. This study conducted an analysis of covariance on post-test scores using pre-test scores as a covariate, which allowed initial differences between the control group and the VFT group to be adjusted for prognostic factors, such as the state of an illness, psychological factors, and body mass index, and the identification of differences between the 2 groups after starting their respective training. All data were analysed by SPSS v19.0 (IBM, Chicago, IL, USA). After adjustment of pre-treatment variables, 2-way mixed-design analysis of variance (ANOVA) with repeated measures was used to compare continuous variables, such as age, body mass index, and the assessment of the scores for Lysholm, Tinetti gait, and the values of length and area measured by TecnoBody, to determine whether there were statistically significant differences within the groups (VFT and control) and between times (post vs pre); all values are presented as means ± standard deviation (SD). Confidence intervals (95% CI) were calculated for any differences between the groups. The training effects within groups at baseline and after training were analysed by paired Student’s t-test. A p-value of < 0.05 was considered statistically significant.
RESULTS
In total, 104 patients were screened and randomly assigned into 2 treatment intervention groups, which were comparable in baseline demographic and clinical measures; all data are shown in Table I. None of the participants reported adverse events during the study period.
Table II shows the differences between the VFT and control groups in the Lysholm scores, Tinetti gait, and TecnoBody® tests of foot COP on moving track length and area for the participants, at baseline and post-intervention. The VFT group showed a significant improvement in TecnoBody® tests of foot COP on moving track length and area after 8 weeks of treatment compared with control; between-group differences were significant. These results suggest that the VFT group improved significantly in the TecnoBody® test compared with the control (p < 0.05, Fig. 5C and 5D). There was no difference between the VFT and control groups regarding Lysholm scores and Tinetti gait before the intervention and at 4 weeks after treatment (p > 0.05, Fig. 5A and 5B). Both groups had improved Lysholm scores and Tinetti gait after 8 weeks (p < 0.05, Fig. 5A and 5B).
| Outcome | Control group (n = 52) | VFT group (n = 52) | p-value between groups | p-value post vs pre | 95% confidence interval between-group difference |
| Lysholm score (points) | |||||
| Pre-training | 54.1 ± 7.2 | 53.9 ± 7.1 | 0.47 | ||
| Week 4 after training | 58.1 ± 7.7 | 62.4 ± 8.0 | 0.314 | 0.301 | 4.2 (1.0, 7.4) |
| Week 8 after training | 69.9 ± 8.7 | 89.2 ± 9.8* | 0.016 | 0.007 | 22.7 (19.9, 25.5) |
| Tinetti gait scale (points) | |||||
| Pre-training | 16.7 ± 2.6 | 16.4 ± 2.3 | 0.515 | ||
| Week 4 after training | 16.8 ± 2.7 | 18.1 ± 2.9 | 0.472 | 0.458 | 1.1 (0.0, 2.3) |
| Week 8 after training | 19.6 ± 3.0 | 23.6 ± 3.2* | 0.033 | 0.026 | 4.6 (3.4, 5.8) |
| Value assessed by TecnoBody – length (mm) | |||||
| Pre-training | 351.5 ± 12.2 | 364.2 ± 12.6 | 0.535 | ||
| Week 4 after training | 338.2 ± 11.9 | 271.2 ± 11.0 | 0.027 | 0.021 | –67.5 (–72.6, –62.4) |
| Week 8 after training | 305.5 ± 11.2 | 193.2 ± 10.6* | 0.001 | 0.001 | –109.9 (–115.4, –104.5) |
| Value assessed by TecnoBody – area (mm2) | |||||
| Pre-training | 243.2 ± 11.9 | 263.2 ± 12.1 | 0.425 | ||
| Week 4 after training | 238.2 ± 11.7 | 215.3 ± 10.9 | 0.037 | 0.035 | –25.0 (–30.6, –19.4) |
| Week 8 after training | 211.8 ± 11.6 | 167.9 ± 9.7* | 0.001 | 0.001 | –45.3 (–50.5, –40.1) |
| Values reported are means±standard deviation (SD). Follow-up values and mean differences were computed after adjusting for baseline values using analysis of covariance. The improvement is indicated by higher Lysholm scores and Tinetti gait scale; lower value of length and area as assessed by TecnoBody. *p < 0.05 for between-groups comparison. |
|||||
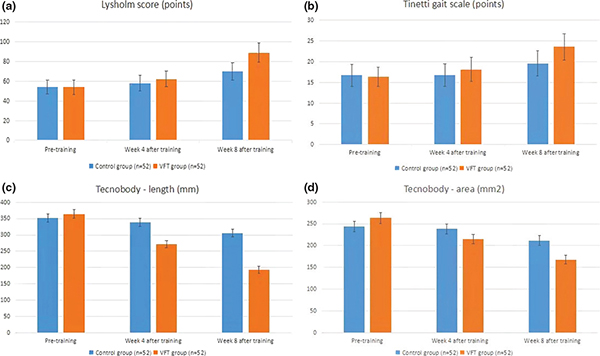
Fig. 5. Differences in the (A) Lysholm scores, (B) Tinetti gait, and (C) TecnoBody tests of foot centre of pressure (COP) on moving track length and area of the participants at baseline and post-intervention between the visual feedback training (VFT) and control groups.
DISCUSSION
The aim of this study was to determine the effect of VFT, using the TecnoBody® device, to improve measures of rehabilitation. After 4 weeks, no significant differences were observed in Lysholm score or Tinetti gait between the treatment and control groups, suggesting that VFT does not have a significant short-term effect regarding knee function and gait. However, the length and area, as evaluated by TecnoBody®, was significantly better than pre-training in the VFT group, and the Lysholm score and Tinetti gait was significantly improved after 8 weeks compared with the pre-treatment and control groups. This suggests that VFT could decrease postural sway and increase motor control in postoperative patients with knee fracture, as well as subsequently improve knee function and balance ability.
In postoperative knee fracture patients, posture control is decreased, lower limb stability is insufficient, and balance function is limited; we believe the mechanism for this dysfunction may be related to the following factors: damaged proprioceptor after knee fracture (11) and/or changes in the central system regulation mechanism of sensation and motion. After the knee joint is damaged, the bilateral proprioception receptor’s afferent information is asymmetrical (12), and thus precise control of the effector is lost. The middle pivot movement system adjusts the control procedure to compensate for the asymmetrical abnormal movement mode, and, consequently, the sensory information from the healthy side of the lower limb is reduced excessively to stabilize patient movement (13). In addition, if the affected limbs remain motionless, this reduced activity may cause decline and degeneration of muscle strength and muscle tension, therefore resulting in insufficient postural stability and increased probability of secondary injury, while post-injury pain might contribute to the poor balance performance (14, 15). A previous clinical study determined that posture control in maintaining dynamic balance was related to the influence of ankle joint movement and arch height after hip and knee joint injury through use of the TecnoBody® system (16).
The ANOVA results of the current study performance (Table II) identified that patients benefited from the therapeutic intervention. The VFT improved balance performance through reducing the moving track length and moving track area of the patient’s injured lower limb on the balance plate when transferring the COP. The potential mechanism of VFT for improving human balance ability is as follows: first, incoming visual information from the eyes play an important role in the maintenance of balance, as it can convey the relative position information between the person and surrounding environmental reference objects, and can also predict external interference (17). Proprioception can perceive changes in space movement and position, and inputs information to the central nervous system. The proprioception input signals from lower limbs are particularly important for maintaining balance. Peterka’s research suggests that reweighing is based on a sensory feedback mechanism and explains how sensory input signals are reprocessed and integrated to construct a unified internal representation and maintain balanced stability (18). Furthermore, balance is achieved through visual feedback and motor control by the central system; when vision or/and proprioception is damaged by fractures or other factors, the brain adapts the reweighing mechanism to ensure processing the incoming information. Thus, the brain uses the remaining sensory information to adjust postural sway, to better maintain the stability of balance (19, 20). Multi-sensory integration is the foundation of balance maintenance in the human body, regulated by postural perception, central motor control and peripheral muscle activity. However, it is also an unstable motion control system; the human body can be regarded as an inverted pendulum model when encountering internal or external sudden force interference (21). Through these prediction and compensatory adjustments, posture is continually changed to maintain balance. In order to maintain ideal balance, the human body needs to collect, integrate and process incoming information from different sensory channels, such as vision and proprioception, and use visual feedback and motor control to maintain balance stability in the process of movement. Compared with previous studies on VTF applied in post-stroke patients, this study raises the additional question as to whether post-injury pain in the lower limbs might be an additional factor slowing down the progression of balance training, which should be addressed in future research.
This study has some limitations. Firstly, the evaluators were not blinded to group allocation of participants, which may have led to bias. Secondly, we were not able to test beyond the 8 weeks of training, and thus further studies are needed to determine long-term outcomes following the conclusion of training. Despite these limitations, this feasibility trial provides important preliminary outcomes for the safety, feasibility and potential effectiveness of VFT for postoperative patients with knee fracture.
CONCLUSION
Applying VFT in conjunction with traditional rehabilitation strategies could decrease postural sway and increase motor control in postoperative patients with knee fracture, as well as subsequently improve knee function and balance ability. This method improves dynamic balance ability in the standing position. Although VFT does not have a short-term effect on knee function and gait, the data suggests that VFT has good potential for training postoperative patients with knee fracture, and thus we conclude that VFT could be a useful addition for rehabilitation of these patients.
ACKNOWLEDGEMENTS
The authors thank LetPub (www.letpub.com) for linguistic assistance and scientific consultation during the preparation of this manuscript.
This clinical trial was supported by the enlarged Health Cooperation Project of Guiyang City Bureau of Science and Technology (number [2019]9-5-5).
REFERENCES
- Huang JF, Shen JJ, Chen JJ, Tong PJ. Primary total knee arthroplasty for elderly complex tibial plateau fractures. Acta Orthop Traumatol Turc 2016; 50: 702–705.
- Takacs J, Krowchuk NM, Garland SJ, Carpenter, MG, Hunt, MA. dynamic balance training improves physical function in individuals with knee osteoarthritis: a pilot randomized controlled trial. Arch Phys Med Rehabil 2017; 98: 1586–1593.
- Lakhani, B, Mansfield A. Visual feedback of the center of gravity to optimize standing balance. Gait Posture 2015; 41: 499–503.
- Srivastava A, Taly AB, Gupta A, Kumar S, Murali T. Post-stroke balance training: role of force platform with visual feedback technique. J Neurol Sci 2009; 287: 89–93.
- Ko Y, Ha H, Bae YH, Lee W. Effect of space balance 3D training using visual feedback on balance and mobility in acute stroke patients. J Phys Ther Sci 2015, 27: 1593–1596.
- Rougier P, Boudrahem S. Effects of visual feedback of center-of-pressure displacements on undisturbed upright postural control of hemiparetic stroke patients. Restor Neurol Neurosci 2010; 28: 749–759.
- Dargo L, Robinson K J. Prevention of knee and anterior cruciate ligament injuries through the use of neuromuscular and proprioceptive training: an evidence-based review. J Athlet Train 2017; 52: 1171–1172.
- In TS, Cha YR, Jung JH, Jung KS. Effects of visual feedback with a mirror on balance ability in patients with stroke. J Phys Ther Sci 2016; 28: 181–185.
- Wang W, Liu L, Chang X, Jia ZY, Zhao JZ, Xu WD, et al. Cross-cultural translation of the Lysholm knee score in Chinese and its validation in patients with anterior cruciate ligament injury. BMC Musculoskel Dis 2016; 17:436.
- Soubra R, Chkeir A, Novella JL. A Systematic review of thirty-one assessment tests to evaluate mobility in older adults. Biomed Res Int 2019 2019: 1354362.
- Arockiaraj J, Korula R J, Oommen A T, Devasahayam S, Wankhar S, Velkumar S, Poonnoose PM, et al. Proprioceptive changes in the contralateral knee joint following anterior cruciate injury. Bone Joint J 2013; 95: 188–191.
- Negahban H, Mazaheri M, Kingma I, van Dieën JH. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 2014; 22: 1491–1504.
- Zhang L, Qi J, Zeng Y. Proprioceptive changes in bilateral knee joints following unilateral anterior cruciate ligament injury in cynomolgus monkeys. Med Sci Monit 2018; 24: 105–113.
- Mat S, Ng CT, Tan MP. Influence of hip and knee osteoarthritis on dynamic postural control parameters among older fallers. J Rehabil Med 2017;49:258–263
- Sanchez-Ramirez DC, van der Leeden M, Knol DL, et al. Association of postural control with muscle strength, proprioception, self-reported knee instability and activity limitations in patients with knee osteoarthritis. J Rehabil Med 2013; 45: 192–197.
- Birinci T, Demirbas SB. Relationship between the mobility of medial longitudinal arch and postural control. Acta Orthop Traumatol Turc 2017; 51: 233–237.
- Chiarovano E, Wang W, Rogers SJ, MacDougall HG, Curthoys IS, de Waele C, et al. Balance in virtual reality: effect of age and bilateral vestibular loss. Front Neurol 2017; 8: 5.
- Peterka RJ. Sensorimotor integration in human postural control. J Neurophysiol 2002; 88: 1097–1118.
- Kabbaligere R, Lee BC, Layne CS. Balancing sensory inputs: sensory reweighting of ankle proprioception and vision during a bipedal posture task. Gait Posture 2017; 52: 244–250.
- Jensen TO, Fischer-Rasmussen T, Kjaer M, Magnusson SP. Proprioception in poor- and well-functioning anterior cruciate ligament deficient patients. J Rehabil Med 2002; 34: 141–149.
- Elliott MT, Wing AM, Welchman AE. Multisensory cues improve sensorimotor synchronization. Eur J Neurosci 2010; 31: 1828–1835.