REVIEW ARTICLE
COMPARISON OF CONTENT AND PSYCHOMETRIC PROPERTIES OF MALNUTRITION OUTCOME MEASURES: A SYSTEMATIC REVIEW
Līga SAVICKA, MSc1,2, Santa SALAKA, MSc1,2 and Guna BĒRZIŅA, MD, PhD1,2
From the 1Department of Rehabilitation, Riga Stradins University and 2Clinic of Rehabilitation, Riga East University Hospital, Riga, Latvia
Objective: To determine the most-often used outcome measures for malnutrition risk and malnutrition, analyse outcome measure content, and assess psychometric properties.
Methods: MEDLINE, SAGE Journals, Web of Science, SCOPUS, ProQuest and Science Direct databases were searched to identify outcome measures. Outcome measure content was compared using the International Classification of Functioning Disability and Health (ICF). Psychometric properties were also systematically searched and compared. This review was prepared according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results: A total of 1,311 studies met the inclusion criteria. The most-often used outcome measures for detecting malnutrition or its risk overall were: body mass index (590), albumin (469), Mini Nutritional Assessment (312), haemoglobin (251), and Subjective Global Assessment (139). The most psychometrically sound outcome measure was Mini Nutritional Assessment, but the most comprehensive measure, covering the most ICF categories, was Patient-Generated Subjective Global Assessment, with a total of 58 meaningful concepts.
Conclusion: The results provide an insight into the content and psychometric quality of malnutrition risk and malnutrition outcome measures. There was some variation between the way reviewers linked meaningful concepts to ICF, and literature gaps were identified regarding psychometric properties. These results can be used to help select the most appropriate malnutrition outcome measure.
LAY ABSTRACT
Malnutrition leads to a decline in physical and mental functioning, as well as activity limitations, which can result in poor disease outcomes and reduced quality of life. Early identification of malnutrition depends on choosing the most appropriate diagnostic method. This article systematically analyses the outcome measures most commonly used in research for detecting malnutrition risk and malnutrition in adults. The content of the most common outcome measures was analysed using the International Classification of Functioning Disability and Health (ICF). Linking rules, and the psychometric properties of the measures were systematically searched, analysed according to an already established framework, and compared.
Key words: malnutrition; outcome measure; International Classification of Functioning Disability and Health; psychometrics; linking.
Citation: J Rehabil Med 2022; 54: jrm00287. DOI: http://dx.doi.org/10.2340/jrm.v54.2447
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Mar 31, 2022; Epub ahead of print: Apr 20, 2022; Published: Jun 20, 2022
Correspondence address: Liga Savicka, Department of Rehabilitation, Rīga Stradiņš University, LV-1067 Rīga, Latvia. E-mail: liga.savicka@gmail.com
Competing interests and funding: The authors have no conflicts of interest to declare.
The World Health Organization (WHO) defines malnutrition as deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients (1). The prevalence of malnutrition in the rehabilitation setting ranges from 14% to 65% worldwide, with the highest prevalence reported in Europe and Australia (2). The prevalence of malnutrition in the (acute) hospital setting has been reported to be 20 – 50%, depending on the patient population, the definition of malnutrition, and the outcome measures or criteria used for diagnosis (3). Keller et al. found the prevalence of malnutrition in 638 long-term care residents from 32 long-term care homes in Canada to range from 28.9% if assessed with InterRAI Long Term Care Facility undernutrition trigger, 33.4% with Patient-Generated Subjective Global Assessment (PG-SGA), and 53.7% with Mini Nutritional Assessment – Short Form (MNA-SF); hence the prevalence depends on the sensitivity and specificity of the specific malnutrition assessment tool (4).
According to the European Society for Clinical Nutrition and Metabolism (ESPEN) Consensus Statement, there are 2 methods of diagnosing malnutrition: body mass index (BMI) < 18.5 kg/m2, or unintentional weight loss > 10% independent of time, or > 5% over the last 3 months combined with either BMI < 20 kg/m2 if < 70 years of age, or < 22 kg/m2 if 70 years of age or older, or fat-free mass index (FFMI) < 15 and 17 kg/m2 in women and men, respectively (5). These diagnostic criteria are supported by the National Institute for Health and Care Excellence (NICE) Clinical Guideline on Nutrition Support for Adults (6) as well as the Global Leadership Initiative on Malnutrition (GLIM) approach, which updates these criteria by including both phenotypic (weight loss %, BMI and muscle mass) and aetiological criteria (reduced food intake or assimilation and inflammation) for the diagnosis of adult malnutrition (7).
According to GLIM criteria, the first step in evaluation of malnutrition is the identification of malnutrition risk, which can be done by using any validated screening tool (8). Diagnosis of malnutrition, however, consists of several additional criteria or components of qualitative or quantitative outcome measures (9). Therefore, authors searched for both malnutrition risk and malnutrition outcome measures, as both are components in the diagnostic process.
For this article, different components used for malnutrition diagnosis were each considered a separate outcome measure. Outcome measures were defined by using International Classification of Health Interventions (ICHI) as any measurements (quantitative determination of characteristics using units of measurement) or tests (review or examination using a questionnaire, rating scale or other instrument) (10).
A person’s functioning and disability is conceived as a dynamic interaction between health conditions and contextual factors, and malnutrition is no exception (11). It has many associated consequences; amongst which are a decline in physical and mental functions, causing dependency in activities of daily living, which can result in hospitalizations and longer hospital stays, poor disease outcomes and reduced quality of life (12, 13). Therefore, all healthcare professionals, and not only nutritionists and dietitians, should be knowledgeable about malnutrition and its assessment.
Information on the psychometric properties and content of the most-often used malnutrition and malnutrition risk outcome measures needs to be systematically reviewed in order to improve evidence-based practice. The latest available evidence on this topic includes Xu & Vincent’s 2020 article on the measurement properties of malnutrition assessment tools for use in hospitals. The authors concluded that the use of the Subjective Global Assessment (SGA), PG-SGA and Mini Nutritional Assessment (MNA) can be supported, but that more studies with sound methodology are needed to assess their responsiveness to change (14). Miller et al. published an article in 2018 about the lack of validated screening tools for simultaneously assessing cachexia, sarcopaenia and malnutrition (15). Marshall et al., in a 2018 systematic review and meta-analysis, concluded that, other than MNA, there is insufficient evidence to recommend a particular assessment tool (16). Zhang et al.’s 2017 study systematically reviewed and evaluated many different malnutrition biomarkers, and showed that BMI, haemoglobin and total cholesterol are useful biomarkers of malnutrition in older adults (17). However, to our knowledge, there is no evidence on the comprehensive comparison of the content of the outcome measures used according to the International Classification of Functioning, Disability and Health (ICF) (11). The aims of this systematic review were therefore to determine the most-often used outcome measures for malnutrition risk or malnutrition, to analyse the content of outcome measures by linking meaningful concepts with the ICF, and to assess the psychometric properties of outcome measures.
METHODS
This review was prepared and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (18).
MEDLINE, SAGE Journals, Web of Science, SCOPUS, ProQuest and Science Direct databases were searched for studies published up to October 2019. Search strategies were created using the keyword “malnutrition” and MeSH terms (if available in the database) and adding Boolean operators. The search strategies used in each database are shown in Appendix 1. Appropriate search filters were then added: “language (articles in English)”; “article type (randomized controlled trial, clinical trial)”; “publication date (2010–2019)”; “species (human)”; and “age (18+)”.
Inclusion criteria for this systematic review were: (i) research design (randomized controlled trial, observational studies, cross-sectional studies, qualitative studies); (ii) at least 1 outcome measure is reported as an outcome variable within the article (screening, clinical assessment, subjective (healthcare personnel and caretakers’ perspective) and/or quality-of-life outcome measures); (iii) article published between 2010 and October 2019; (iv) article in English; (v) research with human subjects; and (vi) study participants aged 18 years or older. Exclusion criteria were: (i) laboratory or genetic studies; and (ii) retracted articles.
One reviewer reviewed the titles and abstracts of studies to determine their eligibility for inclusion. Studies that clearly did not meet the inclusion criteria were excluded at this point. Those that could not be clearly assessed were included and analysed in full text. Studies that met the inclusion criteria were included and further analysed. Data on study design, participant group and amount, as well as outcome measures used in the studies were then extracted from all included studies. Information on frequency of clinical assessments (clinical signs and medical history) was not included in this study, as they do not represent a form of standardized outcome measures. The cut-off for the most-often used outcome measures that were included in further analysis in each group was 5%. To obtain more objective and realistic results and to include a larger selection of research articles, representing as many patient groups as possible, lower levels of evidence (e.g. case reports) were also included. Therefore, the methodological quality of the included studies was not assessed.
ICF linking process
The most commonly used functional outcome measures were selected for the linking process. Two reviewers with prior knowledge of the ICF and linking procedure performed the linking process independently, based on the ICF linking rules described by Cieza et al. (19, 20). Meaningful concepts were first identified, then linked to the most precise ICF category. Wherever possible, consensus between reviewers was reached, either with a discussion or with an opinion from a third reviewer. Agreement between reviewers was determined by calculation of Cohen’s kappa coefficient (κ). Values were interpreted according to Cohen’s 1960 study, where ≤0 = no agreement, 0.01 – 0.20 = none to slight agreement, 0.21 – 0.40 = fair agreement, 0.41 – 0.60 = moderate agreement, 0.61 – 0.80 = substantial agreement, and 0.81 – 1.00 = almost perfect agreement (21).
Analysis of psychometric properties
A search for articles reviewing the properties of functional outcome measurement was performed in PubMed. Search algorithms used on PubMed are shown in Appendix 2. References listed in the articles found were also screened.
Properties and quality criteria were chosen based on Terwee et al.’s 2017 study (22). The following psychometric properties were described: content validity, internal consistency, criterion validity, construct validity, reproducibility (agreement and reliability), responsiveness, floor and ceiling effects, and interpretability. For each measurement property criteria (positive, negative, indeterminate) defined by Terwee et al. were used (22). When analysing psychometric properties, the original target population was interpreted first. If data on the original population were missing, other studies were taken into account.
RESULTS
A total of 11,225 studies were identified through the databases. Of these, 3,923 duplicates were excluded. After removal of duplicates and the screening process, 1,631 full-text articles were reviewed for eligibility. Of these, 320 did not meet inclusion criteria, and 1,311 studies were included in qualitative synthesis. Fig. 1 shows the flow of study selection.
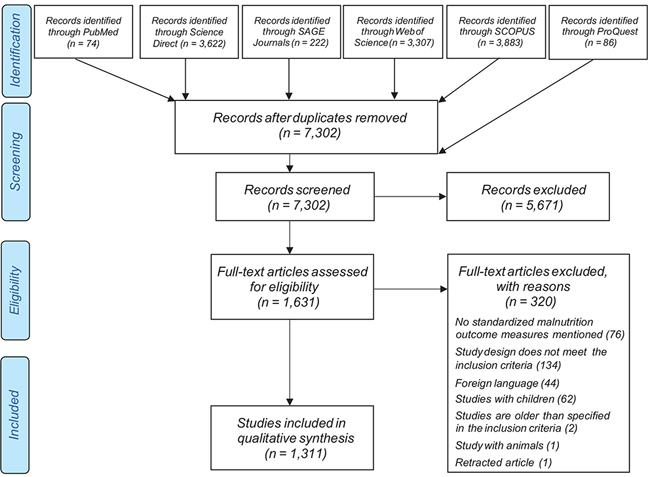
Fig. 1. Study selection flowchart.
Outcome measures
Out of 215 identified outcome measures, 92 were functional assessments, 59 were laboratory tests, 3 were instrumental assessments, and 61 were anthropometric indicators. Nineteen of the instruments identified were subject to further analysis. The most commonly used outcome measures from all groups are shown in Table I.
Outcome measure linking to International Classification of Functioning, Disability and Health
A total of 200 meaningful concepts were identified after outcome measure item analysis: 24 SGA, 33 Nutritional Risk Screening 2002 (NRS-2002), 34 Malnutrition Universal Screening Tool (MUST), 58 PG-SGA, 38 MNA. There was only 1 meaningful concept for each of: BMI, indirect calorimetry, body loss percentage, handgrip strength, albumin, haemoglobin, cholesterol, arm circumference, arm muscle circumference, bioelectrical impedance analysis (BIA), dual-energy X-ray absorptiometry (DEXA), triceps skinfold thickness, and waist circumference.
Functional assessments (standardized assessment tools) (PG-SGA, NRS-2002, MNA, MUST and SGA) are the most comprehensive of the outcome measures, covering the most components of the ICF. The majority of outcome measures were predominantly covered by Body Function and Activity and Participation components. Three PG-SGA concepts (5%) were found to not be covered by the ICF.
All laboratory tests covered 1 category from the Body Structure component – structure of cardiovascular system (s410). Indirect calorimetry also only covered 1 category, which is from the Body Function component (general metabolic functions (b540). BIA and DEXA contain concepts, which were not covered by the ICF.
Tables II–III show the results of anthropometric and functional outcome measure linking with ICF. The agreement between reviewers regarding the linking of most commonly used malnutrition outcome measures with ICF is summarized in Table IV.
Analysis of psychometric properties
Psychometric property analysis was performed for all functional outcome measures (MNA, SGA, NRS-2002, MUST and PG-SGA). Overall, 42 studies that described psychometric properties were included. A summary of the measurement properties in different study populations is shown in Table V.
| Measurement | Content validity | Criterion validity | Construct validity | Internal consistency | Reproducibility | Responsiveness | Floor or ceiling effect | Interpretability | Study population | Study author and year | |
| Agreement | Reliability | ||||||||||
| MNA | ? + |
– | – | – + |
0 | 0 | – + + |
+ | 0 | Elderly | Guigoz Y et al., 1999; Guigoz Y et al., 1994; Amirkalali B et al., 2010; Woldekidan et al., 2020; Machado RS et al., 2015 |
| 0 | – | 0 | – + |
0 | 0 | + | 0 | 0 | Hospitalized elderly | Doroudi T et al., 2019; Jacobsen EL et al., 2016 |
|
| 0 | – | 0 | – | 0 | 0 | + | 0 | 0 | Healthy individuals | Ghazi L et al., 2015 | |
| 0 | – | 0 | + | 0 | 0 | + | 0 | 0 | Parkinson’s disease patients | Ghazi L et al., 2015 | |
| 0 | 0 | 0 | + | 0 | + | 0 | 0 | 0 | Institutionalized elderly | Bleda MJ et al., 2002 | |
| 0 | + | 0 | ? | 0 | ? | 0 | 0 | ? | Elderly rehabilitation patients | Neumann SA et al., 2007 | |
| 0 | 0 | 0 | – | 0 | – | + | 0 | 0 | Elderly outpatients | Soysal P et al., 2019 | |
| 0 | 0 | 0 | 0 | + | 0 | 0 | 0 | 0 | Stroke patients | Lin SC et al., 2019 | |
| SGA | 0 | 0 | 0 | 0 | 0 | ? | – | 0 | 0 | Peritoneal dialysis patients | Yun T et al., 2017; Visser R et al., 1999 |
| 0 | 0 | 0 | + | 0 | ? | 0 | 0 | 0 | Liver-transplant candidates | Hasse J et al., 1993 | |
| 0 | – | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Surgical patients | Almeida AI et al., 2012 | |
| ? | 0 | 0 | 0 | + | + | 0 | 0 | 0 | Hospitalized patients before gastrointestinal surgery | Detsky AS et al., 1987 | |
| 0 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | Hemodialysis patients | Steiber A et al., 2007 | |
| 0 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | Patients with end stage renal disease | Cooper BA et al., 2002 | |
| NRS-2002 | + | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Various diagnostic groups | Kondrup J et al., 2003 |
| 0 | 0 | – | 0 | 0 | 0 | 0 | 0 | 0 | Surgical patients | Almeida AI et al., 2012 | |
| 0 | 0 | 0 | 0 | 0 | + + |
+ + + |
0 | 0 | Hospitalized patients | Bolayir B et al., 2019; Cuong TQ et al., 2019; Tran QC et al., 2018; Young AM et al., 2013 |
|
| MUST | + | – | – | + | 0 | + | + | 0 | 0 | Hospitalized patients | Hormozi S et al., 2019; Mosli MH et al., 2019; Sharma Y et al., 2017; Lawson CS et al., 2012; Tran QC et al., 2018 |
| 0 | – | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Surgical patients | Almeida AI et al., 2012 | |
| 0 | + | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Oncological patients | Boleo-Tome C et al., 2012 | |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ? | Elderly | Elia M et al., 2003 | |
| PG-SGA | + ? + |
0 | ? | + – |
0 | 0 | ? | 0 | 0 | Oncological patients | Sealy MJ et al., 2017; Tobberup R et al., 2018; Henriksen C et al., 2018; Tsilika E et al., 2015; Bauer J et al., 2002; Fu ZM et al., 2018; Isenring EA et al., 2004 |
| ? ? |
0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Hospital and outpatient clinic participants | Erickson N et al., 2018; Gonzalez MC et al., 2018 |
|
| ? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Hospitalized patients | Balstad TR et al., 2019 | |
| 0 | ? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Elderly | Marshall S et al., 2015 | |
| ? | 0 | 0 | 0 | 0 | + | 0 | 0 | 0 | Stroke patients | Yoo SH et al., 2009 | |
| Rating: +: positive; –: poor; ?: lacking clear description or doubtful design or methods; 0: no information available (22). | |||||||||||
| MNA: Mini Nutritional Assessment; MUST: Malnutrition Universal Screening Tool; NRS-2002: Nutritional Risk Screening 2002; PG-SGA: Patient-generated Subjective Global Assessment; SGA: Subjective Global Assessment. | |||||||||||
MNA proved to have positive content validity for its original population, elderly patients (23). Internal consistency was positive for patients with Parkinson’s disease, institutionalized Spanish elderly people, Turkish geriatric outpatients, Ethiopian elderly patients, and Norwegian acute geriatric patients (24–28). Criterion validity was positive only in Norwegian geriatric nursing home patients (29). Agreement was positive in Chinese stroke patients and test-retest reliability was positive in institutionalized Spanish elderly people (27, 30). Responsiveness was positive in all populations tested, except for Iranian elderly people (24, 26, 28, 31, 32). No floor or ceiling effect was found for MNA (25). Interpretability was lacking clear description in older Australian patients undergoing rehabilitation (33). Construct validity for the MNA Portuguese version in Brazilian elderly people was poor (34).
Regarding SGA, no information could be found on construct validity, floor or ceiling effect and interpretability. Content validity was lacking a clear description about the item selection process and target population (patients) were not involved at all in item selection (35). Internal consistency was positive for adult liver-transplant candidates (36). Agreement and inter-rater reliability were positive for the target population, but responsiveness was poor (35, 37). Criterion validity in Portuguese surgical patients was poor (38). Intra-rater reliability in haemodialysis patients was also poor (39).
Only 5 studies on NRS-2002 with an inpatient population were found. There was no information on internal consistency, construct validity, agreement, floor or ceiling effect and interpretability. Content validity in the original population was positive (40). Criterion validity in Portuguese surgical patients was poor (38). Inter-rater reliability was positive in both Turkish and Vietnamese inpatient populations (41, 42). Responsiveness was positive in Vietnamese and Australian inpatient populations (42–44).
For MUST, no information was found on agreement and floor or ceiling effects. Content validity was described as positive for hospitalized Iranian geriatric patients (45). Internal consistency and inter-rater reliability were positive in Arabian patients with inflammatory bowel disease; however, test-retest reliability was poor (46). Criterion and construct validity were poor in all populations tested (38, 47–49). Responsiveness was positive in Vietnamese inpatient population (43). A clear description on interpretability was lacking in a geriatric population, as means and SD scores of only 2 subgroups were given (50).
PG-SGA had no information on agreement, floor or ceiling effect and interpretability. Content validity and internal consistency were positive in the target population (51–53). Reliability was positive in Korean stroke patients (54). Different methods than preferred by Terwee et al. (22) were used to describe PG-SGA criterion validity in geriatric population, and therefore criterion validity for geriatric population was marked as indeterminate (55). A study on PG-SGA construct validity in Chinese target population was lacking a clear description of the hypotheses tested, thus it could not be interpreted as positive or poor (56).
DISCUSSION
This review identified 215 outcome measures that have been used in research as components to measure malnutrition risk or malnutrition. While authors agree that the concepts “malnutrition” and “risk of malnutrition” differ, outcome measures that are components for diagnosis of malnutrition are stand-alone assessments for malnutrition risk; for example, MNA, MUST, and NRS-2002. Perhaps the issue is one of terminology: malnutrition, risk of malnutrition and malnutrition diagnosis. GLIM combines diagnostic criteria for diagnosis of malnutrition. Validated tools are considered malnutrition screenings only in the context of GLIM, because within the outcome measures themselves, they score the patient as “malnourished” all the same. The issue is that, within the tools, the term “malnutrition” is still being used, even if, alone, it does not determine the diagnosis of malnutrition.
The identified outcome measures are diverse and can be categorized into 4 types: (i) functional assessment tools, (ii) laboratory tests, (iii) instrumental assessments, and (iv) anthropometric indicators. The 19 most commonly used tools covered 47 categories when linked to the ICF. An extensive systematic search of the literature was also performed in order to identify and compare the psychometric properties of functional assessment tools. The available evidence was related mostly to responsiveness, reliability and internal consistency of the instruments.
Body mass index (BMI) has been established in this review as, overall, the most commonly used component in malnutrition diagnostics. BMI is a useful measurement for the majority of adults; however, it is flawed if used alone, because it is dependent only on height and weight. It fails to account for any other personal factors that are important in the diagnosis of malnutrition, such as age, ethnicity, sex, physical activity and body composition. Standards of good clinical practice include complex malnutrition assessment to obtain a diagnosis of malnutrition, consisting of several components, such as the GLIM model, however, research articles show that these components are often also used separately, as is the case for BMI.
Therefore, for accurate diagnosis of malnutrition it is necessary to use BMI in addition to other outcome measures. For example, waist circumference can provide additional information on visceral adiposity. Due to its ease of use, BMI is included in many functional assessment tools, such as MNA, NRS-2002 and MUST. BMI parameters do measure nutritional status, but have been supplemented by other important items, making such functional assessment tools accurate in diagnosing risk of malnutrition, compared with BMI alone, as shown in 2016 in a study by Miranda et al. (57). The other most commonly used anthropometric indicators for nutritional assessment in this review were arm circumference, weight loss percentage, arm muscle circumference, triceps skinfold thickness and waist circumference. These are cost-effective, simple and quick, and the results can be compared with the values for a general population. However, other anthropometric indicators have similar issues to BMI; the results, by themselves, are not reliable for all patient groups. For example, assessing only arm circumference or arm muscle circumference in patients with upper extremity oedema would not correctly portray quantity of fat and muscle mass; hence the addition of other assessments is necessary.
Anthropometric indicator content in itself is not very comprehensive and covers only the Body Structure and Body Function components of the ICF. Categories from component Body Structures that were most often linked to were “s730 Structure of upper extremity”, indicating an item construct assessing arm circumference or arm muscle circumference and “b530 Weight maintenance functions”, measured by BMI and body weight loss percentage.
Since anthropometric measurements on their own do not give enough information about body composition and are subject to measurement variability, instrumental assessments can be useful, offering accurate results. Three commonly used instrumental assessments were identified in this review, with 2 of them being body composition assessments (BIA and DEXA) and 1 being a measurement of energy expenditure (indirect calorimetry). BIA was identified as the most-often used body composition instrumental assessment. It is a quick non-invasive method, but requires strict adherence to certain procedures beforehand, such as, fasting for 2 h (58). DEXA is considered an even more accurate method and is consistent with anthropometric measurements (59). DEXA is a reliable and easy-to-perform method, which can help quickly detect early malnutrition and monitor changes in nutritional status (58, 59). However, even though the radiation dose of a single DEXA measurement is low, it is not recommended for pregnant women (58), and DEXA requires specialized, expensive radiology equipment, therefore it is not as feasible in clinical practice as BIA, which is a low-cost device. If no devices are available, combinations of other assessment methods (anthropometrics and laboratory tests) can be used for the assessment of body composition; however, they will be less accurate than instrumental assessments.
Indirect calorimetry was reported as an outcome measure used in 8% of studies included in this review. Indirect calorimetry determines energy expenditure by measuring pulmonary gas exchanges, which allows clinicians to determine the requirements for patients’ energy intake and is a non-invasive technique (60, 61). For calculating energy expenditure, validated equations can be used as well, however, within the scope of this review, indirect calorimetry remains the only method mentioned. Overall, it is the most accurate assessment of energy expenditure and remains the gold standard (60).
Content of body composition instrumental measurements (BIA and DEXA) was found to not be covered in detail by the ICF. Aspects such as body water or fat mass could potentially be linked to Body structure category s598 “Structures related to the digestive, metabolic and endocrine systems, other specified”. However, updated linking rules advise against using “other specified” categories if the content of a meaningful concept is not explicitly named (13); therefore, they were marked as “not covered”.
The first step towards diagnosis of malnutrition is screening for malnutrition risk with a valid tool (8). The most-often used functional assessment tools were MNA, SGA, NRS-2002, MUST and PG-SGA.
MNA, designed for use in elderly patients, shows overall positive psychometric properties, with the only exception being poor construct validity and indeterminate interpretability, where further studies with clearly described minimal important change are necessary. MNA was also the second most comprehensive functional assessment tool, covering 19 ICF categories from all components, including Personal Factors (9 Body Functions, 2 Body Structures, 7 Activities and Participation, 1 Environmental Factors, and 5 Personal Factors). Ten out of 14 identified studies on psychometric properties of MNA were performed with a geriatric population. Therefore, based on our analysis of the available data, MNA can be recommended for use in elderly patients; however, there are insufficient studies available to be able to draw conclusions regarding other patient groups.
SGA and NRS-2002 were originally both validated for hospitalized patients. Despite several studies being available for this patient group, SGA does not clearly demonstrate positive psychometric properties. Content validity was indeterminate, responsiveness was poor, and criterion validity with BMI was also poor. However, internal consistency, agreement and reliability were scored positively. SGA content covers 15 ICF categories over components Body Functions (9 categories) and Activities and Participation (6 categories) and Personal Factor (1 category). Of all the functional assessment tools, NRS-2002, however, had the largest literature gap. No studies could be found on NRS-2002 internal consistency, among other properties, which is in agreement with Millers 2018 systematic review (9), even though first validation studies on the outcome measure were published in early 2000s. Similarly to SGA, NRS-2002 also received a positive rating on 3 different measurement properties; however, it lacks too much overall information to receive a strong recommendation from the authors of this review for use in hospitalized patients. Content analysis revealed that it is also less comprehensive, compared with SGA, covering only 2 categories of Body Functions, 2 contextual factors, and several health conditions.
MUST is intended to be a universal screening tool. However, the available studies mostly tested measurement properties in hospitalized patients, to enable comparison with SGA and NRS-2002. This review shows that, overall, MUST has more available evidence and receives a positive rating for more measurement properties, based on criteria by Terwee et al. (22). Information is lacking for other care settings. Content analysis shows MUST covers 4 Body Function categories, 2 Body Structure categories, 2 Activities and Participation categories, and 4 Environmental Factors categories. It also includes some Personal Factors and Health Conditions. Based on the available evidence, perhaps MUST is a more suitable assessment tool for use in hospitalized patients, compared with SGA and NRS-2002.
PG-SGA is a comprehensive outcome measure, including both patients’ and physicians’ perspectives. Studies are available on different patient groups besides oncological patients, such as outpatients, hospitalized stroke patients and elderly patients. PG-SGA shows several good properties, however, there is a lack of strong evidence on responsiveness, to provide context for clinically meaningful changes in results, which was also established by Xu et al. (2020)’s systematic review, making it clear that further research is necessary (14). PG-SGA is the most comprehensive of all functional outcome measures, covering 25 different ICF categories of all components and Health Conditions. The majority of meaningful concepts were linked to the Body Function categories; however, some were not covered by the ICF. Those meaningful concepts were body structures in conjunction with body composition, which were not described clearly enough to link to a specific category, such as, fat and fluid, similarly to meaningful concepts identified with BIA and DEXA.
Most functional assessment tool constructs, assessing malnutrition, were linked to ICF categories “b510 Ingestion functions” and “b530 Weight maintenance functions”. Those include aspects connected with swallowing and digestion of food, as well as functions of maintenance of acceptable BMI, which is a construct measured in many functional assessment tools. The impact of malnutrition on everyday activities, based on outcome measure content, seems mainly to be related to mobility and self-care. The ability to perform activities, such as “changing basic body position” or “eating”, were assessed in MNA, NRS-2002 and PG-SGA. The most-often covered Environmental Factor category was e110 Products or substances for personal consumption. Outcome measures that included constructs linked to this category were assessing aspects such as meals eaten daily and products consumed, consistency of diet, and necessity for special diets or drugs. Regarding Personal Factors, weight and height were mostly included as separate items to determine a patient’s BMI. Health conditions mentioned in outcome measures were used as an additional factor that increases risk of malnutrition. For example, NRS-2002, MUST and PG-SGA included kidney failure, oncological diseases and intensive care patients as such.
Kappa coefficient values show that the functional outcome measure content has less agreement between reviewers (Table IV). Since functional outcome measure content has more meaningful concepts that can be linked to the ICF, compared with instrumental assessments or anthropometric indicators, interpretations of those concepts tend to differ between reviewers, based on how the item has been phrased. Instrumental assessments and laboratory tests, each with only 1 meaningful concept, had almost perfect reviewer linking agreement.
The most commonly used laboratory tests in the process of malnutrition diagnostics, in this review, were albumin, haemoglobin, cholesterol, vitamin B12 and pre-albumin. Content analysis showed that laboratory tests cover only 1 ICF category. While not being comprehensive, laboratory tests are designed to answer specific clinical questions. According to ESPEN guidelines on definitions and terminology of clinical nutrition, biochemical markers should not be used as indicators of a patient’s overall nutritional status (58). Albumin might be useful for measuring degree of catabolism/inflammation (62). With careful interpretation, under some circumstances, albumin and pre-albumin may be monitored for long- and short-term effects (58, 63). The British Association for Parenteral and Enteral Nutrition advises assessing haemoglobin levels for iron status and indication of anaemia; micronutrients, including vitamins, could be affected if inflammation or infection is present, so should be measured when C-reactive protein is low (62). Therefore, not all laboratory tests are components of currently accepted malnutrition definition; rather, they can be associated with nutrition risk, not malnutrition itself (64).
Nutritional status is determined as a result of the nutritional intake, absorption and influence of other factors, such as the presence of disease. A single measure cannot provide a comprehensive assessment. In the absence of 1 gold standard assessment, different groups of nutrition assessments are combined, as malnutrition impacts functioning on different levels. This review identified that, in the literature, albumin is the most commonly used laboratory test, even though it correlates with patients’ risk for adverse outcomes rather than with protein-energy malnutrition. The most-often used functional assessment tool was MNA, which also includes BMI, calf circumference, and other anthropometric indicators. The most comprehensive outcome measure, based on content analysis, was PG-SGA. Based on measurement property analysis, MNA is recommended for use in elderly patients and MUST for use in hospitalized patients. In addition, BIA is used most often for body composition analysis and indirect calorimetry, for determining resting energy expenditure.
Study limitations
This was a comprehensive review in which a large number of studies and all levels of evidence were included; therefore no quality assessment on included articles was performed.
The linking process showed that there was variance in how both reviewers interpreted the meaningful concepts of some measures. It was especially common with the more comprehensive functional outcome measures. Since some concepts could not be interpreted unequivocally it was intentional that the authors did not strive for consensus in 100% of final linking decisions, rather leaving it open for interpretation. Keeping in mind that the agreement between reviewers in all cases was still high enough to reach at least substantial level, these results can be used as a reference regarding the content of malnutrition outcome measures.
The framework used for outcome measure psychometric property analysis included in advance defined criteria, and thus not all results obtained in studies could be interpreted as either positive or poor, but rather sometimes depicted a lack of quality research on a topic.
Further studies with sound methodological quality need to be performed on specific outcome measures, such as SGA, NRS-2002 and PG-SGA. Overall, information was missing on several outcome measure properties (concurrent validity, construct validity, floor or ceiling effect and interpretability), which should also be addressed in further studies.
CONCLUSION
This review identified BMI as the most commonly used component for assessment of malnutrition. No overall quality score was given, so there is no single objective answer as to which might be the psychometrically best, validated assessment tool in all cases. In conclusion, within the scope of this study, for elderly people, the best, validated assessment tool might be the MNA and, for hospitalized patients, the MUST. However, the most comprehensive outcome measure, covering the most ICF categories, is the PG-SGA, with 58 meaningful concepts in total.
In clinical practice, malnutrition diagnostics are complex, including several outcome measures; hence careful consideration is necessary and other factors, mainly the aim of the measurement, the time-frame for administering and interpreting it, and cost, must be taken into account.
ACKNOWLEDGEMENTS
The research received funding from project No 18-00-A01612-000006 financed by European agricultural fund for rural development.
REFERENCES
- World Health Organization, Malnutrition. 2020 [cited 2020 Nov 8]. Available from: https://www.who.int/news-room/q-a-detail/malnutrition
- Marshall S. Protein-energy malnutrition in the rehabilitation setting: evidence to improve identification. Maturitas 2016; 86: 77–85.
- Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health 2011; 8: 514–27.
- Keller H, Vucea V, Slaughter SE, Jager-Wittenaar H, Lengyel C, Ottery FD, et al. Prevalence of malnutrition or risk in residents in long term care: comparison of four tools. J Nutr Gerontol Geriatr 2019; 38: 329–344.
- Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition – an ESPEN Consensus Statement. Clin Nutr 2015; 34: 335–340.
- National Collaborating Centre for Acute Care, Nutrition Support for adults: oral nutrition support, Enteral tube feeding and parenteral nutrition. The Royal College of Surgeons of England, London, 2006.
- Kirsch R, Matthews K, Williams V. Using global criteria to detect malnutrition: application in disease states. Nutr Clin Pract 2020; 35: 85–97.
- Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition – a consensus report from the global clinical nutrition community. Clin Nutr 2019; 38: 1–9.
- Cifu DX. Braddom’s physical medicine & rehabilitation. Fifth edition. Philadelphia, PA: Elsevier; 2016.
- International Classification of Health Interventions (ICHI). 2021 [cited 2022 Mar 14]. Available from: https://www.who.int/standards/classifications/international-classification-of-health-interventions
- International Classification of Functioning, Disability and Health. Geneva: World Health Organization, 2001.
- Corish CA, Bardon LA. Malnutrition in older adults: screening and determinants. Proc Nutr Soc 2019; 78: 372–379.
- Diekmann R, Wojzischke J. The role of nutrition in geriatric rehabilitation. Curr Opin Clin Nutr Metab Care 2018; 21: 14–18.
- Xu YC, Vincent JI. Clinical measurement properties of malnutrition assessment tools for use with patients in hospitals: a systematic review. Nutr J 2020; 19: 106.
- Miller J, Wells L, Nwulu U, Currow D, Johnson MJ, Skipworth RJE. Validated screening tools for the assessment of cachexia, sarcopenia, and malnutrition: a systematic review. Am J Clin Nutr 2018; 108: 1196–1208.
- Marshall S, Craven D, Kelly J, Isenring E. A systematic review and meta-analysis of the criterion validity of nutrition assessment tools for diagnosing protein-energy malnutrition in the older community setting (the MACRo study). Clin Nutr 2018; 37: 1902–1912.
- Zhang Z, Pereira SL, Luo M, Matheson EM. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and Meta-Analysis. Nutrients 2017; 9.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535.
- Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF Linking rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil 2019; 41: 574–583.
- Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med 2005; 37: 212–218.
- Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960; 20: 37–46.
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60: 34–42.
- Yves G, Vellas B, Garry PJ. Mini nutritional assessment: a practical assessment tool for grading the nutritional state of elderly patients. Facts Res Gerontol 1994; 2: 15–59.
- Woldekidan MA, Haile D, Shikur B, Gebreyesus SH. Validity of Mini Nutritional Assessment tool among an elderly population in Yeka sub-city, Addis Ababa, Ethiopia. S Af J Clin Nutrit 2021; 34: 103–109.
- Jacobsen EL, Brovold T, Bergland A, Bye A. Prevalence of factors associated with malnutrition among acute geriatric patients in Norway: a cross-sectional study. BMJ Open 2016; 6: e011512.
- Ghazi L, Fereshtehnejad SM, Abbasi Fard S, Sadeghi M, Shahidi GA, Lokk J. Mini Nutritional Assessment (MNA) is rather a reliable and valid instrument to assess nutritional status in Iranian healthy adults and elderly with a chronic disease. Ecol Food Nutr 2015; 54: 342–357.
- Bleda MJ, Bolibar I, Pares R, Salva A. Reliability of the Mini Nutritional Assessment (MNA) in institutionalized elderly people. J Nutr Health Aging 2002; 6: 134–137.
- Soysal P, Isik AT, Arik F, Kalan U, Eyvaz A, Veronese N. Validity of the mini-nutritional assessment scale for evaluating frailty status in older adults. J Am Med Dir Assoc 2019; 20: 183–187.
- Fossum M, Terjesen S, Ehrenberg A, Ehnfors M, Soderhamn O. Evaluation of the Norwegian version of the mini nutritional assessment (MNA®) among older nursing home patients. VÅRD I NORDEN 2/2009; 92: 50–52.
- Lin SC, Lin KH, Lee YC, Peng HY, Chiu EC. Test-retest reliability of the Mini Nutritional Assessment and its relationship with quality of life in patients with stroke. PLoS ONE 2019; 14: e0218749.
- Amirkalali B, Sharifi F, Fakhrzadeh H, Mirarefin M, Ghaderpanahi M, Larijani B. Evaluation of the mini nutritional assessment in the elderly, Tehran, Iran. Public Health Nutr 2010; 13: 1373–1379.
- Doroudi T, Alizadeh-Khoei M, Kazemi H, Hormozi S, Taati F, Ebrahimi M, et al. Comparison of two validation nutrition tools in hospitalized elderly: Full mini nutritional assessment and short-form mini nutritional assessment. Int J Prev Med 2019; 10: 168.
- Neumann SA, Miller MD, Daniels LA, Ahern M, Crotty M. Mini Nutritional Assessment in geriatric rehabilitation: Inter-rater reliability and relationship to body composition and nutritional biochemistry. Nutrition & Dietetics, 2007; 64: 179–185.
- Machado RS, Coelho MA, Veras RP. Validity of the portuguese version of the mini nutritional assessment in brazilian elderly. BMC Geriatr 2015; 15: 132.
- Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr 1987; 11: 8–13.
- Hasse J, Strong S, Gorman MA, Liepa G. Subjective global assessment: alternative nutrition-assessment technique for liver-transplant candidates. Nutrition 1993; 9: 339–343.
- Yun T, Ko YE, Kim SJ, Kang DH, Choi KB, Oh HJ, et al. The additional benefit of weighted subjective global assessment (SGA) for the predictability of mortality in incident peritoneal dialysis patients: a prospective study. Medicine (Baltimore) 2017; 96: e8421.
- Almeida AI, Correia M, Camilo M, Ravasco P. Nutritional risk screening in surgery: valid, feasible, easy! Clin Nutr 2012; 31: 206–211.
- Steiber A, Leon JB, Secker D, McCarthy M, McCann L, Serra M, et al. Multicenter study of the validity and reliability of subjective global assessment in the hemodialysis population. J Ren Nutr 2007; 17: 336–342.
- Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Ad Hoc Espen Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003; 22: 321–336.
- Bolayir B, Arik G, Yesil Y, Kuyumcu ME, Varan HD, Kara O, et al. Validation of Nutritional Risk Screening-2002 in a hospitalized adult population. Nutr Clin Pract 2019; 34: 297–303.
- Cuong TQ, Banks M, Hannan-Jones M, Thi Ngoc Diep D, Gallegos D. Validity, reliability and feasibility of nutrition screening tools NRS-2002 and MST administered by trained medical doctors in routine practice. Hosp Pract (1995) 2019; 47: 259–266.
- Tran QC, Banks M, Hannan-Jones M, Do TND, Gallegos D. Validity of four nutritional screening tools against subjective global assessment for inpatient adults in a low-middle income country in Asia. Eur J Clin Nutr 2018; 72: 979–985.
- Young AM, Kidston S, Banks MD, Mudge AM, Isenring EA. Malnutrition screening tools: comparison against two validated nutrition assessment methods in older medical inpatients. Nutrition 2013; 29: 101–106.
- Hormozi S, Alizadeh-Khoei M, Sharifi F, Chehrehgosha M, Esmaeili R, Rezaie-Abhari F, Aminalroaya R, Madadi Z. Validity of Malnutrition Universal Screening Tool (MUST) in geriatric patients: appropriate screening tool in hospital; MUST or full-MNA? J Aging Res Clin Pract 2019; 8: 74–79.
- Mosli MH, Albeshri MA, Alsolami AA, Addas FA, Qazli AM, Alsahafi M, et al. Arabic translation and psychometric testing of the self-screening malnutrition universal screening tool in inflammatory bowel disease patients. Saudi Med J 2019; 40: 828–835.
- Sharma Y, Thompson C, Kaambwa B, Shahi R, Miller M. Validity of the Malnutrition Universal Screening Tool (MUST) in Australian hospitalized acutely unwell elderly patients. Asia Pac J Clin Nutr 2017; 26: 994–1000.
- Lawson CS, Campbell KL, Dimakopoulos I, Dockrell ME. Assessing the validity and reliability of the MUST and MST nutrition screening tools in renal inpatients. J Ren Nutr 2012; 22: 499–506.
- Boleo-Tome C, Monteiro-Grillo I, Camilo M, Ravasco P. Validation of the Malnutrition Universal Screening Tool (MUST) in cancer. Br J Nutr 2012; 108: 343–348.
- Elia M. The “MUST” report. Nutritional screening of adults: a multidisciplinary responsibility. BAPEN 2003.
- Sealy MJ, Hass U, Ottery FD, van der Schans CP, Roodenburg JLN, Jager-Wittenaar H. Translation and cultural adaptation of the scored patient-generated subjective global sssessment: an interdisciplinary nutritional instrument appropriate for Dutch cancer patients. Cancer Nurs 2018; 41: 450–462.
- Henriksen C, Thoresen L, Fjoseide B, Lorentzen SS, Balstad TR, Ottery FD, Jager-Wittenaar H. Linguistic and content validity of the Norwegian patient-generated subjective global assessment. Clin Nutrit ESPEN 2018; 37: 178–184.
- Tsilika E, Parpa E, Panagiotou I, Roumeliotou A, Kouloulias V, Gennimata V, et al. Reliability and validity of the Greek version of Patient Generated-Subjective Global Assessment in Cancer Patients. Nutr Cancer 2015; 67: 899–905.
- Yoo SH, Oh E-G, Youn M-J. The reliability and validity of Patient-Generated Subjective Global Assessment (PG-SGA) in stroke patients. Kor J Adult Nurs 2009; 21: 559–569.
- Marshall S, Young A, Bauer J, Isenring E. Malnutrition in geriatric rehabilitation: prevalence, patient outcomes, and criterion validity of the scored Patient-Generated Subjective Global Assessment and the Mini Nutritional Assessment. J Acad Nutr Diet 2016; 116: 785–794.
- Fu ZM, Xu HX, Song CH, Li W, Guo ZQ, Lin Y et al. Validity of the Chinese Version of the Patient-Generated Subjective Global Assessment (PG-SGA) in gastric cancer patients. The Investigation on Nutrition Status and Clinical Outcome of Common Cancers (INSCOC) Group. J Nutrit Oncol 2018; 3: 182–188.
- Miranda D, Cardoso R, Gomes R, Guimaraes ICRP, Abreu DV, Godinho C et al. Undernutrition in institutionalized elderly patients with neurological diseases: comparison between different diagnostic criteria. J Nurs Home Res 2016; 2: 76–82.
- Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 2017; 36: 49–64.
- Yan Y, Wang N, Jian G, Zhang X, Wang X, Xue Q et al. Assessment of nutritional status by dual-energy X-ray absorptiometry in chronic kidney disease patients without dialysis. J Integr Nephrol Androl 2014; 1: 70–75.
- Delsoglio M, Achamrah N, Berger MM, Pichard C. Indirect calorimetry in clinical practice. J Clin Med 2019; 8.
- Kinney JM. Indirect calorimetry in malnutrition: nutritional assessment or therapeutic reference? JPEN J Parenter Enteral Nutr 1987; 11: 90S–94S.
- BAPEN. BAPEN assessment & planning. [cited 2021 Apr 20]. Available from: https://www.bapen.org.uk/resources-and-education/education-and-guidance/bapen-principles-of-good-nutritional-practice/82-nutrition-support/assessment-and-planning
- Keller U. Nutritional laboratory markers in malnutrition. J Clin Med 2019; 8: 775.
- Evans DC, Corkins MR, Malone A, Miller S, Mogensen KM, Guenter P, et al. The use of visceral proteins as nutrition markers: an ASPEN position paper. Nutr Clin Pract 2021; 36: 22–28.
Appendix 1. Search strategies used in databases for the outcome measure literature search.
- Science Direct, SAGE Journals, SCOPUS: Malnutrition OR “Nutritional deficiency” OR Undernutrition OR Undernourishment
- Web of Science: TI = (Malnutrition OR “Nutritional deficiency” OR Undernutrition OR Undernourishment)
- MEDLINE (PubMed): “Protein-Energy Malnutrition”[MeSH]
- ProQuest: MeSH (protein-energy malnutrition)
Appendix 2. Search algorithm used in databases for the outcome measure properties literature search.
- MEDLINE (PubMed): (“Mini Nutritional Assessment”) AND (psychometrics); (“Subjective global assessment”) AND (psychometrics); (“patient generated subjective global assessment”) AND (psychometrics); (“nutritional risk screening 2002”) AND (psychometrics); (“malnutrition universal screening tool”) AND (psychometrics).