ORIGINAL REPORT
ASSESSING CHANGES IN FEAR OF MOVEMENT IN PATIENTS ATTENDING CARDIAC REHABILITATION: RESPONSIVENESS OF THE TSK-NL HEART QUESTIONNAIRE
Nienke ter HOEVE*, PhD1, Paul KEESSEN*, PT, MSc2, Iris den UIJL, MSc3, Bart VISSER, PhD4, Roderik A. KRAAIJENHAGEN, MD, PhD5, Madoka SUNAMURA, MD, PhD6, Wilma J. M. Scholte OP REIMER, RN, PhD7, Corine H. M. LATOUR, RN, PhD8, Harald T. JØRSTAD, MD, PHD9 and Hendrika J. G. van den BERG-EMONS, PhD10
From the 1Capri Cardiac Rehabilitation and Department of Rehabilitation Medicine, Erasmus University Medical Centre, Rotterdam, 2Department of Cardiology, Heart Center, Amsterdam Cardiovascular Sciences, Amsterdam UMC, University of Amsterdam and Centre of Expertise Urban Vitality, Faculty of Health, Amsterdam University of Applied Sciences, Amsterdam, 3Capri Cardiac Rehabilitation, Rotterdam and Department of Rehabilitation Medicine, Erasmus University Medical Centre Rotterdam, 4Centre of Expertise Urban Vitality, Faculty of Health, Amsterdam University of Applied Sciences, 5Cardiovitaal Cardiac Rehabilitation, Amsterdam, 6Capri Cardiac Rehabilitation, Rotterdam, 7Department of Cardiology, Heart Center, Amsterdam Cardiovascular Sciences, Amsterdam UMC, University of Amsterdam, and Research Group Chronic Diseases, HU University of Applied Sciences Utrecht, Utrecht, 8Centre of Expertise Urban Vitality, Faculty of Health, Amsterdam University of Applied Sciences, 9Department of Cardiology, Heart Center, Amsterdam Cardiovascular Sciences, Amsterdam UMC, University of Amsterdam, Amsterdam and 10Department of Rehabilitation Medicine, Erasmus University Medical Centre Rotterdam, The Netherlands
*Shared authorship: these authors contributed equally.
Objectives: The primary objective was to determine the responsiveness of the Dutch version of the 13-item Tampa Scale for Kinesiophobia for cardiac patients (TSK-NL Heart). The secondary objective was to assess changes in kinesiophobia during cardiac rehabilitation.
Methods: Kinesiophobia was measured pre- and post-cardiac rehabilitation using the TSK-NL Heart questionnaire in 109 cardiac patients (61 years; 76% men). The effect size of kinesiophobia score changes was calculated for the full population. A measure that is responsive to change should produce higher effects sizes in patients in whom kinesiophobia improves. Therefore, effect sizes were also calculated for patients who did or did not improve on selected external measures. For this step, the Cardiac Anxiety Questionnaire (CAQ) and the Hospital Anxiety and Depression Scale (HADS) were completed as external measures in a subsample of 58 patients.
Results: The effect size of the TSK-NL Heart for the full study population was small (0.29). In line with the study hypothesis the effect size was higher (moderate) for patients with improved CAQ (0.52) and HADS scores (0.54). Prevalence of high kinesiophobia levels decreased from 40% pre-cardiac rehabilitation to 26% post-cardiac rehabilitation (p = 0.004).
Conclusion: The TSK-NL Heart has moderate responsiveness and can be used to measure changes in kinesiophobia. Improvements in kinesiophobia were observed during cardiac rehabilitation. Nevertheless, high levels of kinesiophobia were still highly prevalent post-cardiac rehabilitation.
LAY ABSTRACT
Fear of movement (kinesiophobia) is common in patients referred for cardiac rehabilitation. Before interventions can be designed to target kinesiophobia, the impact of current cardiac rehabilitation programmes on kinesiophobia should be studied. Kinesiophobia is measured with the Tampa Scale for kinesiophobia (TSK-Heart). In order to measure the effect of cardiac rehabilitation on kinesiophobia, the TSK-Heart should be able to detect changes in the level of kinesiophobia (responsiveness). This study determined the responsiveness of the TSK-Heart and assessed changes in the level of kinesiophobia during cardiac rehabilitation, and shows that the TSK-Heart has moderate responsiveness. In addition, it was found that the prevalence of high levels of kinesiophobia, decreased from 40% before cardiac rehabilitation to 26% after cardiac rehabilitation.
Key words: Tampa Scale for Kinesiophobia; cardiac rehabilitation; exercise; fear of movement; physical activity; cardiovascular disease; responsiveness; prediction finding.
Citation: J Rehabil Med 2022; 54: jrm00328. DOI: https://dx.doi.org/10.2340/jrm.v54.2519
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jul 28, 2022; Epub ahead of print: Aug 18, 2022; Published: Aug 26, 2022
Correspondence address: P. Keessen, Department of Cardiology, Heart Center, Amsterdam Cardiovascular Sciences, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands and Centre of Expertise Urban Vitality, Faculty of Health, Amsterdam University of Applied Sciences, PO Box: 2557, 1000CN, Amsterdam The Netherlands. E-mail: p.keessen@hva.nl
Competing interests and funding: The authors report no conflicts of interest.
This research was funded by Capri Cardiac Rehabilitation and Raak-PRO (RAAK.PRO02.083). PK’s work was funded by a personal teachers grant form the Dutch Research Council (NWO) (number 023.010.064). The funding sources had no role in the study design, collection and interpretation of data, writing of the manuscript and in the decision to submit the article for publication.
Physical activity (PA) is one of the cornerstones of prevention of cardiovascular disease (CVD) (1). Fear of movement, also known as kinesiophobia, might be associated with inadequate levels of PA (2). Kinesiophobia is present in 45% of patients after a recent CVD hospitalization (2) and in 20% of patients 3–10 months after hospital discharge (3). In addition to low levels of PA, high levels of kinesiophobia are also related to decreased muscle endurance and decreased quality of life (2).
Participation in cardiac rehabilitation (CR), including exercise and psychological interventions, has been shown to improve psychological factors, such as general anxiety and depression (4–6). Therefore, CR might also be a suitable setting for interventions targeting patients with lasting kinesiophobia. However, before interventions can be designed, the impact of current CR should be studied to determine the prevalence of high levels of kinesiophobia post-CR. Furthermore, it is unknown which clinical and demographic variables are predictive of lasting kinesiophobia and which beliefs about PA contribute to high levels of kinesiophobia post-CR. Insight into these aspects is important for the design of interventions.
The lack of data on kinesiophobia pre- and post-CR is partly due to the absence of well-validated instruments. Kinesiophobia is measured with the Tampa Scale for Kinesiophobia (TSK) (7) The TSK was originally developed for patients with musculoskeletal pain and has been shown to have good reliability and validity, and to be responsive to change in this population (7, 8). The TSK questionnaire was adapted by Back et al. for use in cardiac patients and renamed TSK-Heart (9). Although the TSK-Heart questionnaire has been validated (3, 9–11), it is not known if it is responsive to change.
The primary objective of this study was to determine the responsiveness of the Dutch version of the TSK-Heart questionnaire in a CR population. In case reasonable responsiveness was found, the secondary aims were to assess changes in kinesiophobia during CR and to explore candidate predictors (demographic and clinical variables and belief about PA) of high levels of kinesiophobia post-CR.
MATERIAL AND METHODS
Study design and participants
Patients with a variety of cardiac diagnoses referred to CR at Capri Cardiac Rehabilitation (Rotterdam, the Netherlands) or Cardiovitaal Cardiac Rehabilitation (Amsterdam, the Netherlands) between July 2018 and February 2019 were invited to participate in this longitudinal prospective cohort study. The majority of patients are referred to CR within 1–3 months after a cardiac event. Inclusion criteria were: age >18 years, proficiency in Dutch and access to e-mail. A waiver of approval was granted by the Medical Ethics Committee of Erasmus University Medical Centre, Rotterdam, the Netherlands (MEC-2017-1096). All patients provided informed consent. To assure methodological quality the box Responsiveness (construct approach) of the COSMIN checklist (COnsensus-based Standards for the selection of health status Measurement INstruments) was used to design this study (see Appendix I) (12). The current study aimed to include a minimum of 150 participants to determine both validity (see previous publication (3)) and responsiveness. According to the COSMIN Checklist, a minimum of 50 patients is considered adequate, and a minimum of 100 patients is seen as good to determine responsiveness using a construct approach (12).
Cardiac rehabilitation programme
All patients were enrolled in a multidisciplinary CR programme based on European and Dutch guidelines (13, 14). The programme comprised 2 training sessions per week (aerobic and strength exercises) for a duration of 6–12 weeks. Educational sessions were offered on cardiovascular risk factors, healthy lifestyles and emotional coping. All sessions lasted for approximately 1 h. Based on individual goals, patients could participate in individual or group counselling sessions focused on healthy diet, smoking cessation and stress management. If needed, patients were referred to a psychologist for additional psychological support. CR was ended when individual goals were met or after consultation between patient and the multidisciplinary CR team.
Data collection
Kinesiophobia. Kinesiophobia was measured with the Dutch version of the 13-item Tampa Scale for Kinesiophobia for cardiac patients (TSK-NL Heart) (3). The outcome is a score between 13 and 52. A cut-off score of 29 or higher was used to define high levels of kinesiophobia (3). In addition to the total score, a sum score was calculated for each of the 3 subscales of the TSK-NL Heart: (1) fear of injury (sum score between 8 and 32 of items 1, 2, 3, 5, 6, 7, 9, and 12); (2) perception of risk (sum score between 2 and 8 of items 4 and 10); and (3) avoidance of PA (sum score between 3 and 12 of items 8, 11, and 13).
External measures. Since a gold standard for determining kinesiophobia is lacking, the current study used a construct approach (12) with an external criterion. As external criteria 2 measurement tools were used, which are often used to determine anxiety in CR: (i) Cardiac Anxiety Questionnaire (CAQ) (15) and (ii) Hospital Anxiety and Depression Scale (HADS) (16). Our previously conducted cross-sectional study found the TSK-NL Heart to be strongly correlated with the CAQ and HADS (3). The CAQ measures cardiac anxiety, which can be defined as “anxiety symptoms that are triggered by specific cardiac-related stimuli and symptoms” (15). The outcome is a score between 0 and 72. The HADS consists of 2 subscales to measure generic anxiety (HADS-A) and general depression (HADS-D) (16). For the purposes of this study, only the HADS-A was used. The outcome is a score between 0 and 21.
Procedure. Data on age, sex, cardiac diagnoses, type of intervention, history of cardiac disease and comorbidities were obtained from medical charts. Patients were asked to complete the TSK-NL Heart, CAQ and HADS-A online, at home, 1 week before the start of CR (pre-CR). At 3 months follow up (post-CR), patients were asked to complete the TSK-NL Heart again. To determine external responsiveness, only a subsample of the patients (only patients receiving CR at the location in Rotterdam) received the CAQ and HADS for a second time.
Statistical methods
Patient selection and characteristics. Patient characteristics are presented as means and standard deviations (SD) for normally distributed data, and as medians and interquartile ranges (IQR) for non-normally distributed data. Normality was checked using a Kolmogorov–Smirnov test. Categorical data are presented as percentages. To evaluate potential bias, differences in baseline characteristics between patients included and excluded from analysis were evaluated using an independent samples t-test, Mann–Whitney U test or χ2 test, as appropriate. In case of missing items within a questionnaire, a maximum of 2 items were imputed with the median score on the other items of the same patient (17).
Responsiveness. Internal responsiveness was estimated by calculating the effect size (ES, (change score/SD of pre-CR score)) and standardized response mean (SRM, (change score/SD of change score)) of the change in the total score in the full study population. For both the ES and SRM, a score ≤ 0.49 was considered small, 0.50–0.79 as moderate and ≥ 0.80 as large (18). Since ES and SRM are based on parametric distributions, the TSK scores pre-CR and post-CR will be assessed using paired samples t-test (parametric distribution) and Wilcoxon signed-rank test (non-parametric distribution). If similar results are yielded from both tests, the ES and SRM can be interpreted safely. Since substantial improvements in TSK-NL Heart scores are expected in only a subsample of patients entering CR with high kinesiophobia scores (3), and since specific kinesiophobia interventions are lacking during CR, no large treatment effect was anticipated. Therefore, the current study anticipated finding small to moderate ES and SRM values for the full study population. A measure that is responsive to change should be able to distinguish between subgroups of patients who do or do not show changes. Higher ES and SRM values are therefore expected in a subsample of patients who show improvements on the external measures (CAQ and HADS-A). Therefore, external responsiveness was determined by calculating ES and SRM values for subsamples of patients who showed improvements (change score > 0) on the external measures and for patients whose scores did not improve (change score ≤ 0). We defined the responsiveness of TSK-NL Heart to be reasonable in case the ES and SRM values were at least moderate for the subsample that improved on the external measures and small for the group that did not improve.
External responsiveness was further explored using Spearman’s correlation coefficients between change scores on the TSK-NL Heart and change scores on the external measures (CAQ and HADS-A). A correlation coefficient ≤ 0.29 was considered a poor correlation, 0.30–0.49 a moderate correlation, and ≥ 0.5 a strong correlation (19). Since all 3 questionnaires measure anxiety, we anticipated a correlation between the change scores (3). Nevertheless, since the TSK-NL Heart measures a specific anxiety (movement-related), we did not expect to find a strong correlation.
Changes in kinesiophobia and predictor finding analysis. The non-normally distributed TSK-NL Heart, HADS-A and CAQ mean score changes, between pre-CR and post-CR, were tested with a Wilcoxon signed-rank test. Pre-CR scores and post-CR scores were presented with amplitude probability distribution function (APDF) plots (3). For the original TSK, one study reports a change of 5.5 points, on a 13-item scale, as clinically relevant, while another study reports a change of 4.5, on a 17-item scale, as clinically relevant (8, 20). For the purpose of this study, the number of patients showing an improvement of at least 5 points on the TSK-NL Heart was calculated.
For the predictor finding analysis (21), univariate logistic regression analysis was performed with the dichotomized TSK-NL Heart score (scores ≥ 29 vs score < 29) as dependent variable and baseline characteristics (age, sex, diagnosis and type of intervention) and pre-CR scores on the TSK-NL Heart (total score and scores on subscales), CAQ and HADS- A as predictor variables.
For all tests SPSS version 26 (IBM Crop, Amonk, USA) was used. A p-value < 0.05 was considered significant.
RESULTS
Methodological quality
All 10 items of the COSMIN criteria checklist were completed (see Appendix I). Nine items were scored as “very good” and 1 was scored “adequate”.
Participants
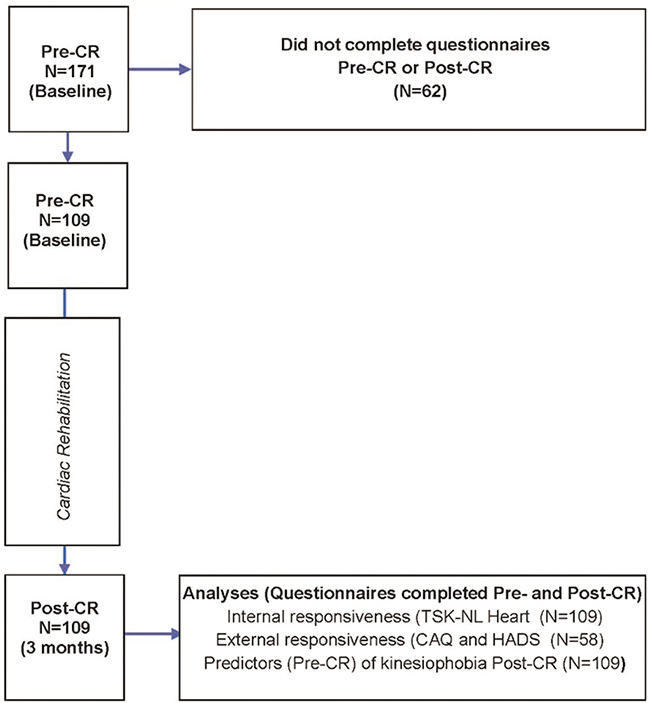
A total of 171 patients participated in this study. Of these, 109 patients (61 years old, 76.1% male) completed the TSK-NL Heart both pre-CR and post-CR and were included in the analysis (Fig. 1, Table I). The majority of patients were referred to CR after an acute event (52.3%), such as a myocardial infarction. Details regarding cardiac diagnosis can be found in Table I. A history of cardiac disease was present in 23.9% of patients. Included patients were more often men (76.1% vs 61.3%; p = 0.04), had lower levels of kinesiophobia (median TSK-NL Heart score (IQR) score of 26 (11) vs 29.5 (14); p = 0.03) and had less generic anxiety (median HADS-A score (IQR) score of 5 (5.5) vs 6.0 (7.0); p = 0.02) compared with patients excluded due to incomplete TSK-NL Heart questionnaires.
The external measures (HADS-A and CAQ) were completed post-CR in only 1 of the participating centres. Therefore, external responsiveness could only be determined within this subsample consisting of 58 patients. There were no baseline differences observed between the sample included for the internal responsiveness (n = 109) and external responsiveness (n = 58).
Responsiveness
The parametric and non-parametric distributions of the TSK-NL Heart were assessed prior to investigating the ES and SRM. Both the paired samples t-test and Wilcoxon signed-rank test yielded similar results (paired samples t-test: mean (SD) TSK NL Heart: pre-CR: 26.11 (7.20) and post-CR: 24.03 (7.41), p < 0.001) (Wilcoxon signed-rank test: median (IQR) TSK NL Heart pre-CR: 26.0 (11) and post-CR: 23.0 (11), p < 0.001), indicating that the assessment of ES and SRM is justified. Both the ES of the change score (0.29) and the SRM of the change score (0.37) were small. There was a moderate and significant correlation between change scores on the TSK-NL Heart and the CAQ (Rs = 0.30, p = 0.02). There was a poor and non-significant correlation between change scores on the TSK-NL Heart and the HADS-A (Rs = 0.21, p = 0.11). Based on the CAQ, 44 patients were classified as improved, while 13 patients did not improve (see Table II). Both the ES and the SRM of the TSK-NL Heart change score were moderate for patients with an improved CAQ score (ES = 0.52; SRM = 0.57) and small for patients with no improvement (ES = 0; SRM = 0). Based on the HADS-A, 29 patients were classified as improved, while 29 patients did not improve (see Table II). In line with the CAQ, both the SRM and the ES of TSK-NL Heart change score were moderate for patients with an improved HADS-A score (ES = 0.54; SRM = 0.60) and small for patients who did not improve (ES = 0.26; SRM = 0.36).
| Group of patients | Pre-CR TSK score | Post-CR TSK score | ∆TSK score | p-value* | Effect size | Standardized response mean |
| Median (IQR) | Median (IQR) | Median (IQR) | (ES) | (SRM) | ||
| Internal responsiveness | ||||||
| Total sample (n=109) | 26.0 (11.0) | 23.0 (11.0) | –2.0 (8.0) | <0.001 | 0.29 | 0.37 |
| External responsiveness | ||||||
| Total sample that completed CAQ (n = 57) | 25.0 (10.5) | 23.0 (10.5) | –2.0 (7.0) | 0.002 | 0.37 | 0.46 |
| Improved on CAQ (n = 44) | 25.0 (10.0) | 23.0 (10.5) | –4.0 (7.0) | 0.001 | 0.52 | 0.57 |
| Not improved on CAQ (n = 13) | 21.0 (15.0) | 22.0 (16.0) | 0.0 (4.0) | 0.88 | 0 | 0 |
| Total sample that completed HADS-A (n = 58) | 25.0 (10.5) | 23.0 (10.3) | –2.5 (7.0) | 0.001 | 0.39 | 0.48 |
| Improved on HADS-A (n = 29) | 25.0 (10.0) | 22.0 (9.5) | –4.0 (8.5) | 0.005 | 0.54 | 0.60 |
| Not improved on HADS-A (n = 29) | 22.0 (12.5) | 24.0 (10.5) | –2.0 (6.5) | 0.08 | 0.26 | 0.36 |
| IQR: interquartile range; TSK: Tampa Scale for Kinesiophobia; CAQ: Cardiac Anxiety Questionnaire; HADS-A: Hospital and Anxiety Questionnaire-Anxiety Scale | ||||||
| *Wilcoxon signed-rank test to compare pre-CR and post-CR TSK scores. | ||||||
Changes in kinesiophobia and predictors for high levels of kinesiophobia post-CR
Since moderate ES and SRM values were found in the subsample that improved on the external measures, we determined the responsiveness of the TSK-NL Heart to be reasonable and we proceeded with our secondary aims. Total score on the TSK-NL Heart improved from a median score (IQR) of 26.0 (11.0) pre-CR to 23.0 (11.0) post-CR (p < 0.001) (Fig. 2, Table II). A total of 31.2% of patients showed an improvement of at least 5 points on the TSK-NL Heart. Prevalence of a high level of kinesiophobia (TSK-NL Heart score ≥ 29) was seen in 40.4% pre-CR and improved to 25.7% post-CR (p = 0.004).
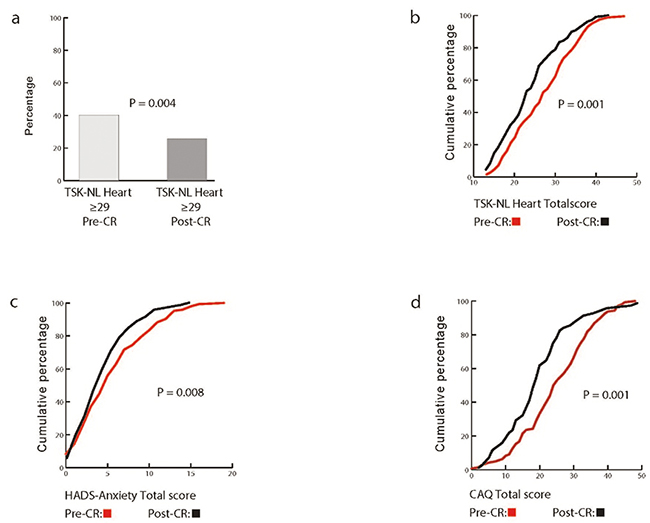
Fig. 2. Total scores of the TSK, HADS-A and CAQ pre-CR and post-CR. (a) Histogram high levels of kinesiophobia (TSK-NL Heart) pre-cardiac rehabilitation (CR) and post-CR (McNemar test). (b,c,d) Amplitude Probability Distribution Function (ADPF) of (c) HADS-A, (b) TSK-NL Heart and (d) CAQ sumscores pre-CR and post-CR (Wilcoxon signed-rank test).
Patients with a high level of kinesiophobia pre-CR were more likely to have high levels of kinesiophobia post-CR (OR = 9.83, 95% CI = 3.52–27.46). Additional univariate regression analyses revealed that the odds of having high kinesiophobia levels post-CR were also higher when having a higher baseline score on the CAQ (OR = 1.12, 95% CI = 1.06–1.19) and HADS-A (OR = 1.26, 95% CI = 1.11–1.42). Furthermore, high scores pre-CR on all TSK subscales (reflecting beliefs that contribute to kinesiophobia) were related to high levels of kinesiophobia post-CR, especially pre-CR score on the subscale “Avoidance of PA” (OR = 1.95, 95% CI = 1.44–2.65) (see Table III).
| Predictor | Low TSK score (< 29), n = 81 | High TSK score (≥ 29), n = 28 | OR high TSK score post-CR | 95 % CI | p-value |
| Sex, n (%) | |||||
| Male | 61 (75.3) | 22 (78.6) | ref | ||
| Female | 20 (24.7) | 6 (21.4) | 0.83 | 0.30–2.35 | 0.73 |
| Age, mean (SD) | 61.7 (11.6) | 59.3 (11.6) | 0.98 | 0.95–1.02 | 0.35 |
| Admission, n (%) | |||||
| Elective | 38 (46.9) | 14 (50) | ref | ||
| Acute | 43 (53.1) | 14 (50) | 0.88 | 0.37–2.09 | 0.78 |
| Procedure, n (%) | |||||
| Medication | 13 (16.1) | 6 (22.2) | ref | ||
| Surgical | 29 (35.8) | 7 (25.9) | 0.52 | 0.15–1.87 | 0.32 |
| Interventional | 39 (48.1) | 14 (51.9) | 0.78 | 0.25–2.44 | 0.67 |
| High TSK score pre-CR, n (%) | |||||
| Low | 59 (72.8) | 6 (21.4) | ref | ||
| High | 22 (27.2) | 22 (78.6) | 9.83 | 3.52–27.46 | < 0.001 |
| TSK total score Pre-CR, median (IQR) | 23.0 (10.0) | 32.0 (7.7) | 1.24 | 1.13–1.36 | < 0.001 |
| TSK Fear of injury Pre-CR, median (IQR) | 15.0 (8.0) | 21.5 (5.0) | 1.28 | 1.14–1.44 | < 0.001 |
| TSK Perception of risk-Pre CR, median (IQR) | 4.0 (2.0) | 5.0 (2.0) | 1.82 | 1.23–2.70 | 0.003 |
| TSK Avoidance of PA-Pre-CR, median (IQR) | 5.0 (3.0) | 6.5 (2.0) | 1.95 | 1.44–2.65 | < 0.001 |
| CAQ score pre-CR, median (IQR)1 | 21.0 (16.0) | 32.5 (15.5) | 1.12 | 1.06–1.19 | < 0.001 |
| HADS-A score pre-CR, median (IQR)2 | 3.0 (3.0) | 7.5 (4.5) | 1.26 | 1.11–1.42 | < 0.001 |
| 1Data missing for n = 13; 2Data missing for n = 12. | |||||
| ref: reference category; SD: standard deviation; IQR: interquartile range; TSK: Tampa Scale for Kinesiophobia; PA: physical activity, CAQ: Cardiac Anxiety Questionnaire; HADS: Hospital and Anxiety Scale. | |||||
DISCUSSION
In line with the study hypothesis, small ES and SRM values were found for the TSK-NL Heart change scores in the full study population and higher (moderate) ES and SRM values in a subsample of patients who showed improvements on the external measures. These results suggest that the TSK-NL Heart has reasonable responsiveness in patients completing CR. The current outcomes reveal that at the start of CR, 40% of patients had high levels of kinesiophobia, which decreased to 26% post-CR.
The original TSK was developed for patients with low back pain (8, 20, 22–24) Internal responsiveness in our full study population (ES: 0.29; SRM: 0.37) was low when compared with that in patients with chronic low back pain participating in a rehabilitation programme (ES 1.36; SRM 1.49) (8). Values of the ES and SRM depend on the expected magnitude of the treatment effect. Despite the fact that targeting kinesiophobia is an objective of CR, no specific treatment strategies for kinesiophobia are currently used in CR. In addition, only a subsample of patients who enter CR have high levels of kinesiophobia (3) Therefore, substantial reductions in TSK-NL Heart scores are not expected for the whole population. Consequently, low ES and SRM were anticipated. By including this heterogeneous population, we were able to determine whether the TSK-NL heart is able to distinguish between subgroups of patients who do or do not show changes in kinesiophobia. We did indeed find that ES and SRM values improved from small to moderate for patients who improved on the CAQ and for patients who improved on the HADS-A compared with patients who did not improve on these external measures. Furthermore, a moderate significant correlation was found between the change scores on the TSK-NL Heart and CAQ, while the correlation between the change scores on the TSK-NL Heart and the HADS-A was non-significant. An explanation for this finding might be that the TSK-NL Heart and CAQ both measure specific cardiac-related fear, while the HADS-A measures generic anxiety.
Overall, the study outcomes indicate that the TSK-NL Heart has moderate responsiveness. The authors recommend further research into the responsiveness of the TSK-NL Heart in larger sample sizes using anchor-based methods to confirm the current results. Using anchor-based methods also allows for research into the minimal clinical important change (MCIC). The MCIC cannot be determined with a construct approach as used in our study. Therefore, it can be debated whether the improvement of 2 points we found on the TSK-NL Heart score is clinically relevant. Nevertheless, 31% of patients showed an improvement of at least 5 points on the TSK-NL Heart, which was previously suggested to be a clinically relevant change in other patient populations (8, 20). Furthermore, an improvement was seen in the percentage of patients scoring above the threshold for high kinesiophobia scores from 40% to 26%. Altogether, this indicates that relevant improvements are made during CR.
Regardless of attendance at CR, a large number of patients (26%) still had high levels of kinesiophobia on the long term. Before designing interventions, it is of value to understand which patients should be targeted. The results of our univariate logistic regression analysis with a limited number of baseline characteristics suggest that high kinesiophobia scores post-CR are independent of sex, age, diagnosis (acute vs elective) and type of intervention, but may be predicted by high kinesiophobia and generic anxiety scores at the start of CR. In line with our findings, a high level of generic anxiety (HADS-A) has been shown to be a predictor for kinesiophobia in a previous study with patients with CVD (2), while sex and medical background did not predict kinesiophobia (25, 26). In addition, the current results also show that high scores on the sub-scales of the TSK-NL Heart were all predictive of high levels of kinesiophobia post-CR. Especially high scores on the subscale “avoidance of PA” increased the risk of high levels of kinesiophobia post-CR. A recent qualitative study shows that avoidance of PA is often the result of negative beliefs and attitudes towards PA (27).
The outcomes of the current study can assist clinicians in determining who could potentially benefit from additional interventions and can also help in designing these interventions. Nevertheless, before these interventions are developed, future studies should first investigate how kinesiophobia relates to PA in cardiac patients. Furthermore, future studies should investigate a larger set of potential predictors (e.g. time since cardiac event and specific diagnosis categories) in a larger study population.
Study limitations
To our knowledge this is the first study to evaluate the responsiveness of the TSK for cardiac patients. Nevertheless, some aspects of the current study warrant consideration. First, patients who were excluded from the current analysis (patients who did not complete the TSK-NL Heart post-CR) had lower TSK-NL Heart scores, which might limit generalizability. Although we could not investigate the subjects’ reasons for not completing the questionnaire, we hypothesize that this was mainly due to not completing the CR programme. This suggests that patients with higher kinesiophobia levels might quit CR prematurely more often than patients with lower levels. Secondly, univariate logistic regression analyses were used to assess a limited number of demographic and clinical variables as predictors of kinesiophobia post-CR. The results of this analysis should be interpreted with caution, as the sample size was restricted. Nevertheless, both the external anxiety measures and the kinesiophobia score at the start of CR all significantly predict high levels of kinesiophobia post CR at the level of p < 0.001. Finally, this study did not include a control group of patients not participating in CR. Therefore, caution is required when attributing the improvements found in kinesiophobia to CR.
CONCLUSION
The outcomes indicate that, in patients attending CR, TSK-NL Heart has moderate responsiveness and can be seen as a candidate measurement tool to evaluate changes in kinesiophobia. In addition, outcomes demonstrate improvements in kinesiophobia levels after completion of CR. Nevertheless, a considerable proportion of patients (26%) retain high levels of kinesiophobia after completion of CR, warranting further investigations and the development of treatment strategies.
ACKNOWLEDGEMENTS
The authors thank participating patients and personnel of Capri Cardiac Rehabilitation and Cardiovitaal Cardiac Rehabilitation who supported the inclusion of patients and data collection.
REFERENCES
- Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane Systematic review and meta-analysis. J Am Coll Cardiol 2016; 67: 1–12.
- Back M, Cider A, Herlitz J, Lundberg M, Jansson B. The impact on kinesiophobia (fear of movement) by clinical variables for patients with coronary artery disease. Int J Cardiol 2013; 167: 391–397.
- Keessen P, den Uijl I, Visser B, van den Berg-Emons H, Latour CHM, Sunamura M, et al. Fear of movement in patients attending cardiac rehabilitation: a validation study. J Rehabil Med 2020; 52: jrm00021.
- Lavie CJ, Menezes AR, De Schutter A, Milani RV, Blumenthal JA. Impact of cardiac rehabilitation and exercise training on psychological risk factors and subsequent prognosis in patients with cardiovascular disease. Can J Cardiol 2016; 32: S365–S373.
- Lavie CJ, Milani RV, O’Keefe JH, Lavie TJ. Impact of exercise training on psychological risk factors. Prog Cardiovasc Dis 2011; 53: 464–470.
- Whalley B, Rees K, Davies P, Bennett P, Ebrahim S, Liu Z, et al. Psychological interventions for coronary heart disease. The Cochrane database of systematic reviews 2011; 10.1002/14651858.CD002902.pub3: CD002902.
- Vlaeyen JW, Kole-Snijders AM, Rotteveel AM, Ruesink R, Heuts PH. The role of fear of movement/(re)injury in pain disability. J Occupat Rehabil 1995; 5: 235–252.
- Monticone M, Ambrosini E, Rocca B, Foti C, Ferrante S. Responsiveness of the Tampa Scale of Kinesiophobia in Italian subjects with chronic low back pain undergoing motor and cognitive rehabilitation. Eur Spine J 2016; 25: 2882–2888.
- Back M, Jansson B, Cider A, Herlitz J, Lundberg M. Validation of a questionnaire to detect kinesiophobia (fear of movement) in patients with coronary artery disease. J Rehabil Med 2012; 44: 363–369.
- Ghisi GLM, dos Santos RZ, Felipe TR, Bonin CDB, Fonseca-Pinto E, Fernandes Guera FE, et al. Validation of the portuguese version of the Tampa Scale for Kinesiophobia Heart (TSK-SV heart). Rev Bras Med Esporte 2017; 23.
- Acar S, Savci S, Keskinoglu P, Akdeniz B, Ozpelit E, Ozcan Kahraman B, et al. Tampa Scale of Kinesiophobia for Heart Turkish Version Study: cross-cultural adaptation, exploratory factor analysis, and reliability. J Pain Res 2016; 9: 445–451.
- Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 2010; 10: 22.
- Ambrosetti M, Abreu A, Corra U, Davos CH, Hansen D, Frederix I, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol 2020; 10.1177/2047487320913379.
- Multidisciplinaire Richtlijn Hartrevalidatie 2011. Utrecht: Revalidatiecommissie NVVC / NHS, 2011.
- van Beek MH, Voshaar RC, van Deelen FM, van Balkom AJ, Pop G, Speckens AE. The cardiac anxiety questionnaire: cross-validation among cardiac inpatients. Int J Psychiatry Med 2012; 43: 349–364.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52: 69–77.
- Streiner DL, Norman GR. Health measurement scales. 4th edn. Oxford: Oxford University Press; 2008.
- Middel B, van Sonderen E. Statistical significant change versus relevant or important change in (quasi) experimental design: some conceptual and methodological problems in estimating magnitude of intervention-related change in health services research. Int J Integr Care 2002; 2: e15.
- Field A. Discovering statistics using SPSS. 3rd edn. Los Angeles: Sage; 2009.
- Haugen AJ, Grovle L, Keller A, Grotle M. Cross-cultural adaptation and validation of the Norwegian version of the Tampa Scale for Kinesiophobia. Spine (Phila Pa 1976) 2008; 33: E595–601.
- Bouwmeester W, Zuithoff NP, Mallett S, Geerlings MI, Vergouwe Y, Steyerberg EW, et al. Reporting and methods in clinical prediction research: a systematic review. PLoS Med 2012; 9: 1–12.
- Pulles A, Koke AJA, Strackke RP, Smeets R. The responsiveness and interpretability of psychosocial patient-reported outcome measures in chronic musculoskeletal pain rehabilitation. Eur J Pain 2020; 24: 134–144.
- Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain 2005; 117: 137–144.
- de Souza FS, Marinho Cda S, Siqueira FB, Maher CG, Costa LO. Psychometric testing confirms that the Brazilian-Portuguese adaptations, the original versions of the Fear-Avoidance Beliefs Questionnaire, and the Tampa Scale of Kinesiophobia have similar measurement properties. Spine (Phila Pa 1976) 2008; 33: 1028–1033.
- Knapik A, Dabek J, Brzek A. Kinesiophobia as a problem in adherence to physical activity recommendations in elderly Polish patients with coronary artery disease. Patient Prefer Adherence 2019; 13: 2129–2135.
- Brunetti ND, Guerra A, Ieva R, Correale M, Santoro F, Tarantino N, et al. Scared for the scar: fearsome impact of acute cardiovascular disease on perceived kinesiophobia (fear of movement). Clin Cardiol 2017; 40: 480–484.
- Keessen P, Latour CHM, van Duijvenbode ICD, Visser B, Proosdij A, Reen D, et al. Factors related to fear of movement after acute cardiac hospitalization. BMC Cardiovasc Disord 2020; 20: 495.