ORIGINAL REPORT
COMPARISON OF QUADRICEPS AND HAMSTRING MUSCLE STRENGTH AFTER EXERCISES WITH AND WITHOUT BLOOD FLOW RESTRICTION FOLLOWING ANTERIOR CRUCIATE LIGAMENT SURGERY: A RANDOMIZED CONTROLLED TRIAL
Rafael Francisco Vieira DE MELO, MSc1, William Ricardo KOMATSU, PhD1, Mellissa Sales DE FREITAS, MD1, Maria Eduarda Vieira DE MELO, Medical Student2, Moises COHEN, PhD1
From the 1Universidade Federal de São Paulo, São Paulo and 2Universidade Católica de Pernambuco, Recife, Brazil
Background: Muscle mass loss occurs following anterior cruciate ligament reconstruction surgery.
Objective: To compare the gain in muscle strength in the quadriceps and hamstring muscles in patients following anterior cruciate ligament reconstruction surgery, using exercises with and without blood flow restriction.
Methods: This is a randomized controlled trial, in which 50% (n = 14) of the participants were allocated to the intervention group and the remaining 50% (n = 14) to the control group. The study included the participation of postoperative patients, with reconstruction of the anterior cruciate ligament.
Results: After comparing the rehabilitation of the groups, a statistical difference was observed in the quadriceps with an increase in muscle strength (p < 0.01) after 12 weeks and an increase in muscle strength hamstrings (p < 0.01) after 8 and 12 weeks in the injured legs of the intervention group compared to the control. In the analysis of the participants' physical function, there was an significant increase difference in the Lysholm questionnaire (p < 0.01) after 8 and 12 weeks, in the KOOS pain questionnaire (p < 0.01) after 4 weeks a decrease was observed, symptoms and daily activities (p < 0.01) after 8 and 12 weeks, quality of life (p < 0.01) after 12 weeks, and in the IKDC questionnaire (p < 0.01) after 8 and 12 weeks there was an significant increase difference of the intervention group compared to the control.
Conclusion: After anterior cruciate ligament surgery, exercises with blood flow restriction proved more efficient for improving the muscle strength of the quadriceps and hamstrings, and the physical function of the knee than the same exercises without blood flow restriction.
LAY ABSTRACT
After anterior cruciate ligament reconstruction surgery patients need to undergo a gradual process of rehabilitation. This prospective study compared muscle strength gain between exercises with and without blood flow restriction (BFR) in the quadriceps and hamstring muscles. Regarding knee extension, there was an improvement in muscle strength after 12 weeks in the injured legs. For knee flexion an improvement was observed at 8 weeks, in addition to improvement in functionality. The use of blood flow restriction in rehabilitation exercises after anterior cruciate ligament reconstruction was shown to be more efficient for muscle strength gain in the quadriceps and hamstrings and improvement in knee physical function.
Key words: anterior cruciate ligament; rehabilitation; exercise therapy; physical therapy specialty; exercise; blood flow restriction.
Citation: J Rehabil Med 2022; 54: jrm00337. DOI: https://doi.org/10.2340/jrm.v54.2550
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Sep 8, 2022; Epub ahead of print: Oct 3, 2022; Published: Nov 1, 2022
Correspondence address: Rafael Francisco Vieira de Melo, Avenida Onze de Junho, 1425, apto: 21, Edf: Iguaçu. 04041-054. São Paulo, Brazil. E-mail: melorfv@gmail.com
Competing interests and funding: The authors have no conflicts of interest to declare.
Not applicable.
Delayed rehabilitation after leg trauma and surgeries, such as anterior cruciate ligament (ACL) reconstruction, leads to deficits in muscle strength and endurance, due to muscle atrophy and arthrogenic inhibition, contributing to alteration of the movement patterns of the involved limb and therefore increasing the risk of early onset of knee osteoarthritis (1, 2).
Decrease in strength due to disuse of the thigh muscles is considered important, since rehabilitation usually takes a prolonged period of time to regain the original muscle strength, compromising the function of the lower limbs and the patient’s quality of life. Weakness of the knee muscles is present during the first 12 weeks following surgery, impairing lower limb function and quality of life. This is also affected by contributing mechanisms, such as neural inhibition, which, in turn, is caused partly by pain and swelling. Thus, it induces chronic muscle weakness, which is linked to decreased function and injuries (3).
A few studies and protocols have addressed on the adequacy of rehabilitation of quadriceps and hamstring muscle strength after ACL reconstruction (ACLR) to preoperative strength levels, thus attenuating muscle atrophy following ACLR, through the use of exercises with blood flow restriction (BFR) at 20–30% of maximum strength (3, 4). This occlusion is known to minimize the risk of injury because the exercises are performed with low load, ensuring joint and graft safety and contributing to postoperative strengthening (3, 4).
However, the effect of BFR on other important aspects in ACLR rehabilitation, such as physical function and pain, has not been studied. Also, the effectiveness of BFR for stimulating muscle strength and hypertrophy during rehabilitation after ACLR has not been directly compared with high-load exercises in the preoperative period with follow-up in the first 3 months (5–9).
Therefore, the aim of the current study is to evaluate the intensity of muscle strength gain, comparing BFR with low-intensity exercise or high-intensity exercise without occlusion in the quadriceps and hamstring muscles in the ACLR postoperative period.
METHODS
Study type
The Consolidated Standards of Reporting Trials (CONSORT) guideline and flowchart for randomized clinical trials (RCTs) was followed in conducting this study (10). This is a randomized clinical trial, prospective, longitudinal, parallel, analytical, and experimental. Random allocation was performed to assign 50% of the participants to an intervention group and 50% to a control group. The study included the participation of post-operated patients, with ACLR using a hamstring autograft.
Participants
Men and women with ACL rupture confirmed by medical examination in the last 2 months and planned reconstructive surgery, aged between 18 and 59 years, were included in the study. Exclusion criteria were: new injury or reconstruction of the ACL due to laxity in the involved limb during rehabilitation, patients who needed additional surgical procedures after reconstruction of the ACL, or infections in the operated region. Patients with previous surgeries on the injured knee, or injury to another knee ligament or meniscus were not included. Participants were recruited from the Cohen Institute of Orthopedics, Rehabilitation and Sports Medicine and underwent rehabilitation training at the same location (São Paulo, Brazil).
Randomization and allocation
For allocation into groups, randomization was performed in blocks. For each participant a number was generated by computer through the website https://www.random.org/sequences/, where the smallest value was 1 and the largest 28. The hidden allocation format was automatically generated through the website, divided into 2 columns: the first, control group and the second, intervention group.
Interventions
The experimental protocol is shown in Fig. 1, followed by the description of each step of the study.
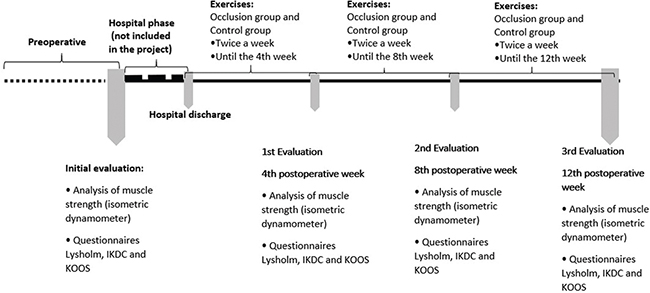
Fig. 1. Overview of the experimental study protocol. KOOS: Knee Injury and Osteoarthritis Outcome Score; IKDC: International Knee Documentation Committee.
The intervention group used pressure gauges measuring 10 × 80 cm in width and a 7 × 52 cm pneumatic bag (Cuff Scientific Leg® – WCS, Curitiba, Paraná, Brazil) in the region close to the inguinal ligament of the right and left leg. The control group performed the same proposed exercises without any occlusion material.
To determine the vascular occlusion pressure a portable vascular Doppler device (ICC = 0.795) (DV-610B®; MEDMEGA, Franca, São Paulo, Brazil) was used. The patient rested for 15 min in neutral supine position before the procedure. After resting, the blood flow over the posterior tibial artery was captured using a portable vascular Doppler pen with an infrared signal transducer, with the aid of a gel. The cuff with a pneumatic bag was then inflated at the lowest pressure until the arterial pulse was no longer detected, and the pulse was measured until total occlusion was reached (approximately 15 s). At this time, the pressure value marked on the manometer represented the total occlusion pressure, after this the cuff was deflated. This measurement was repeated with all participants in order to customize the training according to the pressure of each participant, thus ensuring patient safety (11, 12). During training, 80% of the total occlusion pressure was used following recommended guideline protocol and previous studies (12, 13). The maximum load tests (1RM) were performed through maximum repetitions in the leg press and flexor chair exercises for training with BFR. The repetitions and load (submaximal) performed in the exercise were applied using the formula: 1RM = submaximal load/100% – (2 × number of repetitions%). The injured limb was trained first, and then the uninjured limb matched the repetitions, each with a relative percentage of its 1RM, to equalize the volume and external load and thus control for any cross-transfer effects of training from the limbs. Blood flow restriction was applied to both limbs for this reason. The training load was increased by 10% if participants completed all repetitions in 2 subsequent sessions or on the last training day of the 4th, 8th, and 12th weeks. Exercise volume (kg) was calculated as: number of repetitions × load (kg). For each selected exercise, 30% of a repetition maximum (RM) was used in the intervention group and 70% of 1RM in the control group.
Leg press. Seated patients performed hip and knee flexion-extension, the injured limb was trained first, then the control limb matched the repetitions, each with a relative percentage of its 1RM (intervention group with BFR: 1 × 30 repetitions and 3 × 15 repetitions and control group without occlusion: 3 × 10 repetitions).
Flexor chair. Seated patients performed knee flexion-extension, the injured limb was trained first, then the control limb matched the repetitions, each with a relative percentage of its 1RM (intervention group with BFR: 1 × 30 repetitions and 3 × 15 repetitions and control group without occlusion: 3 × 10 repetitions).
In exercises with BFR, 4 sets were performed, the first always of 30 repetitions, followed by 3 further sets of 15 repetitions each, with 2 s for concentric contraction and 2 s for eccentric contraction. The rest time in each series was 30 s, measured on a digital clock. The pressure was maintained during the performance of all sets of exercise. If necessary, the pressure was adjusted at intervals of sets, after the end of the exercise. Sometimes there was a small leakage of air during the movement, hence inflating the cuff a little more to leave it at the pre-established pressure was necessary. In this way, a light touch just to maintain the air in the cuff is ideal so that there is no change in pressure. Between each exercise block, the BFR was released for 5 min, to normalize the blood flow in that region and therefore ensure reperfusion (13). The training frequency was twice a week for 12 weeks. When the patient could not perform the full movement of 1 repetition due to fatigue, the exercise was stopped. The control group performed the same exercises, with 70% of 1RM, with 3 sets of 10 repetitions, with all other parameters, but without BFR. The adherence of the research subjects was registered on an attendance list.
Outcomes
The primary outcome was assessment of muscle strength using an isometric dynamometer on the first day of assessment and repeated on the last training day of the 4th, 8th and 12th weeks; these evaluations were always performed on a day separate from the physical training. The maximum isometric strength of the knee extensors and flexors in both legs was measured using the MICROFET2® digital handheld dynamometer (Hoggan Health Industries, West Jordan, UT, USA). The maximum force was recorded in Newtons (N) and collected 3 times in each leg. Between each contraction there were 60-s intervals. Participants were instructed to remain seated in a very erect position on a chair with their arms crossed in front of their chests and their legs hanging over the edge, with knees and hips flexed at 90°. To measure the quadriceps through isometric knee extension, the dynamometer was positioned in the anterior region of the tibia and secured with an inelastic band, in a location identical to the location used in isokinetic dynamometers (5 cm proximal to the lateral malleolus), generating stabilization and resistance against movement during the test. To assess the strength of the hamstrings for isometric knee flexion, the dynamometer was attached to the sural triceps region (5 cm proximal to the lateral malleolus), and to a table located in front of the participant by an inelastic strap. A demonstration was performed to familiarize the patient with the device before measurements for isometric knee extension and flexion strength began to be collected. Each participant was instructed to perform maximal isometric contractions for 5 s and the maximal strength was recorded.
The secondary outcomes were to analyse physical function of the knee using the Lysholm, International Knee Documentation Committee (IKDC) and Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaires. All questionnaires were completed by the patient in order to reduce application bias on the first day of assessment and repeated on the last training day of the 4th, 8th and 12th week.
Sample size
A pilot study was conducted, on a small scale, with the same objectives, procedures, materials and methods proposed in the research. Thus, a total of 24 patients was needed, 12 per group. Therefore, to represent a dropout rate of up to 10%, a total of 28 patients was recruited, 14 in each group.
Sample size calculation was performed using the G*power® 3.1.9.2 Software (Heinrich-Heine-Universität, Düsseldorf, Germany), based on the effect size for muscle strength with BFR and HL reported in a meta-analysis (7), to achieve a statistical power of 95% and α = 0.05. Therefore, stipulating a total of 24 patients, 12 in each group. However, a total of 28 patients were recruited, considering an abstinence rate of at least 10%.
Statistical analysis
Descriptive data analysis was performed and expressed as mean and standard deviation (SD). To verify possible differences in the sampling characteristics (age, weight, height, body mass index and sex) between the 2 groups, analysis of variance (ANOVA) with Greenhouse-Geisser adjustment was used.
Data normality and homogeneity were tested using the Shapiro–Wilk and Levene tests, respectively, verifying that the sample did not follow a Gaussian distribution, as well as the homogeneity was violeted. To analyse the effect of training with vascular occlusion, the generalized linear model of generalized estimating equations (GEE) statistical test was used, in which the independent factor was group allocation (control or intervention) and time (weeks 0, 4, 8 and 12), dependent factor. Effect size was described using Cohen’s D as small if 0.20 – 0.30, medium if 0.40 – 0.70, and large if greater than or equal to 0.807 (7).
RESULTS
The flow of participants is shown in Fig. 2, followed by a description of each step of the study.
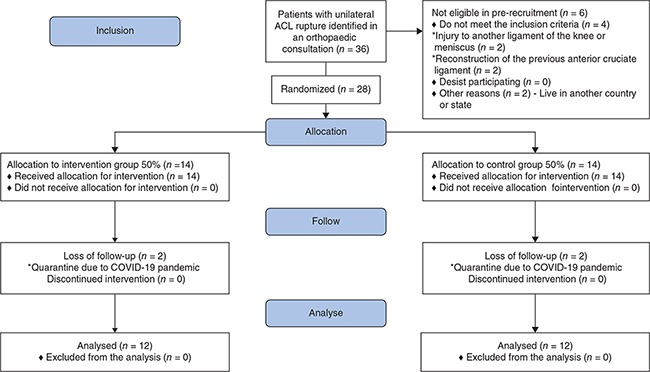
Fig. 2. Overview of study flowchart. ACL: anterior cruciate ligament.
Data regarding the sample characterization of both groups is shown in Table I.
In the injured leg, both groups showed an increase in strength for the extension movement throughout the training cycle, but from the third post-surgical period, the intervention group had a greater gain in the flexion movement (Fig. 3). As for the flexion movement, both groups showed an increase in strength throughout the training cycle, but from the second post-surgical period onwards there was a greater gain in the intervention group (Fig. 3).
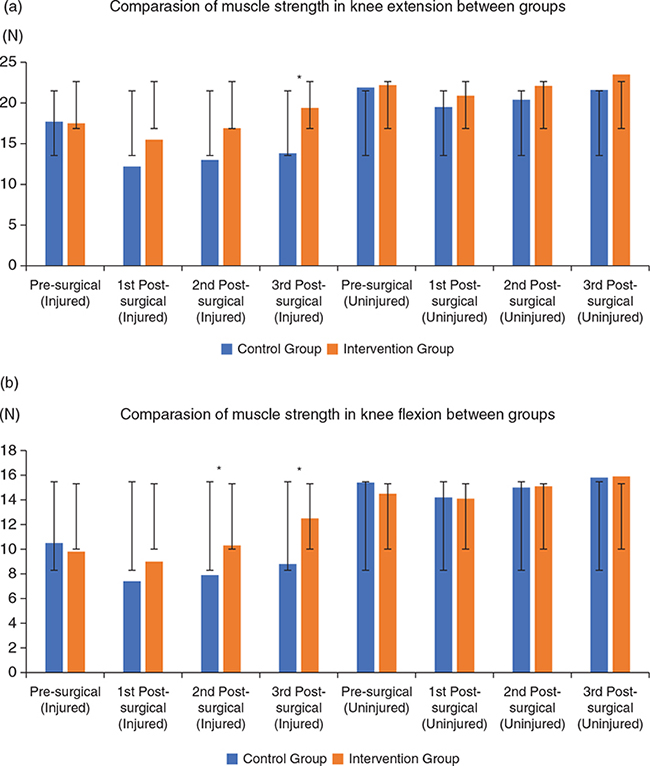
Fig. 3. Representation of the comparison of muscle strength in knee extension (a) and flexion (b) between groups.
N = Newton; *p < 0.01.
In all groups, an increase in self-reported scores was observed throughout the rehabilitation period, with the intervention group showing better scores from the 1st post-surgical period for Knee Injury and Osteoarthritis Outcome Score (KOOS) subscale (Pain) and, from the 2nd post-surgical period, for all other scales (Table II).
DISCUSSION
In the postoperative phase of training, there is a progressive load on the operated limb. Thus, the advantages of BFR over resistance training without occlusion reside in the fact that it can initially allow for greater pain reduction, with subsequent improvement in patients’ physical function and quality of life, to a higher degree compared with resistance training without occlusion (3). These benefits are achieved without any detrimental effect on strength, including greater strength gains compared with groups that perform conventional physical therapy rehabilitation, as observed in the current study.
| Questionnaires | Groups | Preoperative week mean difference (95% CI) | ES | Mean difference week 1st post-surgery (95% CI) | ES | Mean difference 2nd week after surgery (95% CI) | ES | Mean difference week 3rd Post-surgery (95% CI) | ES | p-valor |
| Lysholm | Control | 81.17 ± 6.23 (69.84 – 94.84) | 0.21 | 81.75 ± 3.80 (74.64 – 89.54) | 0.87 | 86.17 ± 1.95 (82.43 – 90.07) * | 2,72 | 90,58 ± 0,84(88,96 – 92,24) | 4,31 | < 0,01* |
| Intervention | 85.17 ± 3.97 (77.74 – 93.31) | 92.00 ± 2.39 (87.43 – 96.80) | 100.00 ± 0 (100.00 – 100.00) # | 100,00 ± 0(100,00 – 100,00) # | ||||||
| KOOS Symptoms | Control | 81.67 ± 6.26 (70.27 – 94.91) | 0.39 | 80.42 ± 4.53 (72.01 – 89.80) | 0.97 | 85.25 ± 2.28 (80.89 – 89.85) | 2,07 | 91,92 ± 0,88(90,21 – 93,65) | 3,53 | < 0,01* |
| Intervention | 88.42 ± 1.64 (85.25 – 91.70) | 92.42 ± 1.29 (89.92 – 94.99)* | 98.58 ± 0.93 (96.77 – 100.43) # | 100,00 ± 0(100,00 – 100,00) # | ||||||
| Pain | Control | 84.75 ± 4.67 (76.07 – 94.42)* | 0.01 | 70.67 ± 3.30 (64.49 – 77.43)* | 1.66 | 76.92 ± 3.94 (67.57 – 85.05)* | 2,18 | 88,00 ± 2,35(83,52 – 92,72) | 1,96 | < 0,01* |
| Intervention | 84.50 ± 3.33 (78.22 – 91.29)* | 90.58 ± 3.20 (84.52 – 97.09)* | 99.50 ± 0.48 (98.57 – 100.44)* # | 100,00 ± 0(100,00 – 100,00) *# | ||||||
| Daily activity | Control | 86.92 ± 4.44 (75.64 – 93.10)* | 0.03 | 78.83 ± 3.72 (71.37 – 85.97) | 0.76 | 80.58 ± 3.99 (73.12 – 88.81) | 1,53 | 87,50 ± 2,00(83,67 – 91,51) | 2,38 | < 0,01* |
| Intervention | 83.42 ± 3.37 (77.07 – 90.29) | 86.67 ± 1.93 (82.97 – 90.53)* | 97.00 ± 0.98 (95.10 – 98.94) *# | 99,92 ± 0,08(99,76 – 100,07*# | ||||||
| Quality of life | Control | 66.42 ± 4.99 (57.32 – 76.96)* | 0.12 | 62.25 ± 4.54 (53.96 – 71.82) | 0.81 | 65.17 ± 4.08 (57.63 – 73.68) | 1,29 | 69,92 ± 3,04(64,20 – 76,15) | 1,72 | < 0,01* |
| Intervention | 64.33 ± 4.03(56.89 – 72.75)* | 72.58 ± 1.82 (69.10 – 76.25)* | 79.75 ± 1.43 (77.00 – 82.60)* | 83,92 ± 0,69(82,57 – 85,28) * | ||||||
| IKDC | Control | 57.67 ± 3.06 (51.97 – 63.99)* | 0.22 | 51.58 ± 2.02 (47.77 – 55.70)* | 1.014 | 55.00 ± 1.60 (51.95 – 58.23) | 2,34 | 60,92 ± 1,59(57,88 – 64,12) | 3,23 | < 0,01* |
| Intervention | 59.67 ± 1.65 (56.52 – 62.98) | 58.25 ± 1.50 (55.38 – 61.27) | 65.08 ± 0.38 (64.34 – 65.83) *# | 74,83 ± 0,44(73,98 – 75,70) *# | ||||||
| KOOS: Knee Injury and Osteoarthritis Outcome Score; IKDC: International Knee Documentation Committee; ES: Cohen’s d effect size; *Significant difference p < 0.05; #Significant difference in relation to control. | ||||||||||
Thus, resistance exercises with occlusion lead to increased strength and muscle growth by reducing the supply of oxygen to the muscle, inducing muscle hypoxia, releasing some growth factors. Metabolic stress and the accumulation of substances in the environment seem to be responsible for the increase in the secretion of growth hormone (GH), which is a precursor of Insuline like growth factor (IGF-1), which is responsible for protein synthesis, increasing muscle trophism, cross-sectional area and force. As well as myostatin inhibition and increased heat shock proteins.
Regarding knee extension, this study observed that, before surgery, there were no differences between the groups of patients. After comparing the rehabilitation groups, a greater statistical difference was observed in quadriceps muscle strength (p < 0.01) after 12 weeks of training in the group with BFR; findings similar to those in the study by Hughes et al. (3), although he achieved a significant difference in quadriceps muscle strength in a unilateral leg press (p < 0.01) after 8 weeks. In the current study in the fourth and eighth weeks there were progressive improvements, but these were not significant. Regarding the uninjured leg, there were no differences in any period.
In addition to evaluating the isometric muscle strength of the quadriceps, this study was the first to test the isometric muscle strength of the hamstrings using a portable dynamometer preoperatively and immediately after ACLR: at 4, 8 and 12 weeks. It was possible to observe in the intervention group and in the control group, but the group that used BFR and lower training load showed a significantly greater improvement in muscle strength in a shorter rehabilitation period than the group in which the rehabilitation exercises were performed with a greater load.
The hamstrings may have been stronger than the quadriceps muscle after ACLR due to the greater arthrogenic muscle inhibition of the quadriceps, decreasing sensory reception and information sent to the frontal cortex. This is commonly observed in the first days of the post-surgery period, as the ligament makes this connection between the peripheral nervous system and the central nervous system.
Another associated issue that may have contributed to the early strengthening of the hamstrings is the fact that patients could have used the posterior leg muscles in the exercise leg press, using contractions together with the quadriceps, performing movement compensation during execution, even with all the execution guidelines and correct positioning on the device. In addition, we subsequently train later on the flexor chair, with a muscle isolation contraction, which further increases the strength of this musculature. Future studies are needed to analyse this aspect using electromyography in this initial phase of post-surgical training. There were no significant differences in strength in the uninjured legs.
In order to promote the patients’ well-being we used validated functionality questionnaires used previously in other research on the same topic. The use of the isometric dynamometer ensured, in a validated way, as observed in previous studies (14–17), the assessment of muscle strength for knee extension and flexion in early rehabilitation with practical execution and data analysis. Thus, any major strains on the knee that could be caused by an isokinetic dynamometer were avoided, in addition to the lower cost and ease of transport when comparing the 2 devices.
As in other studies (3, 18, 19), the current study applied the technique of BFR individually, ensuring safety for all patients and respecting their individual differences. Safety in the current study was obtained through the use of portable Doppler ultrasound in all patients, offering 80% occlusion during individual training. Use of a handheld Doppler ensures that the pulse and/or blood flow is still present in each participant and provides an affordable and valid alternative to the “gold standard” (Doppler ultrasound) in determining arterial resting occlusion pressure level. It can be used in clinical settings to determine arterial occlusion pressure level in order to provide a safe and relative stimulus during patient rehabilitation protocols (11, 12).
The current study used a consistent protocol, with low loads, consistent training and 80% precise occlusion pressure in the intervention group during all sessions. In exercises with BFR, 4 sets were performed, the first always of 30 repetitions, followed by 3 more sets of 15 repetitions each. Similar applicability used in other studies (3, 18). The protocol used in this study reflect current guidelines for training with BFR (1, 3, 5, 18, 21), in addition to proposed objectives for the best possible rehabilitation after ACLR.
Regarding the pre-surgical questionnaires (22, 23, 24), there were no differences between the patient groups. In the first evaluation, the only statistical difference was in the KOOS questionnaire in the pain subtopic (p < 0.01) after 4 weeks in the group that trained with BFR and with low load. This data revealed a key factor for the patients to be able to progress subsequently in all other items evaluated during the treatment, possibly due to the comfort and security they felt with the low load during the execution of the movements and the muscle strengthening of the region promoted by the occlusion. The KOOS questionnaire in the subtopics symptoms and daily activities showed significant improvements (p < 0.01) after 8 and 12 weeks and quality of life (p < 0.01) after 12 weeks, where the answers involved many behavioural psychological questions and not just motor ones. The IKDC questionnaire showed statistical differences (p < 0.01) after 8 and 12 weeks. Similar results were seen with the Lysholm questionnaire, which obtained a significant difference (p < 0.01) after 8 and 12 weeks, demonstrating the importance of pain improvement for early gain in strength and physical function.
This study observed that the application of BFR in the early postoperative phase is beneficial in terms of muscle strength and physical function of patients. During this period, high-intensity exercise is not possible and the benefits of metabolic stress on protein synthesis can be activated. Thus, training with BFR can be a preparatory approach and used prior to high-intensity resistance exercises, especially in the presence of pain or when high loads are not tolerated/allowed (3, 18, 25).
We suggest that, in clinical practice, the use of BFR with low loads should be integrated with exercises with higher loads in more advanced stages of rehabilitation in an intercalated way, as this may stimulate other important musculoskeletal adaptations during treatment after ACLR.
No adverse effects, such as deep vein thrombosis, skin lesions, haematomas or any damage, occurred in any patient during the study. However, during the initial training, subjects reported discomfort with the technique due to compression in the inguinal region, fatigue during exercises, and hyperaemia in the thigh due to the increased blood supply to the region; findings that improved a few seconds after removal of the occlusion. This was due to the novelty of training with BFR associated with oedema in the knee region, which is considered normal after the recent surgical procedure, promoting such sensations. Similar findings were also described previously (3, 18, 24), suggesting that the light load associated with BFR in the early post-surgical phase may not exacerbate pain or inflammation in the knee joint in the days following training, which may positively influence the volume of exercise during sessions and patient adherence to a rehabilitation programme. Thus, it was observed in the current sample that early reduced pain plays a fundamental role in the patient’s functionality and quality of life.
Further studies, with larger sample sizes, specific groups of grafts, ages and in a multicentric design, are needed to increase the scope of these findings.
Study limitations
The current study has some limitations. Participants could not be blinded due to the intervention model using the cuffs. The study also has a relatively short follow-up time, but was performed during the period in which patients could undergo the best benefits from the application of the technique, which is during this initial post-surgical phase. The sample was relatively small, but sufficient according to the sample size calculation, and randomization ensured sample homogeneity.
CONCLUSION
Comparing training in an early rehabilitation programme after ACLR, using 30% of 1RM with BFR or 70% of maximum repetition without occlusion, the group that used BFR showed a statistically more rapid gain in improvement in quadriceps and hamstrings muscle strength, and physical function of the knee.
ACKNOWLEDGEMENTS
The authors acknowledge the Federal University of São Paulo for the opportunity to study in an environment of excellence. We thank all the employees of the university (the library, reception, secretariat, security, cafeteria, maintenance and cleaning assistants) who have always been very kind.
Ethics approval and consent to participate
The study was submitted for evaluation by the ethics committee of the Federal University of São Paulo and started after approval (Project CEP/UNIFESP n: 0507/2019; CAAE: 12902219.4.0000.5505). Designed by the World Health Organization, its Universal Evaluation Number (UTN): U1111-1242-8567 in 31/10/2019 and also submitted to the Brazilian Registry of Clinical Trials with approval opinion: RBR-9bdgxh in 28 January 2020. The recruitment of participants was conducted after approval by the ethics committee in January 2020 until May 2020. All patients signed a written informed consent form prior to the start of the study.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analysed during the current study are available in the REDCap repository (https://redcap.epm.br/redcap_v12.2.2/index.php?pid=2250).
Authors’ contributions
Melo RFV: investigation, methodology, project administration, supervision, validation, visualization, writing-original draft, writing-review and editing; Cohen M: supervisor; Komatsu WR: supervise; Freitas MS: data curation, formal analysis; Melo MEV: writing – review and editing.
REFERENCES
- Žargi T, Drobnič M, Stražar K, Kacin A. Short-term preconditioning with blood flow restricted exercise preserves quadriceps muscle endurance in patients after anterior cruciate ligament reconstruction. Front Physiol 2018; 9: 1150.
- Sonnery-Cottet B, Saithna A, Quelard B, Daggett M, Borade A, Ouanezar H, Thaunat M, Blakeney WG. Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Br J Sports Med 2019; 53 (5): 289–298.
- Hughes L, Rosenblatt B, Haddad F, Gissane C, McCarthy D, Clarke T, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service randomised controlled trial. Sports Med 2019; 49 (11): 1787–1805.
- Iversen E, Røstad V, Larmo A. Intermittent blood flow restriction does not reduce atrophy following anterior cruciate ligament reconstruction. J Sport Health Sci 2016; 5 (1): 115–118.
- Lipker LA, Persinger CR, Michalko BS, Durall CJ. Blood flow restriction therapy versus standard care for reducing quadriceps atrophy after anterior cruciate ligament reconstruction. J Sport Rehabil 2019; 28 (8): 897–901.
- Barber-Westin S, Noyes FR. Blood flow-restricted training for lower extremity muscle weakness due to knee pathology: a systematic review. Sports Health 2019; 11 (1): 69–83.
- Lixandrão ME, Ugrinowitsch C, Berton R, Vechin FC, Conceição MS, Damas F, et al. Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med 2018; 48 (2): 361–378.
- Nascimento DDC, Petriz B, Oliveira SDC, Vieira DCL, Funghetto SS, Silva AO, et al. Effects of blood flow restriction exercise on hemostasis: a systematic review of randomized and non-randomized trials. Int J Gen Med 2019; 12: 91–100.
- Schoenfeld BJ, Grgic J, Krieger J. How many times per week should a muscle be trained to maximize muscle hypertrophy? A systematic review and meta-analysis of studies examining the effects of resistance training frequency. J Sports Sci 2019; 37(11): 1286–1295.
- Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010; 23: 332–340.
- Laurentino GC, Ugrinowitsch C, Roschel H, Aoki MS, Soares AG, Neves M Jr, et al. Strength training with blood flow restriction diminishes myostatin gene expression. Med Sci Sports Exerc 2012; 44 (3): 406–412.
- Laurentino GC, Loenneke JP, Mouser JG, Buckner SL, Counts BR, Dankel SJ, et al. Validity of the handheld Doppler to determine lower-limb blood flow restriction pressure for exercise protocols. J Strength Cond Res 2020; 34 (9): 2693–2696.
- Patterson SD, Hughes L, Warmington S, Burr J, Scott BR, Owens J, et al. Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol 2019; 15: 510–533.
- Lesnak J, Anderson D, Farmer B, Katsavelis D, Grindstaff TL. Validity of hand-held dynamometry in measuring quadriceps streght and rate of torque development. Int J Sports Phys Ther 2019; 14 (2):180–187.
- Almeida GPL, Albano TR, Melo AKP. Hand-held dynamometer identifies asymmetries in torque of the quadriceps muscle after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2019; 27 (8): 2494–2501.
- Hansen EM, McCartney CN, Sweeney RS, Palimenio MR, Grindstaff TL. Hand-held dynamometer positioning impacts discomfort during quadriceps strength testing: a validity and reliability study. Int J Sports Phys Ther 2015; 10 (1): 62–68.
- Koblbauer IF, Lambrecht Y, van der Hulst ML, Neeter C, Engelbert RH, Poolman RW, et al. Reliability of maximal isometric knee strength testing with modified hand-held dynamometry in patients awaiting total knee arthroplasty: useful in research and individual patient settings? A reliability study. BMC Musculoskelet Disord 2011; 31: 212–249.
- Hughes L, Paton B, Haddad F, Rosenblatt B, Gissane C, Patterson SD. Comparison of the acute perceptual and blood pressure response to heavy load and light load blood flow restriction resistance exercise in anterior cruciate ligament reconstruction patients and non-injured populations. Phys Ther Sport 2018; 33: 54–61.
- Curran MT, Bedi A, Mendias CL, Wojtys EM, Kujawa MV, Palmieri-Smith RM. Blood flow restriction training applied with high-intensity exercise does not improve quadriceps muscle function after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med 2020; 48 (4): 825–837.
- Giles L, Webster KE, McClelland J, Cook JL. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. Br J Sports Med 2017; 51 (23): 1688–1694.
- Tennent DJ, Hylden CM, Johnson AE, Burns TC, Wilken JM, Owens JG. Blood flow restriction training after knee arthroscopy: a randomized controlled pilot study. Clin J Sport Med 2017; 27 (3): 245–252.
- Metsavaht L, Leporace G, Riberto M, de Mello Sposito MM, Batista LA. Translation and cross-cultural adaptation of the Brazilian version of the International Knee Documentation Committee Subjective Knee Form: validity and reproducibility. Am J Sports Med 2010; 38 (9): 1894–1899.
- Peccin MS, Ciconelli R, Cohen, M. Questionário específico para sintomas do joelho “Lysholm Knee Scoring Scale”: translation and validation into Portuguese. Acta Ortop Bras 2006; 14 (5): 268–272.
- Gonçalves RS, Cabri J, Pinheiro JP, Ferreira PL. Cross-cultural adaptation and validation of the Portuguese version of the Knee injury and Osteoarthritis Outcome Score (KOOS). Osteoarthrit Cartil 2009; 17 (9): 1156–1162.
- Ohta H, Kurosawa H, Ikeda H, Iwase Y, Satou N, Nakamura S. Low-load resistance muscle training with moderate restriction of blood flow after anterior cruciate ligament reconstruction. Acta Orthop Scand 2003; 74 (1): 62–68.
- Kilgas MA, Lytle LLM, Drum SN, Elmer SJ. Exercise with blood flow restriction to improve quadriceps function long after ACL reconstruction. Int J Sports Med 2019; 40 (10): 650–656.