ORIGINAL REPORT
RETURNING TO WORK AFTER STROKE: ASSOCIATIONS WITH COGNITIVE PERFORMANCE, MOTIVATION, PERCEIVED WORKING ABILITY AND BARRIERS
Katri SAAR, Master of Psychology1, Asko TOLVANEN, Doctor of Philosophy (Psychology)2, Erja POUTIAINEN, Doctor of Philosophy (Psychology)3 and Tuija ARO, Doctor of Philosophy (Psychology)2
From the 1South Savo Social and Health Care and Authority, Suojelius Oy, Espoo, 2Department of Psychology, University of Jyväskylä, Jyväskylä and 3Rehabilitation Foundation, Helsinki, Finland
Objective: To investigate post-stroke return-to-work and its associations with cognitive performance, motivation, perceived working ability, and self-perceived barriers to returning to work.
Design: Prospective cohort study of a clinical sample.
Subjects and methods: Participants were 77 stroke patients younger than age 69 years. Assessment included a cognitive screening method for stroke patients (CoMet), a questionnaire regarding work-related matters, and a question regarding motivation to return to work. A predictive model of return-to-work was built, and how participants managed in their working life was examined.
Results: Cognitive performance was significantly connected with returning to work. Three of the 5 individuals who dropped out of working life had cognitive dysfunction. Cognitive performance predicted 80% of those who had not returned and 37% of those who had returned by 6 months after the initial assessment. Self-perceived working ability and barriers predicted 64% of those who had not returned and 78% of those who had returned at the 12-month follow-up.
Conclusion: Cognitive performance seems to be a crucial predictor of return-to-work post-stroke, but individuals’ own evaluations of their working capabilities are also important.
LAY ABSTRACT
Returning to work after stroke is important for stroke patients’ participation in society. This study investigated return-to-work among stroke patients and its association with cognitive skills, motivation, and patients’ self-perceived abilities and barriers concerning returning to work. Cognitive skills were connected to returning to work and predicted returning for a 6-month period. Patients’ self-perceived abilities and barriers predicted returning to work by 12 months after stroke. These findings indicate that cognitive skills have an important role in returning to working life after stroke, but patients’ own evaluations of their capabilities are also important. This study may provide information for better rehabilitation planning after stroke and help rehabilitation professionals to consider the patients’ views of their capabilities.
Key words: stroke; return-to-work; cognitive performance; self-perceived working ability.
Citation: J Rehabil Med 2023; 55: jrm00365. DOI: https://dx.doi.org/10.2340/jrm.v55.2576
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Nov 18, 2022; Published: Jan 9, 2023
Correspondence address: Katri Saar, South Savo Social and Health Care and Authority, Suojelius Oy/Katri Saar, Juvanpuistonkuja 2 A 1, 02920 Espoo, Finland. E-mail: psykologipalvelu@live.fi
Competing interests and funding: The authors have no conflicts of interest to declare.
The authors thank the University of Jyväskylä for funding this article.
Stroke was ranked, in 2010, as the third most common cause of disability-adjusted life years worldwide (1). Approximately 1 in 4 individuals with stroke are under the age of 65 years (2, 3) and encounter challenges related to work life (4).
A systematic review at Edwards et al. (5) found that rates of post-stroke return-to-work varied from 7.3% to 74.5% between studies and increased over time. On average, 41% of subjects returned to work between 0 and 6 months and 53% at 1 year. Work can be seen as a key to participation in society and to a sense of competence (6) and returning to work can be viewed as an important indicator of recovery following stroke (7).
Previous studies have shown that the major cause of unsuccessful return-to-work post-stroke is impaired cognitive ability (8, 9) and other hidden impairments, such as fatigue (10, 11), as well as motor impairments (12). In addition, stroke severity (13, 14) and younger age (15, 16) have a significant influence on returning to work. Furthermore, white-collar workers are more likely to return to work (9, 17), although blue-collar workers tend to return earlier (18). Tanaka et al. (17) found that secure employment status at the time of stroke may enhance the likelihood of returning to work after stroke.
There is a paucity of studies analysing the impact of motivation and self-perceived facilitators of and barriers to return-to-work after stroke, and diverse factors have not been studied in concert. In the current study, both cognitive and non-cognitive factors associated with return-to-work after stroke were scrutinized.
In addition to returning to work, remaining at work should also be considered (19), as some of the stroke patients drop out of work after some time (9). Individuals may experience several difficulties in staying at work and being able to retain their jobs, such as understanding of hidden impairments, lack of support, severity of impairment, and indirect issues, such as not being able to drive (10). Stroke survivors may return to the workforce too early and leave when difficulties are realized in practice, causing disappointment, frustration, and consequent individual suffering (9, 19).
The aim of this study was to investigate the association between cognitive performance and return-to-work after stroke, in concert with motivational factors, perceived working ability, and barriers to work, as well as demographic factors. Post-stroke coping in working life was also investigated by studying potential drop-outs from work by individuals in a follow-up period of 6 months to 2 years after stroke. The specific research questions were:
- Do the participant’s demographic characteristics (occupational status, education level, sex, and age), motivation, self-perceived working ability, self-perceived barriers to returning to work, and cognitive performance have an association with stroke patients’ return-to-work by 6 or 12 months after stroke? To what extent can returning to work be predicted by these factors?
- Do drop-outs from work occur during the 24-month period after stroke, and do demographic characteristics or cognitive performance contribute to drop-out?
METHODS
Participants and procedure
Participants were 77 individuals attending a 3-day post-stroke assessment at the Kruunupuisto Punkaharju Rehabilitation Center in Savonlinna. They had been referred by the hospital’s project coordinator at 2 weeks to 2 months (mean 51 days) after stroke. The assessment included a cognitive screening method for stroke patients (CoMet). Participants were under 69 years of age (mean 53 years, standard deviation (SD) 6.9, range 34–64 years, 73% male) and were working at the time of stroke. Participants had an opportunity to return to their previous work after sick leave, and 74 had held a full-time job prior to the stroke. Educational levels (in years) were as follows: <10 years (16%), 10–15 years (61%), and >15 years (23%). Diagnostic brain imaging was used to confirm the stroke. Patients with severe stroke-related disabilities were excluded from the study due to the unlikeliness of their return to work in the follow-up period. Neurologists evaluated each patient’s fitness for the research project using the following exclusion criteria: serious degenerative illnesses, transient ischaemic attack (TIA), multiple sclerosis, Parkinson’s disease, central nervous system infection, severe brain injury, acute cancer treatment, hip replacement or exoskeleton operation within 2 months, severe depression, psychotic disorder, or alcohol or psychoactive drug addiction. Aetiological information was as follows: infarct (73%), intracerebral hemorrhage (ICH) (17%), subarachnoid hemorrhage (SAV) (8%), and other (3%). Participants’ functional status was measured with the Barthel Index (mean 97, SD 9). The prevalence of language problems, including aphasia, was 23% (Number of participants 18).
The first follow-up assessment was conducted at 6 months after the initial assessment and included a phone interview. Four male participants had dropped out of the study by the first follow-up assessment. The mean age of subjects participating in the 6 month follow-up was 53 (SD = 7), and 71% were male. The occupational status of 2 of the drop-outs was white-collar and, of the other 2, blue-collar.
The second follow-up assessment, at 12 months after the initial assessment, included working status information and a questionnaire on work-related matters (21). By the 12-month follow-up, 9 additional participants had dropped out of the study. The mean age of participants attending the 12 months follow-up was 52 (SD = 7), and 66% were male. Two of the drop-outs had occupational statuses as entrepreneurs, 2 were white-collar workers, and 5 were blue-collar workers.
The working status information was obtained from a subsample of 44 participants (mean age 52 years, SD 7 years, 68% male) 24 months after stroke (Fig. 1).
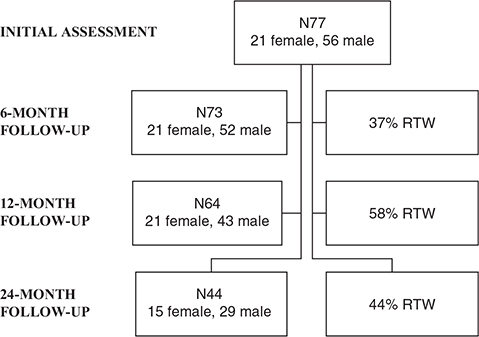
Fig. 1. Participants and return-to-work (RTW) information.
Assessments were conducted at the Kruunupuisto Punkaharju Rehabilitation Center from 2012–15. Participants gave written informed consent before participating. The Research Ethics Committee of the Southern Savo Hospital District approved the study and consent procedure (registration number 93//2011).
Measures
Initial assessment 2 weeks to 2 months after stroke.
- Occupational status and educational level. Occupational status was divided into 3 categories: 1: white-collar workers; 2: blue-collar workers; and 3: entrepreneurs. Educational level was defined as 4 categories: 1: comprehensive school/middle school/civic school; 2: vocational school/high school; 3: university of applied sciences degree; and 4: university degree.
- Cognitive screening method for stroke patients (CoMet) (20). The CoMet consists of 11 subtests that assess orientation, language, visual processing, memory, attention, working memory, processing speed, and executive function-based cognitive functions (Table I). Saar et al. (20) validated the CoMet total score with a clinical neuropsychological assessment and discovered that the best balances of sensitivity (88%) and specificity (50%) were obtained with a cut-off point of 138. Scores lower than 138 indicate cognitive dysfunction. The total score was used in the current study.
- Questionnaire on work-related matters. This comprised 12 parts from the Work Ability Index (21). Self-perceived working ability and self-perceived barriers were evaluated using 4 parts of the questionnaire on work-related matters.
- Perceived working ability. Self-perceived working ability was assessed by 3 questions: 1: “Evaluate your working ability by scoring from 1 to 10, where 10 describes your working ability when at the best possible level”; 2: “Evaluate your working ability in terms of physical demands”; and 3: “Evaluate your working ability in terms of mental demands.” A Likert scale (1 = very poor, 5 = very good) was used when answering questions 2 and 3. All questions were analysed separately.
- Perceived barriers to returning to work. Self-perceived barriers to returning to work were evaluated with 6 questions covering diverse areas of possible barriers: “Do you have problems with the following issues concerning your ability or strength to carry on in your duties: (a) issues concerning your health or functional ability, (b) lack of education or know-how, (c) problems concerning physical load in your duties or working environment, (d) mental stress in the work or in the work community, (e) lack of motivation or willingness to work, (f) problems outside of work (in family, financial situation, etc.)?” The participants answered all items using the following scale: 1: “No harmful effects”; 2: “A few harmful effects”; 3: “Many harmful effects”; and 4: “Can’t tell.” The results for the participants who chose “Can’t tell” were excluded from the particular analyses. The questions were analysed both separately and by forming a sum score.
| CoMet | ||
| I | Orientation | Six orientative questions |
| II | a. Writing sentences b. Instruction understanding |
Writing a sentence from a model and making up another sentence Drawing following 5 instructions |
| III | Word fluency | Naming animals in 1 min |
| IV | Episodic memory | Recalling a story |
| V | Drawing | Drawing 2 pictures from a model |
| VI | Delayed episodic memory | Recalling a story |
| VII | a. Object naming b. Object memory |
Naming 10 objects from the picture Recalling 10 objects |
| VIII | Sentence repetition | Repeating a sentence read by the researcher |
| IX | a. Object replacing b. Object recognition |
Recalling 10 objects and placing them in the right spot Recognizing 10 objects among other objects |
| X | Visual finding | Finding a target symbol among different symbols as quickly as possible |
| XI | Number arranging | Arranging 12 numbers in descending order as quickly as possible |
| XII | Self-evaluation | Subject’s self-evaluation of CoMet performance |
Six-month follow-up.
- Motivation. Motivation to return to work was assessed during a phone interview. Participants were guided to answer with dichotomous alternatives, and the answers were registered dichotomously (motivation/no motivation).
- Working status. Current working status was surveyed during the phone interview as follows: returning to previous work as full-time or part-time; work try-out; on sickness leave; retired; and other. Full-time or part-time work was regarded as returning to work.
Twelve-month follow-up.
- Working status. Information on working status was gathered as in the 6-month follow-up assessment.
- Questionnaire on work-related matters. Perceived working ability and perceived barriers to returning to work were assessed by the questionnaire on work-related matters, as in the initial assessment.
Twenty-four-month follow-up.
- Working status. Information on working status was gathered as in the 6-month follow-up assessment.
Data analysis
First, a correlation analysis (Spearman’s rho) was used to answer the first research question (i.e. to investigate whether age, sex, education level, cognitive performance evaluated with the cognitive screening test, motivation, self-perceived working ability, or self-perceived barriers to return-to-work were associated with return-to-work at 6 and 12 months). An independent samples t-test was used to compare the CoMet mean differences between the groups that returned and did not return to work at 6 and 12 months after stroke. Cross-tabulation and a χ2 test were used to investigate if the premorbid occupational status had an association with returning to work 6 or 12 months after stroke. Logistic regression analysis was then used to predict returning to work; however, only variables showing significant correlations with returning to work were included in the model. Variables from initial assessment were used to predict returning to work at 6 months follow-up. Returning to work at the 12-month follow-up was predicted with variables measured at the 6-month follow-up. Perceived barriers to returning to work at the 6-month follow-up were analysed with a sum score. The best predictive model was chosen using backward elimination (Wald).
Next, the demographic information (sex and age), working statuses, and cognitive profiles of the participants who returned to work once but later dropped out were examined with a closer inspection at the 24-month follow-up. The data were analysed with SPSS 26.0, and the significance level was set at 0.05.
RESULTS
Returning to work and its association with demographic variables, cognitive performance (CoMet), and participants’ own views of working-related matters
A total of 27 participants (37%) had returned to work by 6 months after the stroke. Nineteen of these had returned to their previous jobs, 1 had an altered job description for the previous job, 4 were in part-time jobs, and 3 were in work try-outs.
After 12 months, 37 individuals (58%) had returned to work (Fig. 1). Of the returned individuals, 25 had returned to their previous jobs, 8 were in part-time jobs, and 4 were in work try-outs. No significant correlations were detected between returning to work and age, sex, or educational level, and no association was found between premorbid occupational status and returning to work (χ2) at either 6 or 12 months after stroke.
The mean of the CoMet total score was 119 (range 37–149). Better cognitive performance (high CoMet total score) was significantly correlated with returning to work at 6 (r = 0.310; p = 0.008) months after stroke (Table II). A significant difference was noted in CoMet mean scores between groups returning and not returning to work at 6 (p = 0.01) and 12 months (p = 0.049) after stroke (Table III).
| Returning to work after 6 months (r) | Returning to work after 12 months (r) | |
| Cognitive performance Initial assessment |
||
| CoMet total scorea | 0.310** | 0.213 |
| Motivation | ||
| Six-month follow-up | ||
| “Are you motivated to return to work?” | 0.255* | 0.155 |
| Perceived working abilityb Six-month follow-up first assessment period |
||
| “Evaluate your working ability from 1 to 10, where 10 describes your working ability when at the best possible level” ability at best” | 0.496** | 0.458** |
| “Evaluate your working ability in terms of physical demands” | 0.396** | 0.412** |
| “Evaluate your working ability in terms of mental demands” | 0.210 | 0.125 |
| Twelve-month follow-up | ||
| “Evaluate your working ability from 1 to 10, where 10 describes your working ability when at the best possible level” | 0.607** | 0.728** |
| “Evaluate your working ability in terms of physical demands” | 0.479** | 0.638** |
| “Evaluate your working ability in terms of mental demands” | 0.493** | 0.580** |
| Perceived barriersb “Do you have problems with following issues concerning your ability or strength to carry on in your duties?” Six-month follow-up “Do you have problems with following issues concerning your ability or strength to carry on in your duties:” First assessment period |
||
| “Issues concerning your health or functional ability” | –0.242* | –0.213 |
| “Lack of education or know-how” | –0.322** | –0.358* |
| “Problems concerning physical load in your duties or working environment” | –0.265* | –0.252* |
| “Mental stress in the work or in the work community” | –0.137 | –0.255* |
| “Lack of motivation or will to work” | –0.078 | –0.104 |
| “Problems outside of the work (in family, financial situation etc.)” | –0.109 | –0.310* |
| Sum score | –0.310 | –0.371** |
| Twelve-month follow-up | ||
| “Issues concerning your health or functional ability” | –0.486** | –0.640** |
| “Lack of education or know-how” | –0.263* | –0.289* |
| “Problems concerning physical load in your duties or working environment” | –0.514** | –0.591** |
| “Mental stress in the work or in the work community” | –0.319* | –0.501** |
| “Lack of motivation or will to work” | –0.245 | –0.412** |
| “Problems outside of the work (in family, financial situation etc.)” | –0.186 | –0.343** |
| Sum score | –0.477** | –0.660** |
| aCognitive screening methods (CoMet) (20); total score consisting of the scores of 11 subtests of CoMet. The CoMet also includes self-evaluation, but this was not included in the CoMet total score. bPerceived working ability was evaluated with 3 questions and perceived barriers with 6 questions from the questionnaire on work-related matters (Work Ability Index) (21). *p ≤ 0.05; **p ≤ 0.01. |
||
| Working | Not working | ||||
| CoMet total scorea | M (SD) | M (SD) | t | df | p-value |
| Six-month follow-up | 128 (15.3) | 114 (24.9) | –3.03 | 69.968 | 0.01 |
| Twelve-month follow-up | 124 (18.2) | 113 (25.8) | –2.0 | 62 | 0.049 |
| Motivation | % | % | χ2 p | ||
| Six-month follow-up | 36% | 49% | 0.034 | ||
| Twelve-month follow-up | 52% | 33% | 0.214 | ||
| No motivation | |||||
| Six-month follow-up | 1% | 14% | 0.034 | ||
| Twelve-month follow-up | 6% | 9% | 0.214 | ||
| Perceived working abilityb | |||||
| Six-month follow-up | M (SD) | M (SD) | t | df | p-value |
| “Evaluate your working ability from 1 to 10, where 10 describes your working ability when at best possible level” | |||||
| Six-month follow-up | 6.7 (2.1) | 4.1 (2.3) | –4.769 | 67 | 0.001 |
| Twelve-month follow-up | 6.0 (2.5) | 3.7 (2.1) | –4.041 | 60 | 0.001 |
| “Evaluate your working ability in terms of physical demands” | |||||
| Six-month follow-up | 3.4 (1.0) | 2.5 (0.9) | –3.669 | 67 | 0.001 |
| Twelve-month follow-up | 3.2 (1.1) | 2.2 (0.9) | –3.574 | 60 | 0.001 |
| “Evaluate your working ability in terms of mental demands” | |||||
| Six-month follow-up | 3.3 (0.8) | 2.9 (0.9) | –1.687 | 67 | 0.096 |
| Twelve-month follow-up | 3.1 (0.9) | 2.9 (1.0) | –0.891 | 60 | 0.376 |
| Perceived working abilityb | |||||
| Twelve-month follow-up | |||||
| “Evaluate your working ability from 1 to 10, where 10 describes your working ability when at best possible level” | |||||
| Six-month follow-up | 8.1 (1.2) | 4.7 (3.1) | –6.37 | 53 | 0.001 |
| Twelve-month follow-up | 8 (1.2) | 3.4 (2.8) | –7.814 | 32.7 | 0.001 |
| “Evaluate your working ability in terms of physical demands” | |||||
| Six-month follow-up | 4 (0.7) | 2.8 (1.2) | –4.883 | 61 | 0.001 |
| Twelve-month follow-up | 3.9 (0.7) | 2.4 (1.1) | –6.326 | 43.1 | 0.001 |
| “Evaluate your working ability in terms of mental demands” | |||||
| Six-month follow-up | 4 (0.96) | 2.9 (1.0) | –4.246 | 62 | 0.001 |
| Twelve-month follow-up | 3.9 (0.8) | 2.6 (1.0) | –5.601 | 62 | 0.001 |
| Perceived barriersb | |||||
| Six-month follow-up sum score | |||||
| Six-month follow-up | 10 (3.4) | 12 (3.6) | 2.449 | 68 | 0.017 |
| Twelve-month follow-up | 11.2 (4.8) | 15.2 (4.9) | 0.996 | 6 | 0.358 |
| aCognitive screening methods (CoMet) (20); total score consisting of scores of 11 subtests of CoMet. The CoMet also includes self-evaluation, but this was not included in the CoMet total score. bPerceived working ability was evaluated with 3 questions and perceived barriers with 6 questions from the questionnaire on work-related matters (Work Ability Index) (21). M: mean; SD: standard deviation. |
|||||
Higher motivation was significantly associated with returning to work 6 months after stroke (Table II). Positively perceived working ability correlated significantly with return-to-work at 6 and 12 months after stroke (Table II). Significant negative correlations were also found between more pronounced perceived barriers for returning to work detected at 6 months after stroke and actually returning to work by 6 and 12 months after stroke (see Table II).
Predicting return-to-work
Logistic regression analysis revealed that the CoMet total score from the first weeks to months after stroke correctly predicted 80% (N37) of the individuals who had not returned to work by 6 months after stroke and 37% (N10) of those who had returned to work. By the 12-month follow-up, the predictability of getting back to work based on self-perceived working ability and barriers was 64% (N16) for those who had not returned and 78% (N29) for those who had returned (Table IV).
| Predictor | Return-to-work | |||||||||||
| Six months, 95% CI | 12 months, 95% CI | |||||||||||
| B | SE B | Exp(B) | p-value | Lower limit | Upper Limit | B | SE B | Exp(B) | p-value | Lower limit | Upper limit | |
| CoMet total scorea | 0.037 | 0.015 | 1.038 | 0.015 | 1.008 | 1.07 | 0.024 | 0.013 | 1.024 | 0.060 | 0.999 | 1.05 |
| Perceived working abilityb | 0.388 | 0.138 | 1.474 | 0.005 | 1.125 | 1.93 | ||||||
| Perceived barriersb | –0.187 | 0.102 | 0.830 | 0.067 | 0.679 | 1.013 | ||||||
| Constant | 0.739 | 1.442 | 2.093 | 0.608 | ||||||||
| ¹Cognitive screening methods (CoMet) (20); total score consisting of 11 subtests of CoMet. The CoMet also includes self-evaluation, but this was not included in the CoMet total score. ²Perceived working ability was evaluated with 3 questions and perceived barriers with 6 questions from the questionnaire on work-related matters (Work Ability Index) (21). 95% CI: 95% confidence interval. |
||||||||||||
Factors associated with work dropout
Five individuals (40% male) had returned to work by the 12-month follow-up, but they had dropped out of working life at the time of the 24-month follow-up assessment. Two of these participants had received a disability pension statement, and 2 had a disability pension application in process. The remaining 1 was studying. For 3 of these 5 individuals, the CoMet total score at the initial assessment clearly indicated cognitive dysfunction, varying between 100 and 136, while for the other 2, the CoMet total scores were 138 and 149, indicating no significant problems. The ages of these drop-outs ranged from 34 to 62 years (mean age 52 years). Their educational level varied from 1 to 3, and three were blue-collar and two were white-collar workers.
DISCUSSION
The aim of this study was to identify the factors associated with return-to-work after stroke. The study focused on stroke patient’s cognitive performance, motivation, self-perceived ability to work, and self-perceived barriers to returning to work as explanatory aspects of returning to work in stroke patients with no severe post-stroke dysfunction. Cognitive performance was connected to returning to work and predicted return-to-work by 6 months after the initial assessment. Stroke patients’ own evaluations of their working abilities and barriers predicted return-to-work by 12 months after the initial assessment.
The percentage of participants who returned to work in the current study sample was similar to that found in a previous review (22). Consistent with the study by Lindström et al. (23), no association was found between returning to work and sex. However, contradictory research findings have been published (16, 24, 25). In contrast to the current results, a younger age has been connected to returning to work (15, 24). This discrepancy might reflect age differences between the study participants. In a study by Varona et al. (15), participants were younger (15–45 years) than those in the current study, and the age range was wider, and these differences may have affected the connection with returning to work. No connection was found between occupational status and returning to work, but previous studies have indicated that white-collar workers were most likely to return to work after stroke (12, 18, 26). One of our exclusion criteria in this study was a pre-estimated unlikeliness to return to work, which would have an impact on the severity of post-stroke dysfunction in our sample. This might explain the lack of connection observed between occupation status and returning to work in the current study, since patients with severe physical injury were excluded from the study.
In line with previous studies (8, 9), we found an association between cognitive impairments and returning to work. CoMet was used for cognitive screening, and its ability as a predictor appeared high (80%) for participants who had not returned to work by the 6-month follow-up. However, CoMet was not sufficient for predicting returning to work at the 12-month follow-up. This is probably because much healing and rehabilitation had occurred during the follow-up time, which could explain the CoMet’s lower prediction ability at 12 months after the initial assessment. The CoMet sumscore differences between the groups returning and not returning to work were statistically significant at both the 6-month and 12-month follow-ups. However, the CoMet mean sumscore indicated cognitive problems in both groups, suggesting the probability of cognitive dysfunction occurring to some extent when returning to work.
The findings presented here indicate that self-perceived working ability and barriers, along with cognitive deficits, were strongly connected with returning to work. Previous studies have highlighted the importance of hearing and prioritizing the voice of a stroke survivor as an expert on their journey in returning to work after stroke (9, 27), and our findings support this stance. Based on the present findings, both cognitive deficits and the patients’ own views of their competence and motivations need to be considered when planning returning to work.
The challenge faced by stroke patients is not only returning to work, but also staying at work after a stroke (19). Alaszevski et al. (7) reported that “some individuals may return to work rapidly with the aim to minimize the significance of the stroke within their personal narrative.” The speed of return to work is not necessarily connected to the severity of dysfunction, and invisible cognitive deficits may jeopardize survival of the return to work (10). In a recent study, Aarnio et al. (12) found that approximately 20% of individuals who had returned to work at 1 year after stroke had dropped out of working life by the 5-year follow-up. In the current study, 14% of those who had returned to work by the 12-month follow-up had dropped out between the 12- and 24-month follow-ups. However, the analysis of the drop-outs in this study was not adequate, given that the 24-month follow-up included only part of the group, which was a consequence of the 3-year timeframe for the current study data collection. The shortcomings regarding the number of participants at the 12-month follow-up, the shorter follow-up time, and the exclusion of participants unlikely to return to work might explain the smaller number of work drop-outs in the current study. The CoMet total score indicated cognitive dysfunction for 3 of the 5 drop-outs. A small majority of those who dropped out were women and blue-collar workers. Cognitive performance seemed to have an impact on managing working life after stroke, but further studies with a larger number of individuals are needed to verify the reasons for dropping out.
This study had some limitations that should be considered when interpreting and generalizing the findings. Individuals with severe post-stroke deficits were excluded from the study due to the initial exclusion of those unlikely to return to work. However, mild cognitive dysfunction might also jeopardize the stroke survivor’s management of work and is therefore an important area of research. Motivation was measured with only 1 dichotomous question; therefore, this should be considered when drawing conclusions. This study had 13 drop-outs by the 12-month follow-up, and this could have had an effect on the analysis. The 24-month follow-up consisted of a subsample of 44 subjects, so caution should be used when interpreting these results.
Based on the current findings, cognitive performance assessed with a screening test (CoMet) predicted return-to-work life after stroke. An individual’s own view of their working ability and barriers were also connected to returning to work and should be taken into consideration. In clinical practice, every stroke patient of working age should undergo a routine cognitive evaluation. A screening test provides an opportunity to identify individuals who are in need of comprehensive neuropsychological assessment. More long-term follow-up studies are needed to determine how well stroke survivors manage in their working lives and the importance of the patient’s own voice and perceived working ability.
ACKNOWLEDGEMENTS
Funding statement. The authors thank the University of Jyväskylä for funding this article.
The authors have no conflicts of interest to declare.
REFERENCES
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life-years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2197–2223.
- Kersten P, Low JTS, Ashburn A, George SL, McLellan DL. The unmet needs of young people who have had a stroke: results of a national UK survey. Disabil Rehabil 2002; 24: 860–866.
- Hall MJ, Levant S, DeFrances CJ. Hospitalization for stroke in U.S. hospitals, 1989–2009. 2012 NCHS Data Brief 2012 May; 95: 1–8.
- Lawrence M. Young adults’ experience of stroke: a qualitative review of the literature. Br J Nurs 2010; 19: 241–248.
- Edwards JD, Kapoor A, Linkewich E, Swartz RH. Return to work after young stroke: a systematic review. Int J Stroke 2018; 13: 243–256.
- Corr S, Wilmer S. Returning to work after a stroke: an important but neglected area. Br J Occup Ther 2003; 66: 186–192.
- Alaszewski A, Alaszewski H, Potter J, Penhale P. Working after a stroke: survivors’ experiences and perceptions of barriers to and facilitators of the return to paid employment. Disabil Rehabil 2007; 29: 1858–1869.
- Kauranen T, Turunen K, Laari S, Mustanoja S, Baumann P, Poutiainen E. The severity of cognitive deficits predicts return to work after a first-ever ischaemic stroke. J Neurol Neurosurg Psychiatry 2013; 84: 316–321.
- Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. J Rehabil Med 2003; 35: 127–131.
- Balasooriya-Smeekens C, Bateman A, Mant J, De Simoni A. Barriers and facilitators to staying in work after stroke: insight from an online forum. BMJ Open 2016; 6: e009974.
- Scott SL, Burns SP, Schwartz J, Kovic, M. Returning to work after mild stroke. Arch Phys Med Rehabil 2019; 100: 379–383.
- Aarnio K, Rodríguez-Pardo J, Siegerink B, Hardt J, Broman J, Tulkki L. et al. Return to work after ischemic stroke in young adults: a registry-based follow-up study. Neurol 2018; 91: 1909–e1917.
- Glozier N, Hackett ML, Parag V, Anderson CS. The influence of psychiatric morbidity on return to paid work after stroke in younger adults. Stroke 2008; 39: 1526–1532.
- Trygged S, Ahacic K, Kåreholt I. Income and education as predictors of return to working life among younger stroke patients. BMC Public Health 2011; 11: 1–9.
- Varona JF, Bermejo F, Guerra, JM, Molina JA. Long-term prognosis of ischemic stroke in young adults. J Neurol 2004; 251: 507–1514.
- Chang WH, Sohn MK, Lee J, Kim DY, Lee SG, Chin YI et al. Return to work after stroke: The Kosco study. J Rehabil Med 2016; 48: 273–279.
- Tanaka H, Toyonaga T, Hashimoto H. Functional and occupational characteristics associated with very early return to work after stroke in Japan. Arch Phys Med Rehabil 2011; 92: 743–748.
- Saeki S, Ogata H, Okubo T, Takahashi K, Hoshuyama T. Return to work after stroke. Stroke 1995; 26: 399–401.
- Coole C, Radford K, Grant M, Terry J. Returning to work after stroke: perspectives of employer stakeholders, a qualitative study. J Occup Rehabil 2013; 23: 406–418.
- Saar K, Nyrkkö H, Tolvanen A, Kuikka P, Poutiainen E, Aro T. Validation of a new cognitive screening method for stroke patients. Behav Neurol 2019: 2943603.
- Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A. Work Ability Index. Helsinki: Työterveyslaitos; 1998.
- Edwards JD, Kapoor A, Linkewich E, Swartz RH. Return to work after young stroke: a systematic review. Int J Stroke 2018; 13: 243–256.
- Lindström B, Röding J, Sundelin G. Positive attitudes and preserved high level of motor performance are important factors for return to work in younger persons after stroke: a national survey. J Rehabil Med 2009; 41: 714–718.
- Hackett ML, Glozier N, Jan S, Lindley R. Returning to paid employment after stroke: the Psychosocial Outcomes In StrokE (POISE) cohort study. PloS One 2012; 7: e41795.
- Palstam A, Westerlind E, Persson H. Work-related predictors for return to work after stroke. Acta Neurol Scand 2019; 139: 382–388.
- Hofgren C, Björkdahl A, Esbjörnsson E, Stibrant-Sunnerhagen K. Recovery after stroke: cognition, ADL function and return to work. Acta Neurol Scand 2007; 115: 73–80.
- Wolfenden B, Grace M. Returning to work after stroke: a review. Int J Rehabil Res 2009; 32: 93–97.