ORIGINAL REPORT
AN EARLY BIOPSYCHOSOCIAL INTERVENTION DESIGN FOR THE PREVENTION OF LOW BACK PAIN CHRONICITY: A MULTIDISCIPLINARY EMPIRICAL APPROACH
Linda NIEMINEN, MD1,2, Jari VUORI, PhD3,4,5 and Markku KANKAANPÄÄ, MD, PhD1,2
From the 1Department of Rehabilitation and Psychosocial Support, Tampere University Hospital, Tampere, Finland, 2Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland, 3Faculty of Business and Management, Tampere University, Tampere, Finland, 4Social Insurance Institution of Finland, Helsinki, Finland and 5Center for Organization Research and Design, Arizona State University, Phoenix, Arizona, USA
Objective: Comprehensive intervention models for prevention of chronification of low back pain, in which the early identification of holistic risk factors is considered are needed. The aim of this study is to design a tailored biopsychosocial intervention for patients with low back pain to prevent pain chronicity.
Design: A multidisciplinary empirical approach.
Methods: A multidisciplinary team designed a biopsychosocial intervention following an application from the Medical Research Council’s complex intervention framework. The methods used included problem identification, identification of the evidence, theory, and needs, examination of the current context and modelling of the theory. Biomechanical, psychological, social and environmental, and lifestyle and personal risk factors were taken into account.
Results: The intervention process was introduced in a logic model. The model presents all the required resources, their activities and outputs, as well as the outcomes and impacts of the intervention. The intervention was tailored according to the underlying risk factors for pain chronification in patients with low back pain.
Conclusion: A comprehensive tailored intervention may decrease the risk of pain chronicity. Further studies are needed to obtain information on the feasibility, effectiveness and cost-effectiveness of such interventions.
LAY ABSTRACT
Low back pain is the leading cause of years lived with disability worldwide. In cases of non-specific low back pain, a specific structural reason for the pain cannot be identified. It is recognized, however, that individual factors, such as biomechanical, psychological, social, environmental, lifestyle, and personal factors, can increase the risk of pain chronicity. Therefore, a multidisciplinary intervention was designed to address these individual factors in addition to traditional treatment methods. The intervention was also designed to improve the timing of the rehabilitation to prevent pain chronification. This study presents the background, the different phases of the design process, and the model for the intervention. Further studies will be conducted to determine the applicability and effectiveness of the design.
Key words: low back pain; chronic pain; biopsychosocial model; rehabilitation; multidisciplinary research.
Citation: J Rehabil Med 2022; 54: jrm00338. DOI: https://doi.org/10.2340/jrm.v54.2723
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Sep 8, 2022; Epub ahead of print: Oct 3, 2022; Published: Oct 21, 2022
Correspondence address: Linda Nieminen, Department of Rehabilitation and Psychosocial Support, Tampere University Hospital, PO Box 2000, FI-33521 Tampere, Finland. E-mail: linda.k.nieminen@pshp.fi
Public health requires immediate global intervention actions (1) for the early identification of risk factors associated with chronicity of low back pain (LBP) (2). In terms of disability, LBP is the most burdensome global health problem (3). To date, many LBP interventions have been introduced, but, in many cases, the knowledge of key professionals has not been exploited holistically enough. Likewise, very few interventions are truly comprehensive mutualistic models in which the multiple risk factors driving pain and disability and their interactions are considered (4). Furthermore, there is a scarcity of usage of intervention frameworks that increase the validity of the design and decrease resource waste (5). The key problems concerning the effective rehabilitation of patients with LBP are mostly related to the correct timing of risk stratification, the tailoring of interventions, and the mutuality between healthcare professionals and patients.
Achieving the correct timing of rehabilitation is difficult, especially in patients with multiple morbidities where the steps involved are considered highly complex. In particular, the problems associated with LBP should be explored in more detail regarding the timing and shared decision-making for rehabilitation in rapidly ageing populations of people with biased health information. Therefore, to scrutinize the health problems associated with LBP, the following questions should be answered: how can healthcare professionals identify the relevant factors that affect the risk of chronicity in patients with LBP in a comprehensive and timely manner? How can healthcare professionals proceed effectively in the rehabilitation process with colleagues if this data is unavailable at the beginning of the process?
With the increasing costs of healthcare, new interventions should aim to add effectiveness to the margins of the available resources. Although not all patients with LBP need comprehensive, multidisciplinary rehabilitation, the delayed detection of patients at risk of chronicity can result in excessive costs, not to mention the burden for the patient in terms of decreased quality of life and functioning. The foundations of new interventions should be based on value clarifications (where the patient’s values and preferences are heard during the decision-making process) (6) and value-based healthcare (VBHC). Thus, the interventions should be equitable, sustainable, and transparent, while using the resources available to achieve better outcomes and experiences for all patients. The aim should be to deliver the best possible outcome for patients individually with the resources available (7).
This study develops a comprehensive intervention for non-specific LBP suitable for primary and occupational healthcare. The effective healthcare policy aim is to prevent chronicity of pain and disability by considering the whole spectrum of disability and health in accordance with the International Classification of Functioning, Disability, and Health (ICF). A secondary aim is to identify the individualized needs of patients according to the underlying risk factors in the rehabilitation process using the following research questions:
- Which healthcare professionals and stakeholders are needed in primary healthcare for the effective prevention of LBP chronicity?
- What are the roles of different healthcare professionals in the intervention processes of patients with risk factors for LBP?
METHODS
The design of the intervention (Table I) followed the development phase of United Kingdom Medical Research Council’s (MRC) complex interventions framework (8), which is the most cited guidance using an iterative approach (5). A new update of the framework came at the end of the design process, and the intervention design reflected the most recent implications (9). The optimization of the design was adopted from a framework application, which enriches the development phase of the MRC framework. The approach adds crucial elements to the development phase to strengthen the internal and external validity, to minimize research waste, and to add value to healthcare research (5). The rehabilitation design was divided into 4 sections to represent those risk factors affecting patients with non-specific LBP: biomechanical, psychological, social and environmental, and lifestyle and personal.
Multidisciplinary professional teams involving different stakeholders were gathered to design the intervention. To be included in the team, participants had to have strong knowledge of treating patients with LBP, at least several years of work experience, and the will and vision to advance the management of patients with LBP in their working environment. The teams included physicians, physiotherapists, mental health physiotherapists, nurses, a psychologist specialized in pain management, a social worker, and a rehabilitation counsellor (Table II). The teams worked via remote meetings between April 2021 and February 2022. Before the collaborative discussion, the chairperson gave an introduction based on scientific literature concerning the subject of the meeting.
At the beginning of the design process of the intervention (phases I and II, Table I), a previous systematic review of the risk factors for LBP chronicity (2) was examined and compared with the experience the professionals in the current study encountered in their daily work. Another review of the literature was performed to increase our understanding of previous interventions. The aim was to provide a representative picture of the literature rather than execute a comprehensive systematic review. The previous interventions were discussed in the teams in terms of their usefulness for the design. The search (Table III) was made with an advanced search (query from title/abstract with LBP, intervention, and hypernym of different risk factors, e.g. psychological) from PubMed and Google Scholar, and the references of suitable articles were searched for additional articles. The principal patient group was patients with back pain; however, due to the lack of articles that would be applicable to the healthcare system in question, a few articles from patients with other painful musculoskeletal disorders were also included. In addition, systematic reviews with other patients groups could also be accepted. In the search for articles concerning social or lifestyle factors associated with back pain, articles with interventions targeting the risk factors associated with LBP chronicity (LBP was excluded from the query) were also accepted.
The psychological theories of health behaviour were studied and their applicability for the intervention was discussed. Behaviour change techniques were examined in terms of the desired change, and were reflected in the chosen psychological theories (phase III). The main challenges for patients with LBP in functioning and health within the ICF framework were examined from a secondary analysis of a retrospective population study of patients with chronic LBP (10). The ICF framework was used to further discuss the domains where the intervention was to be targeted (phase IV). In addition, current resources were discussed as well as the problems in the clinical pathways of patients with complex LBP. The facilitators of, and barriers to, the intervention givers and receivers were identified (phase V). In the final phase of the intervention design (phase VI), the implementation road map was planned.
RESULTS
Problem identification
A systematic review was used as a basis to identify the risk factors for LBP chronicity (2). The teams discussed those factors that, in their opinion, play a crucial role in LBP chronicity (Table IV). A flow chart of patients with non-specific LBP from primary contact to the intervention was identified. The primary contact is a direct access physiotherapist (PT) when red flags or specific reasons for LBP are not identified during the treatment needs assessment. In cases where red flags are identified, the primary contact is a physician. A healthcare professional (direct access PT or physician) then performs an initial assessment and interview, excludes mechanical and specific reasons for LBP (11), gives pain education and plans the treatment and rehabilitation needs. Assessment of the risk factors for chronic LBP will be conducted during the follow-up visits (2–3 weeks from initial visit) and, if these factors are recognized, a broader multidisciplinary team will be contacted according to the factors identified.
| Psychological factors | Social and environmental factors | ||
| Clinical experience | Systematic review | Clinical experience | Systematic review |
| Depression | Depression | Difficulties in social affairs | Good quality of life (protective) |
| Anxiety | General anxiety | Challenging family obligations | – |
| Traumatic experiences | Post-traumatic stress disorder | Difficulties in work adaption | Support at work (protective) |
| Fatigue | Any psychiatric diagnosis | Workload too excessive | Work-related back pain |
| Catastrophizing | Catastrophizing | Returning to work after long sickness leave | – |
| Certain personality disorders | Somatization | Contradictions in the workplace | Non-recognition of work |
| Prolonged stress | Perceived stress | Financial problems | Disability compensation |
| Pain-related fear behaviour | Low tolerance of pain | Cultural background and age | – |
| Low self-efficacy, resources | Perceived risk of persistence | Level of education | – |
| Addictions | Coping by ignoring pain | Form of residence | – |
| Sleep disorders | – | ||
| Biomechanical factors | Lifestyle and personal factors | ||
| Clinical experience | Systematic review | Clinical experience | Systematic review |
| Physically heavy work | Particularly physical work | Multimorbidity | – |
| Inactive lifestyle | Physical exercise (protective) | Smoking | Nicotine dependence |
| Disabilities in the musculoskeletal system | Baseline disability | Diabetes | Diabetes |
| Unhealthy lifestyle combined | Physical wellbeing (protective) | Obesity | Obesity |
| – | Difficult working positions | Inactive lifestyle | Poor health |
| – | Carrying heavy loads | Disability | Baseline disability |
| – | Vibrations and jolts | Previous LBP episodes | Previous episode of LBP |
| Sleep disorders | – | ||
| – | Female sex | ||
Identifying the evidence
In the literature review, an introduction consisted of the Finnish National Current Care Guideline for treating LBP (12), previous systematic reviews considering the prolongation of pain and disability (2, 13, 14), and an article explaining the development of chronic pain (15). The reviews used to support the development of the national public rehabilitation guidelines organized by the Social Insurance Institution of Finland were introduced. The first review concerned the rehabilitation of musculoskeletal disorders as a whole (16), and the latter the rehabilitation of patients with subacute back pain with biopsychosocial aspects and patient stratification (17). In addition, the Cochrane review on multidisciplinary biopsychosocial rehabilitation was presented (18).
In addition to the preface, 26 studies were found suitable for strengthening the scientific foundation of the design (19–44). Details of the studies and the comments of the teams are shown in Appendix I.
Identifying the theory
The perception of different behaviour change theories was initiated with the COM-B system (45). This system works as an umbrella theory to understand different aspects of how a theory works on capability, opportunity, and motivation. Behaviour change techniques were explored to increase the understanding of the theoretical background of the techniques already used in everyday practice (46, 47). Finally, different theories were studied more closely. The theory of planned behaviour, social-cognitive theory and self-regulation theories were found suitable to form a base for the intervention (48). From the basis of the theories, the chosen behavioural change techniques were as follows:
- Goals should be timely, realistic, concrete, with graded tasks, and meet with the recipient’s resources.
- Provider’s support, monitoring and feedback are important, concrete exercises with the provider.
- Activities should be planned beforehand (what, where, when, how and with whom).
- Positive beliefs and self-efficacy should be amplified, discrepant views should be confronted.
- Motivation and positive changes should be amplified from the recipient’s perspective, and providers should only support the recipient’s own remarks.
- Recipient’s limitations and strengths should be recognized, and empowering resources cherished.
- Self-monitoring with the recording of thoughts verbally and literally should be used to increase cognitive learning.
- Techniques based on self-belief (mental rehearsal, self-talk) as well as distraction should be used.
- The social and physical environment should be examined and opportunities for change should be created with the necessary services.
- Feelings of pain and discomfort should be encountered and normalized.
- Communality and reward systems should be benefitted.
Identifying needs
A secondary analysis of a retrospective population study of patients with chronic LBP (10) was examined to identify the main aspects of disability in the ICF framework. The recognition of the population’s difficulties in functioning and health was used to theoretically reflect the domains targeted by the intervention. During the design phase, the recipients were not included in the team. Instead, the ICHOM (International Consortium for Health Outcomes Measurement) standard set for LBP was followed (49) This is the reference for ICHOM to identify those outcomes that matter the most to patients.
Examining current context
The facilitators and barriers of the recipients and intervention givers were discussed (Table V). Clinical experience was used to identify the facilitators and barriers of the recipients. The themes were in line with previous studies on the subject (50). Some healthcare units have the required resources and, according to the team members, their availability is adequate. The mental health resources (mental health PT, psychiatric nurse and psychologist) were seen as the most vulnerable members of the multidisciplinary team. The time resource for risk recognition was also discussed as a possible dilemma. Different aspects to increase multidisciplinary collaboration were discussed through the team members’ previous experiences from their working environment.
Modelling the theory
The intervention was introduced in a logic model (Fig. 1). The model graphically represents the needed resources, their activities and intended effects, and the assumptions and contextual factors where the intervention operates (51). The healthcare professionals needed depend on the patient’s personal needs and the underlying risk factors. When certain risk factors are recognized, the process owner (e.g. in the biomechanical group PT; bold text in Fig. 1) will take charge of the multidisciplinary assessment and invite all the required professionals to the process. Additional inputs are principally contacted via a referral from the physician.
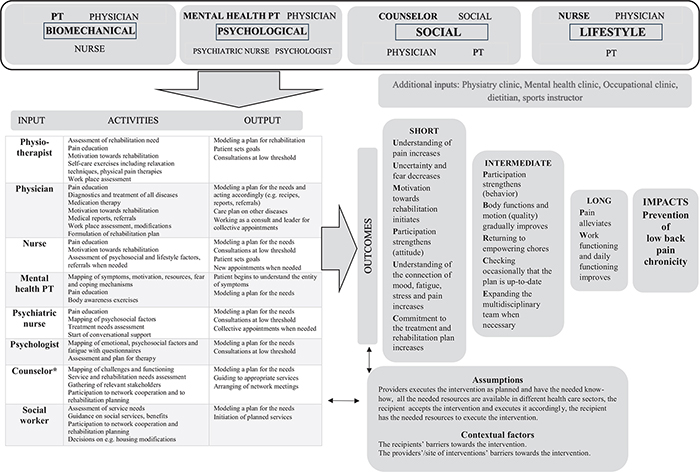
Fig. 1. Logic model for the intervention. The first contact in the different risk factor groups is shown in bold text.
*Rehabilitation counsellor, customer counsellor, social counsellor or nurse, depending on local resources.
DISCUSSION
This study outlines the design process of a multidisciplinary, tailored biopsychosocial intervention for the prevention of LBP chronicity. The design process was conducted using an iterative approach, since the elements have reciprocal relations (5). In future, a new reflection on the design elements will be collected from a feasibility study. Furthermore, economic considerations will be conducted with a cost-benefit analysis before a larger intervention study.
Adequate resources in the primary and occupational care for the early recognition of LBP chronicity should lead to cost-effective clinical pathways. At present, the prevalent clinical pathways in high-income countries are costly, and the financial burden is projected to increase in the coming decades (52). Global disability caused by LBP is highest among the working-age populations. In Europe, LBP is one of the most common causes of medically certified sick leave and early retirement (52). In addition, there is a correlation between longer-term disability and work absence extending beyond 1 month (53). These findings should encourage healthcare providers to find functional solutions to the primary contact site of patients with LBP.
Local resources may vary, which may complicate the implementation of the intervention. It is, therefore, desirable that the feasibility study should verify the resource needs identified in this design. Other implementation challenges are related to the reception of the intervention. To be accepted by the recipients, sufficient resources must be allocated for patient education before the intervention process begins. With limited time resources, the use of high-quality patient material (54) is strongly suggested. In addition, healthcare professionals must have adequate skills to recognize specific reasons for LBP, which might need different treatment approaches, such as interviews and examinations. In case the feasibility study, cost-benefit analysis, and larger intervention study find the designed intervention superior to present clinical practice, a strategy and evaluation protocol for the implementation should be created. A team of professionals is needed to define widely the outcome measures of the implementation (e.g. use of valid questionnaires such as Determinants of Implementation Behavior Questionnaire) (55), to monitor, as well as continuously develop, the process.
In this study, multidisciplinary teams brought their clinical experience to common use and the conversation was enriched with current scientific knowledge. Healthcare professional teams embedded within a complex system enabled team members to understand that rehabilitation as a complex system is not unitary, but an interdisciplinary concept constructed by different scientific terms. The teams explored answering “what if” questions to avoid the traps of rehabilitation defined solely by one discipline or profession. By doing this they were able to evaluate how alternative rehabilitation plans might be developed.
Although accurate plans for the recognition of the risk factors associated with pain chronicity were not in the scope of the intervention design phase, they were discussed within the teams. Different questionnaires (see Appendix I for team’s comments) were found to be suitable, going through the health records before the appointment was seen as important, as were bringing up the issues of mood, social situation, and lifestyle factors in the assessment conversation. In addition, evaluation of the outcomes was considered. The ICHOM working group (49) recommends using the Numerical Pain Rating Scale (NPRS), the Oswestry Disability Index (ODI), and EuroQol-5D for the evaluation of pain, disability and quality of life. 15D for health-related quality of life and Net Promoter Score (NPS) for patient satisfaction were also found to be suitable for the evaluation.
In future, artificial intelligence (AI) will help scientists to find answers for risk recognition. Moreover, AI technologies (10) could fill the gap in tailored solutions and help to achieve successful clinical pathways. However, AI cannot be exploited successfully until a mutual holistic understanding between all key healthcare professionals involved in the rehabilitation process is achieved.
This study has some limitations. The facilitators and barriers of the implementation site were not listed, as the exact site for the study was not decided during the design phase. However, the barriers connected to the resources, and the agreement regarding the possible variations were discussed, so that the intervention can still maintain the integrity of the core components while varying across different contexts (9). The absence of the recipients during the design phase was a weakness of this study. However, the completed intervention design was introduced to a LBP patient forum (10 experts by experience), where the intervention received mainly positive feedback. The exploitation of current resources on behalf of patients with LBP, the structure of the intervention, and low thresholds between professionals were mentioned. Education of professionals, especially regarding the patient encounters, the availability of resources in terms of time, and skilful professionals were listed as development targets. In addition, patient satisfaction, and their overall opinion on the intervention will be collected during the feasibility study before larger intervention. The intervention will be conducted as a case-control study to avoid the confounding factors of local phenomena.
In the near future, it is hoped that more biopsychosocial primary healthcare interventions from similar healthcare systems will be developed, so that benchmarking analyses can be conducted. It would also be beneficial to find an agreement on the evaluation of implementation and outcomes for an effective comparison.
In conclusion, this study developed a multidisciplinary rehabilitation for non-specific LBP, which holistically considers the entities of functioning, disability, and health in accordance with the ICF framework. The design has the potential to broaden our understanding of disability, lower the threshold for collaboration between different healthcare professionals and healthcare sectors, move the rehabilitation pathway towards preventive services, and decrease the risk of pain chronicity.
ACKNOWLEDGEMENTS
The authors thank all the professionals from Tampere, Valkeakoski, and Kangasala social and health services, Pirte occupational healthcare services, Tampere University and Tampere University Hospital for participating in the intervention design, and also the LBP patient forum from Tampere University hospital for their valuable comments.
This study was financially supported by Tampere University Hospital Support Foundation, Tampere University Hospital.
The authors have no conflicts of interest to declare. The authors accept and agree with the United Nations (UN)’s Declaration of Human Rights.
REFERENCES
- Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: a call for action. [Cited 2022 Mar 15]. Lancet 2018; 391: 2384–2388. Available from: https://www.sciencedirect.com/science/article/pii/S0140673618304884
- Nieminen LK, Pyysalo LM, Kankaanpää MJ. Prognostic factors for pain chronicity in low back pain: a systematic review. [Cited 2022 Mar 15]. Pain Rep 2021; 6: e919[17 p.]. Available from: https://journals.lww.com/painrpts/Fulltext/2021/01000/Prognostic_factors_for_pain_chronicity_in_low_back.43.aspx
- Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. [cited 2022 May 3]. Ann Transl Med 2020 Mar;8:299[14 p.]. Available from: /pmc/articles/PMC7186678/
- Tousignant-Laflamme Y, Martel MO, Joshi AB, Cook CE. Rehabilitation management of low back pain – it’s time to pull it all together! J Pain Res 2017; 10: 2373–2385.
- Bleijenberg N, de Man-van Ginkel JM, Trappenburg JCA, Ettema RGA, Sino CG, Heim N, et al. Increasing value and reducing waste by optimizing the development of complex interventions: enriching the development phase of the Medical Research Council (MRC) Framework. Int J Nurs Stud 2018; 79: 86–93.
- Llewellyn-Thomas HA, Crump RT. Decision support for patients: values clarification and preference elicitation. [Cited 2022 Mar 21]. Med Care Res Rev 2012 Nov; 70: 50S–79S. Available from: https://doi.org/10.1177/1077558712461182
- Hurst L, Pluddemann A, Lewis S, Harvey K, Briggs A, Boylan A-M, et al. Defining Value-based Healthcare in the NHS: CEBM report May 2019. [Cited 2022 Mar 27]. Oxford: CEBM, University of Oxford. 2019 [14 p.]. Available from: https://www.cebm.ox.ac.uk/resources/reports/defining-value-based-healthcare-in-the-nhs
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000; 321: 694–696.
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. [Cited 2022 May 6]. BMJ 2021; 374: n2061 [11 p.]. Available from: http://www.bmj.com/content/374/bmj.n2061.abstract
- Nieminen L, Vuori J, Ketamo H, Kankaanpää M. Applying semantic computing for health care professionals: the timing of intervention is the key for successful rehabilitation. In: Proceedings of 31st conference of open innovations association FRUCT. Helsinki, Finland: FRUCT Association; 2022, p. 201–206.
- O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther 2005 [cited 2022 Apr 13]; 10: 242–255. Available from: https://pubmed.ncbi.nlm.nih.gov/16154380/
- Working group set up by the Finnish Medical Society Duodecim and Finnish Society of Physical medicine and Rehabilitation. Low back pain. Current Care Guidelines. [Cited 2022 Mar 27]. Helsinki: The Finnish Medical Society Duodecim 2017. 2017. Available from: https://www.kaypahoito.fi/hoi20001
- Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med 2005; 62: 851–860.
- Steenstra IA, Munhall C, Irvin E, Oranye N, Passmore S, van Eerd D, et al. Systematic review of prognostic factors for return to work in workers with subacute and chronic low back pain. J Occup Rehabil 2017; 27: 369–381.
- Kalso E. Can pain becoming chronic be prevented? [Cited 2022 Mar 17]. Lääkärilehti. 2018; 18/2018 vsk 73:1119–1126. Available from: https://www.laakarilehti.fi/tieteessa/katsausartikkeli/miksi-kipu-pitkittyy-ja-voiko-sita-ehkaista/?public=219108ef10470df8d9b792c240c4f1fb#reference-62
- Häkkinen A, Aartolahti E, Tarnanen S, Nikander R, Heinonen A. Evidence-based rehabilitation of musculoskeletal disorders. [Cited 2022 Mar 17]. Kela 2014. Available from: https://helda.helsinki.fi/bitstream/handle/10138/144093/Tyopapereita68.pdf?sequence
- Pasternack I, Saronkari M, Fogelholm C, Mäkelä M. Treatment of subacute back pain in primary health care - a systematic review on the effectiveness of biopsychosocial rehabilitation and patient stratification. [Cited 2022 Mar 17]. Summaryx Ltd. 2018 Apr. Available from: https://app.box.com/s/0msxfuxxcmcdm2cjl2tu50gqpc35vrsd
- Marin TJ, van Eerd D, Irvin E, Couban R, Koes BW, Malmivaara A, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. [Cited 2022 Mar 17]. Cochrane Database Syst Rev 2017; (6) [86 p.]. Available from: https://doi.org//10.1002/14651858.CD002193.pub2
- Anema JR, Steenstra IA, Bongers PM, de Vet HC, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine (Phila Pa 1976) 2007; 32: 291–300.
- Baadjou VA, Lee H, Smeets RJ, Kamper SJ. How much of the effect of exercise and advice for subacute low back pain is mediated by depressive symptoms? Musculoskelet Sci Pract 2019; 44: 102055.
- Baez S, Hoch MC, Hoch JM. Evaluation of cognitive behavioral interventions and psychoeducation implemented by rehabilitation specialists to treat fear-avoidance beliefs in patients with low back pain: a systematic review. Arch Phys Med Rehabil 2018; 99: 2287–2298.
- Beneciuk JM, Hill JC, Campbell P, Afolabi E, George SZ, Dunn KM, et al. Identifying treatment effect modifiers in the STarT Back Trial: a secondary analysis. J Pain 2017;18:54–65.
- Bültmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. J Occup Rehabil 2009; 19: 81–93.
- Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007; 66: 433–439.
- van Erp RMA, Huijnen IPJ, Jakobs MLG, Kleijnen J, Smeets RJEM. Effectiveness of primary care interventions using a biopsychosocial approach in chronic low back pain: a systematic review. Pain Pract 2019; 19: 224–241.
- Foster NE, Mullis R, Hill JC, Lewis M, Whitehurst DG, Doyle C, et al. Effect of stratified care for low back pain in family practice (IMPaCT Back): a prospective population-based sequential comparison. Ann Fam Med 2014; 12: 102–111.
- Hajihasani A, Rouhani M, Salavati M, Hedayati R, Kahlaee AH. The influence of cognitive behavioral therapy on pain, quality of life, and depression in patients receiving physical therapy for chronic low back pain: a systematic review. PM R 2019; 11: 167–176.
- Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum 2008; 59: 632–641.
- Karjalainen K, Malmivaara A, Pohjolainen T, Hurri H, Mutanen P, Rissanen P, et al. Mini-intervention for subacute low back pain: a randomized controlled trial. Spine (Phila Pa 1976) 2003; 28: 531–533.
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. [Cited 2022 Apr 07]. Cochrane Database Syst Rev 2017; (3) [70 p.]. Available from: https://doi.org//10.1002/14651858.CD001292.pub3
- Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, et al. A population-based, randomized clinical trial on back pain management. Spine (Phila Pa 1976) 1997; 22: 2911–2918.
- Nicholas MK, Linton SJ, Watson PJ, Main CJ, Group “Decade of the Flags” Working. Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther 2011; 91: 737–753.
- Rantonen J, Karppinen J, Vehtari A, Luoto S, Viikari-Juntura E, Hupli M, et al. Effectiveness of three interventions for secondary prevention of low back pain in the occupational health setting – a randomised controlled trial with a natural course control. BMC Public Health 2018; 18: 598.
- Rasmussen CD, Holtermann A, Jørgensen MB, Ørberg A, Mortensen OS, Søgaard K. A multi-faceted workplace intervention targeting low back pain was effective for physical work demands and maladaptive pain behaviours, but not for work ability and sickness absence: stepped wedge cluster randomised trial. Scand J Public Health 2016; 44: 560–570.
- Rosenberg NR, Petersen SB, Begtrup LM, Flachs EM, Petersen JA, Hansen BB, et al. Early occupational intervention for people with low back pain in physically demanding jobs: 1-year follow-up results of the randomized controlled GOBACK trial. Spine (Phila Pa 1976) 2021; 46: 347–355.
- Schiltenwolf M, Buchner M, Heindl B, von Reumont J, Müller A, Eich W. Comparison of a biopsychosocial therapy (BT) with a conventional biomedical therapy (MT) of subacute low back pain in the first episode of sick leave: a randomized controlled trial. Eur Spine J 2006; 15: 1083–1092.
- Shaw WS, Main CJ, Johnston V. Addressing occupational factors in the management of low back pain: implications for physical therapist practice. Phys Ther 2011; 91: 777–789.
- Stapelfeldt CM, Christiansen DH, Jensen OK, Nielsen C v, Petersen KD, Jensen C. Subgroup analyses on return to work in sick-listed employees with low back pain in a randomised trial comparing brief and multidisciplinary intervention. BMC Musculoskelet Disord 2011; 12: 112.
- Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health 2018; 18: 1376–1379.
- van Vilsteren M, van Oostrom SH, de Vet HCW, Franche RL, Boot CRL, Anema JR. Workplace interventions to prevent work disability in workers on sick leave. [Cited 2022 Apr 07]. Cochrane Database Syst Rev 2015; (10) [77 p.]. Available from: https://doi.org//10.1002/14651858.CD006955.pub3
- Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, de Boer WEL, Busse JW, et al. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database Syst Rev. 2017 [Cited 2022 Apr 07]; (3) [92 p.]. Available from: https://doi.org//10.1002/14651858.CD011618.pub2
- Wai E, Gruscynski A, Johnson G, Chow D, O’Neil J, Vexler L. Modifiable lifestyle factors in patients presenting to a tertiary spine surgery clinic. [cited 2022 May 3]. Orthopaed Proceed 2018 Feb; 90-B: 118. Available from: https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.90BSUPP_I.0880118a
- Wai EK, Rodriguez S, Dagenais S, Hall H. Evidence-informed management of chronic low back pain with physical activity, smoking cessation, and weight loss. Spine J 2008; 8: 195–202.
- Williams A, Wiggers J, O’Brien KM, Wolfenden L, Yoong SL, Hodder RK, et al. Effectiveness of a healthy lifestyle intervention for chronic low back pain: a randomised controlled trial. Pain 2018; 159: 1137–1146.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95.
- Hankonen N, Nuojua S, Ahokas M. Taxonomy on behavior change techniques: a step towards more systematic science of behavior change. [cited 2022 Mar 20]. Psykologia. 2017. Available from: https://www.researchgate.net/publication/316239233_Kayttaytymisen_muuttamisen_tekniikoiden_luokitusjarjestelma_askel_kohti_systemaattisempaa_kayttaytymismuutostiedetta
- Linnasaari A, Hankonen N, editors. Sinikallio S. Health psychology. How can health behaviour be effected. First, PS-kustannus. 2019. [cited 2022 Mar 20]. Available from: https://www2.helsinki.fi/sites/default/files/atoms/files/miten_terveyskayttaytymiseen_voidaan_vaikuttaa.pdf
- The International Consortium for Health Outcome Measures working group. The ICHOM standard set for low back pain. [Cited 2022 Apr 10]. Available from: https://connect.ichom.org/standard-sets/low-back-pain/
- Holopainen R, Simpson P, Piirainen A, Karppinen J, Schütze R, Smith A, et al. Physiotherapists’ perceptions of learning and implementing a biopsychosocial intervention to treat musculoskeletal pain conditions: a systematic review and metasynthesis of qualitative studies. Pain 2020; 161: 1150–1168.
- CDC Division for Heart Disease and Stroke Prevention. Evaluation guide. Developing and using a logic model. [Cited 2022 Mar 27]. 2021. Available from: https://www.cdc.gov/dhdsp/docs/logic_model.pdf
- Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018 Jun [cited 2022 Apr 13];391:2356–2367. Available from: https://pubmed.ncbi.nlm.nih.gov/29573870/
- Wynne-Jones G, Cowen J, Jordan JL, Uthman O, Main CJ, Glozier N, et al. Absence from work and return to work in people with back pain: a systematic review and meta-analysis. Occup Environ Med 2014 [cited 2022 Apr 21]; 71: 448–458. Available from: https://pubmed.ncbi.nlm.nih.gov/24186944/
- Simula AS, Jenkins HJ, Hancock MJ, Malmivaara A, Booth N, Karppinen J. Patient education booklet to support evidence-based low back pain care in primary care – a cluster randomized controlled trial. BMC Fam Pract 2021; 22: 178.
- Huijg JM, Gebhardt WA, Dusseldorp E, Verheijden MW, van der Zouwe N, Middelkoop BJ, et al. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement Sci 2014; 9: 33.