Original Report
RECOVERING FROM COVID-19 – A PROCESS CHARACTERIZED BY UNCERTAINTY: A QUALITATIVE STUDY
Marie ENGWALL, PhD1,2, Karin TÖRNBOM, PhD1,3, Hanna C. PERSSON, PhD1,4 and Annie PALSTAM, PhD1,5,6
From the 1Department of Clinical Neuroscience, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, 2Department of Health Science, University West, Trollhattan, 3Department of Social Work, University of Gothenburg, Gothenburg, 4Department of Occupational and Physiotherapy, Sahlgrenska University Hospital, 5Department of Neuroscience, Sahlgrenska University Hospital, Gothenburg and 6School of Health and Welfare, Dalarna University, Falun, Sweden
Objective: To obtain a deeper understanding of the lived experiences of patients with COVID-19, the recovery process and consequences for everyday life 6 months after hospital discharge.
Design: An explorative qualitative study using individual interviews.
Subjects: A purposive sampling was applied to recruit persons who had received inpatient hospital care, were discharged approximately 6 months previously, were of working age and had persistent self-reported symptoms at a 3-month follow-up appointment.
Methods: Semi-structured interviews were conducted with 15 participants (10 men, 5 women), which were then transcribed and analysed with inductive thematic analysis.
Results: Three themes were identified: “Status of recovery – two steps forward, one step back”, “Remaining symptoms caused limitations in everyday life” and “Strategies for recovery”. Participants indicated the recovery process through 6 months after discharge was a challenging road, often involving setbacks. A wide range of persistent, fluctuating, or new symptoms negatively impacted many areas of daily life, with fatigue and lack of energy being especially prominent. Participants used a variety of strategies to cope and recover.
Conclusion: This study increases our knowledge of the lived experiences of COVID-19 based individual experiences. Unexpected symptoms in the recovery process were described and not always possible to forecast.
LAY ABSTRACT
The aim of this study was to gain a deeper understanding of the lived experiences of patients with COVID-19, the recovery process and impacts on everyday life 6 months after hospital discharge. Included participants were discharged 6 months previously from inpatient care, and selected from a patient cohort. All participants had self-reported symptoms at a 3-month follow-up and were of working-age. Individual interviews were conducted with 15 participants (10 men, 5 women) following an interview guide developed together with patient partners, who were contributing to the research process. The interviews were analysed using thematic analysis. The results of the analysis revealed that the recovery process was experienced as a rocky and uncertain road, often involving setbacks. A wide range of persistent, fluctuating or newly developed symptoms had negative impacts on many areas of daily life, with fatigue and lack of energy being especially challenging. Participants used a variety of strategies to manage everyday life and recover.
Key words: persistent symptoms; qualitative research; coping strategies; inpatients; activities of daily living; COVID-19; follow-up studies.
Citation: J Rehabil Med 2022; 54: jrm00326. DOI: https://doi.org/10.2340/jrm.v54.2739
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jul 26, 2022; Epub ahead of print: Aug 17, 2022; Published: Sep 9, 2022
Correspondence address: Hanna C Persson, Sahlgrenska Academy at University of Gothenburg, Institute of Neuroscience and Physiology, Rehabilitation Medicine, Per Dubbsgatan 14, SE-413 45 Göteborg, Sweden. E-mail: hanna.persson@neuro.gu.se
Competing interests and funding: The authors have no conflicts of interest to declare.
Persistent symptoms and consequences of COVID-19, often referred to as long-COVID or post-COVID-19 (1, 2), are increasingly acknowledged as being both various and complex several months after infection. Two systematic reviews (3, 4), has reported that up to 80% of infected persons (most of those had been hospitalized), had 1 or more persistent long-term symptoms months after the acute COVID-19 infection. These symptoms were frequently reported in both qualitative and quantitative studies. Commonly reported symptoms were: fatigue, dyspnoea, myalgia, joint pain, deficits in cognitive function, neurological disorders, anxiety, depression (5–10), limitations in daily activities (5) and a reduced quality of life (11). Previous qualitative research concerning the experiences of hospitalized COVID-19 patients and their long-term symptoms and consequences for daily life exist (9), but are limited, as this is a current, rapidly evolving medical phenomenon.
There is a great need for knowledge about the variability of symptoms, the road to recovery and the lived experiences of persons with persistent symptoms, in order to better understand their needs for support and rehabilitation. As described in the biopsychosocial model of the International Classification of Functioning, Disability and Health (ICF) (12), a disease may impact body functions and structure, as well as activity and participation, and these perspectives must be included when investigating the lived experiences of having been ill with COVID-19 (13). There is also a need for research, especially on patients with persistent symptoms after COVID-19, who needed to be treated in hospital due to the initial critical severity of the infection, as these patients have an increased risk of developing severe residual symptoms after COVID-19 (10, 14). Patients who were cared for in intensive care are the group who are particularly vulnerable and susceptible to developing severe long-term symptoms related to the disease. This patient group is also the most likely to require care regarding any persistent symptoms after COVID-19 (15).
To date, many studies have identified a wide range of symptoms post COVID-19, as well as stories about how these symptoms are experienced 1–3 months after discharge from hospital (16). The need for formal methodologically sound qualitative research is crucial to obtain a wide range of perspectives on how persons describe the recovery processes and lived experiences of this disease. Persistent symptoms after COVID-19 occur in some persons for an extended period, and it is unknown how long these symptoms will be problematic. It is important to continue longitudinal investigations to gain knowledge about whether persons are still living with residual symptoms after COVID-19 and in what way these symptoms have affected their health and impacted their lives in the longer term (17, 18). To tailor targeted care and rehabilitation for this group, it is important to investigate if the changes are perceived as permanent or still as transitory. There is a lack of in-depth exploration about varieties of experience, management and recovery of symptoms related to COVID-19 in everyday life after 6 months or more. The aim of the current study was to obtain a deeper understanding of the lived experiences of COVID-19, the recovery process and impacts on everyday life 6 months after hospital discharge.
METHODS
Study design
This is an explorative qualitative study using individual interviews and inductive thematic analysis (19), which can be referred to as a realist or essentialist paradigm. The study adheres to the consolidated criteria for reporting qualitative research (COREQ) guidelines (20). The study complies with the principles of the Declaration of Helsinki and was approved by the Swedish Ethical Review Authority (Dnr: 2020-03046, 2020-0392). The purpose of the study was carefully presented to participants, and informed consent was obtained before participation. The results are being presented in 2 separate publications, which complement each other, but can also be read separately. The first paper (current) is descriptive and informative, while the second (Törnbom K et al. Back to life: Is it possible to be myself again? A qualitative study with persons initially hospitalized due to COVID-19. J Rehabil Med 2022) provides insight and a deeper understanding about life with persistent symptoms after COVID-19.
Participants
Persons hospitalized due to COVID-19 were recruited for the Life in the Time of COVID study in Gothenburg (GOT-LOCO) (21). The inclusion criteria of the GOT-LOCO study were: patients with COVID-19 who were admitted to hospital between July 2020 and February 2021 within the Västra Götaland region (9 units) in Sweden, non-contagious when enrolled, expected hospital care periods ≥ 5 days, ≥ 18 years old and previously lived independently. Patients were excluded for not being able to provide informed consent, having a comorbidity with a 1-year anticipated mortality (i.e. palliative care or metastatic cancer) or not being Swedish residents.
For the current study, a purposive sampling from the GOT-LOCO cohort was applied to recruit persons who had been discharged from hospital approximately 6 months previously, were 18–65 years old (working age) and who had persisting self-reported symptoms at a previously performed 3-month follow-up (part of the GOT-LOCO study), including respiration, mental health and functional status. The 3-month follow-up was a structured interview, using patient-reported outcome measures, conducted by phone (22). An invitation letter was sent to 21 persons based on the inclusion criteria, in order to achieve a heterogeneous sample based on age, sex, educational level, employment category and country of birth. Participants were contacted by phone and, upon agreement, a time for the interview was scheduled. Two of the contacted persons declined to participate, and 4 could not be reached despite several attempts. Based on current COVID-19 restrictions, participants could choose a phone/digital or a face-to-face interview.
A total of 15 persons agreed to participate (10 men, 5 women). The mean age was 57 years, and the median hospital stay was 16 days (Table I). Demographic data and data on the hospital stay were collected from the medical charts. The interview took place between 154 and 231 days after hospital discharge.
Data collection
Individual interviews were conducted by the first and second authors (ME and KT). ME is a woman, has a PhD in caring science, is a registered nurse, and has previous experience in performing qualitative studies. She performed the 3-month follow-ups by telephone with the GOT-LOCO cohort. KT is a woman, has a PhD in medicine, is a social scientist, has previous experience in performing qualitative studies but had no previous contact with the participants.
An interview guide was developed by 2 of the authors (HP and AP). HP is a woman, has a PhD in medicine, and is a physiotherapist. AP is a woman, has a PhD in medicine and is a physiotherapist with previous qualitative research methodology experience. AP and HP had no previous contact with the participants. The original guide was refined into a semi-structured interview guide with open-ended questions after discussions between all authors. The interview guide was discussed and revised in cooperation with 2 patient partners with lived experiences of COVID-19, 1 having been hospitalized due to COVID-19 and 1 having had long COVID-19 without needing inpatient care.
The interview guide was considered suitable after being tested in a pilot interview with the patient partner with experience of inpatient COVID-19 care. Fifteen interviews were performed in July and August 2021. Eleven were conducted over the phone, 2 were conducted as an online digital meeting and the remaining 2 were conducted at the rehabilitation medicine research facilities. Most interviews were performed individually with 1 researcher, but the interview at the research facility had both participants simultaneously. The duration of interviews ranged from 37 to 91 min. All interviews were audio-recorded and transcribed verbatim. No field notes were taken during the interviews. After 15 interviews, a low degree of new knowledge was obtained from new interviews, achieving data saturation. Experience and knowledge about qualitative research interviewing techniques were considered important prerequisites for conducting the interviews in the current study. Questions contained potentially sensitive topics, and to avoid as much psychological distress as possible, researchers proceeded through the questions with caution and respect. After the interview, the participants were encouraged to contact the interviewer with any questions or concerns; however, the transcribed interview was not given to the participant.
Data analysis
The wide range of symptoms that participants described after COVID-19 were summarized (see Table II-III). The symptoms were grouped if participants described similar symptoms. The transcribed interviews were analysed by inductive thematic analysis (19) due to its possibility to analyse participants described experiences and realities without any pre-existing theoretical framework. The themes presented in the results are strongly connected to the participants’ statements and provide a deeper understanding of participants lived experiences. First, the transcribed interviews were read and re-read independently by 2 authors (ME and AP; AP is well acquainted in the analysis, and ME with the data material, and their cooperation in the process increase the credibility) to become familiar with the text. In this process, initial codes were noted. Secondly, the same 2 authors coded the interviews together and searched for potential themes. The themes were then reviewed and refined by all 4 authors together, and differences were discussed until a consensus was reached for credibility of the analysis. The analysis process moved continuously back and forth between the whole and parts of the text to ensure the themes were representative of the data-set. Examples of the coding process are shown in Table III.
RESULTS
Three themes were identified, “Status of recovery – two steps forward, one step back”, “Remaining symptoms caused limitations in everyday life”, and “Strategies for recovery” illustrated in Fig. 1. The themes are illustrated with quotes from the participants.
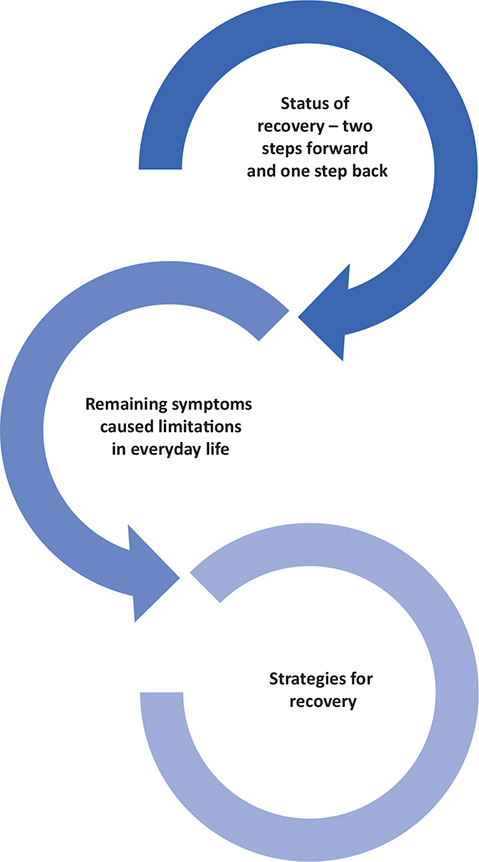
Fig. 1. The 3 separate main themes identified in the interviews 6 months after hospital discharge due to COVID-19. The themes identified were “Status of recovery – two steps forward, one step back”, “Remaining symptoms caused limitations in everyday life”, and “Strategies for recovery”, separate themes, but related.
Participants described in the interviews a wide range of symptoms 6 months after hospital discharge summarized in Table III. Symptoms involved several different organ systems and were often described as persisting since the acute phase or as fluctuating and new symptoms sometimes appearing over time. Some participants experienced no persistent symptoms from the initial infection of COVID-19 6 months after hospital discharge.
Status of recovery – two steps forward, one step back
Six months after being discharged from hospital, participants experienced setbacks and a lack of progress in recovery, which worried them about their future health. Others recovered quite well, in line with their expectations, and felt content. Overall, most of the participants’ experiences were characterized by motivation and hope for better future health.
Slow and fluctuating improvements involved frequent setbacks, which were triggered by going beyond one’s capacity, resulting in exhaustion and worsened symptoms. Setbacks were stressful and mentally difficult to handle, leaving participants crestfallen and worried about whether they would ever recover. COVID-19 vaccination was described as another trigger for setbacks, which could lead to worsened symptoms or re-onset of previous symptoms, especially symptoms relating to respiration. However, a slow recovery process was accepted by some subjects, who were patiently looking forward to being fully recovered.
“I could walk seven kilometres when I was feeling good, and I felt that now I was coming along…but then I crashed…sometimes you just want it so much”. (Participant 7, woman)
Additional complications due to COVID-19 could also mean setbacks in recovery. These involved, for example, embolisms, developing diabetes as a side-effect of treatments, worsening of previous chronic conditions and medical treatments for circulatory and cardiovascular conditions.
“So, I have a clots in my lungs, in my kidney and several more clots in my left and right foot. So, I take warfarin [medication]…it is awful, really”. (Participant 12, man)
On the other hand, some described health benefits after COVID-19 with regards to previous health conditions. These related to lifestyle changes with less stress in life, meaning lowered blood pressure and consequently needing less medical treatment.
“My blood pressure had been hard to keep down previously. I have had to take medication for this before, but this is something biologically interesting. I have actually been able to stop taking my blood pressure medicine since I came home from the hospital…when my work stress disappeared, that lowered my blood pressure”. (Participant 5, man)
Some described a fast physical recovery process. Although not being fully recovered, an unproblematic recovery process with continuous improvements that met expectations was perceived as positive. Everyday activities were not limited by impairments, and physical activity habits were back to normal.
“My stamina is still a little worse than before…I would say about 75% compared to before [COVID]…but I am working on it”. (Participant 6, man)
Remaining symptoms caused limitations in everyday life
Many daily life activities were affected as a consequence of impairments. Fatigue and lack of energy was especially troublesome when trying to manage everyday life. Participants expressed overwhelming fatigue as limiting their participation in family activities, such as parental responsibilities and being there for other family members. Depending on the participant’s age and family situation, different situations were described as challenging. Participants with school-aged children described not being able to participate actively with or support their children as before. Participants with grandchildren described their limitations and grief of not coping to take care of or even interact with them.
“I have a son who plays soccer. I cannot watch his games any longer. I can’t cope because it is always too much going on there”. (Participant 14, woman)
Participants avoided social activities, and this led to loneliness and isolation. Some described being too tired to accept invitations or not having enough energy to host social activities, as they were used to doing before the infection. In addition, some were afraid of being re-infected and stopped socializing in order to protect themselves and others from the disease. The avoidance of social activities was often difficult for friends and acquaintances to understand and accept, and participants described being perceived as asocial.
“I am used to working and socialising with people, but now I just sit at home and do nothing, I don’t feel like doing anything”. (Participant 10, man)
Trying to manage household chores was described as strenuous, leading to exhaustion and frustration. Shortness of breath made it difficult to carry out household chores, such as making the bed, vacuuming, and doing the dishes. Participants described having to take frequent pauses to rest, resulting in chores having to be extended over longer periods of time, sometimes over several days. Grocery shopping was described as demanding, not having the stamina to walk to the grocery store or to remember what to buy led to feelings of frustration. Not coping with chores also brought feelings of guilt.
“I pant just like a horse when I lean over to make the bed. So, after I’ve made the bed and put all the pillows on, then I sit down to rest. But once I have sat, the panting disappears rather quickly”. (Participant 7, woman)
Due to impairments related to the infection, leisure activities were set aside to save energy for activities that were considered to be of higher priority and were sometimes difficult to carry out. Participants described prioritizing their time and energy on rehabilitation and healthcare visits, not having spare energy for hobbies or leisure. Some described not being able to ride their bikes due to impaired balance and being prohibited from driving due to impairments related to their infection. Refraining from enjoyable activities meant a loss of inspiration and meaning, sometimes leading to feelings of melancholy.
“I spend so much more time at home. I had had a quite active life before…I have been doing martial arts, and we trained there two times a week…I can´t really do that type of training now. It´s a little too tough as it is right now”. (Participant 5, man)
Strategies for recovery
Participants described structuring their everyday life and setting up routines to manage their days. This included planning and structuring activities (e.g. getting up at a specific time, doing 1 thing at a time and alternating between rest and activity) to manage throughout the day. One way to cope with strenuous household chores was to sit down during the activity to conserve energy. To create meaning in everyday life, participants described engaging in creative activities, such as sewing, handcraft, or outdoor recreation.
“I break it down so that I can cope with it so that I don’t totally exhaust myself. This is how I go about it, I put the timer on 45 minutes, and then I start vacuuming and all and then, when the timer goes off, then I take a break to rest for a while”. (Participant 12, man)
Setting limits for and adjusting expectations of one’s own stamina was another strategy, where this change in attitude towards doing activities made it possible to avoid exhaustion. Participants expressed having received advice to conserve their energy, which they tried to follow. Some asked others for help with household chores or accepted offers of help from others, which was somewhat a new experience.
“Firstly, lower my expectations on what to achieve. Secondly, accept help [from others]. So, to be honest with others about how I feel and how it is and to say “now I am tired” or “no, it isn’t going to work to do three activities on Saturday, we need to take one thing at a time”. (Participant 5, man)
Participants expressed using physical activity to regain strength and to feel better. Knowledge and experience of the physical and mental benefits motivated participants to try and be physically active although it was often perceived as challenging due to their condition. Taking a walk, going to the gym, working out at home, cycling or gardening were described as manageable by some, whereas others were worse off and challenged themselves to, for example, stand up for more than 5 min. Strenuous activities, such as jogging, were often replaced with less vigorous activities, such as walking or cycling.
“Well, I have been thinking that when it comes to my physical health, so I have thought about trying to recover as soon as possible, and when it comes to my mental fatigue, I have realised that it is connected. My only strategy was to go out in the fresh air and take walks, powerwalks, and hang out with people”. (Participant 6, man)
To make life work despite memory and concentration difficulties, participants put creativity and effort into structuring their lives. This was in order to manage and be able to function together with others, family, friends and with colleagues. To cope, participants used the reminder function on the mobile phones, pill organisers, memory notes, and they noted they were careful to put things back in the same place to find them later more easily. To cope with concentration difficulties, one strategy was to focus only on 1 task at a time, which also reduced the risk of exhaustion.
“It is likely my short-term memory that is the worst. If I read something and try and repeat it, then I don’t remember much at all…I just have to write everything down if I need to do something, for example, if want to buy groceries”. (Participant 4, woman)
Social activities were important for recovery, but were at the same time tiring, and structuring social activities was essential for being able to participate. Planning to spend time with friends and family was difficult, as it was difficult to predict how they would feel, and the interaction could mean being tired for several days. Limiting the duration of social activities, not meeting too many persons at the same time and prioritizing socializing with friends who were understanding were described as important coping strategies. Having conversations with others who had the same illness, problems and reactions was perceived as positive for their recovery and led to an increased understanding of their own experiences.
“Well, I just can’t cope, and then I prioritize hanging out with my close friends where I can lay on sofa or where I know that it is completely OK to lay down and rest a little”. (Participant 8, woman)
DISCUSSION
Three themes were identified: “Status of recovery – two steps forward, one step back”, “Remaining symptoms caused limitations in everyday life”, and “Strategies for recovery”. The themes revealed that the recovery process up until at least 6 months after discharge from hospital was a rocky and uncertain road often involving setbacks. A wide range of persistent, fluctuating or newly emerging symptoms had negative consequences for many areas of daily life. Participants described a wide range of symptoms after COVID-19 that affected their everyday life. Prominent symptoms were fatigue, depression, anxiety and isolation as well as emotional distress. Participants stated that they used a variety of strategies to manage everyday life activities and to recover. The results confirm findings from previous studies (3, 10) investigating patient experiences of the recovery period 6 months after COVID-19.
The results need to be interpreted bearing in mind that all participants in the current study had been hospitalized in infectious control departments, special COVID-19 wards, or the intensive care unit (ICU) for severe illnesses. Being seriously ill and being cared for in critical care in itself contribute to residual problems that might negatively affect person’s daily lives. Similar persistent symptoms in the current findings were reported in a previous study in which 80% of patients treated for COVID-19 in the ICU for acute respiratory failure with mechanical respiration also developed post-intensive care syndrome (PICS) (15). PICS meant worsened physical, cognitive and/or mental health problems after discharge from hospital (15). In another study (10), ICU admission was an independent risk factor for post-COVID-19 symptoms, indicating that persistent symptoms following COVID-19 could be from the critical care or the COVID-19 infection, and that PICS could mean further long-term consequences in addition to the COVID-19-related symptoms (15). Previous research (18, 23, 24) also highlighted that persistent symptoms similar to our findings occurred even after mild COVID-19 for some non-hospitalized persons, indicating post-COVID-19 is a challenge for many individuals, the healthcare system and society overall, regardless of the severity of the initial COVID-19 infection (25).
Recent studies showed that persistent symptoms affected participants’ everyday life (26) and showed that a holistic perspective needs to be undertaken in the rehabilitation process to fully understand the complex situation for patients living with persistent symptoms after COVID-19. The current results, in agreement with previous research (27), shows that patient health conditions strongly impair functioning, where activities and participation are limited after COVID-19. Hence, family, friends and society are also impacted. A holistic approach is crucial in rehabilitation, which means that interdisciplinary teams should jointly develop strategies for managing post-COVID-19 care (3, 14).
The findings of the current study demonstrate that participants coped with persistent symptoms after COVID-19 in various ways. Some looked forward to their future recovery; whereas others were not sure if they would ever get well. Managing distress seemed to depend on the patients’ capacity to develop coping strategies to navigate their everyday life in this novel situation (3). In the present study, the results showed that several different coping strategies were used. The prominent strategy was the problem-focused coping strategy (PFC) (28), which was seen in the strategies for recovery theme. This was evident when the participants described how they creatively and actively planned and structured their daily activities and varied these with rest. Thus, they were able to manage their daily lives to some extent despite their fragile health. They became experts about their own body and learned to what extent they could exert themselves and what was the most effective way to recover. Small adjustments in everyday life, such as sitting while peeling potatoes, allowed them to complete housework.
Physical activity was another strategy for recovery that was highlighted. The participants wished to get back to normal life again and recognized that their bodies were important. The deteriorating physical condition led to feelings of a loss of “self” and that their identity changed. Similar findings were presented in another study (26), in which researchers found that physical activity was perceived as important enough that participants were willing to risk setbacks after physical activity to feel normal for a while. Using PFC strategies allowed participants to live their lives in their homes, and some were even able to work despite their limitations.
Another described setback that has rarely been described in previous research was the experiences of deteriorating health and reinfection symptoms in relation to COVID-19 vaccination. Participants found this type of setback particularly frustrating, as they felt they were back to square one again despite a strenuous month-long rehabilitation programme.
The reactions and experiences in relation to slow and fluctuating improvements meant residual feelings of frustration, anxiety and sadness. This is similar to findings from another study (29) investigating inpatients’ post-acute psychological experiences, in which anxiety, demoralization, acute stress, depression and grief were the most commonly noted. In the current study, participant strategies seldom linked to emotion-focused coping strategies. It did not appear that they had processed their feelings related to their new health situation, which could have influenced the emotional experiences and reactions they reported. There can be several reasons for this: the participants’ personality, repeating previous coping strategies and available and effective PFCs were utilized. Furthermore, since the interviews were conducted only 6 months after discharge from hospital, it may have been too short a period to process a new life situation, further influencing the chosen coping strategies. Previous research (30, 31) has shown that recovery after a critical illness can require 2 years or longer. In 1 study (32), the patient coping strategy choice for patients in an acute and in a remitted phase of COVID-19 was found to be predominantly PFCs during the acute phase of the illness, indicating that other coping strategies may be chosen later.
Participants clearly used seeking a social support coping strategy (SSCS) (33), but it was complex, as this strategy was affected by the nature of the recovery process, the protracted period of the illness and the lockdowns. The results of the current study show the need and value of social interaction with family but also friends and others they met in society to facilitate their recovery process. However, several factors made social contact more difficult, especially the participants’ fragile health, including fatigue, powerlessness and need for isolation. In previous research (34), the COVID-19 pandemic was compared with other difficult situations, such as natural disasters, in which SSCS is a common utilized coping strategy. However, the nature of the pandemic impacted this, as many were forced to isolate to protect themselves and/or family members. Findings from the present study highlight how isolation coupled with fragile health leads to feelings of loneliness and reduced participation in activities, such as sports, culture and shopping, negatively impacting the quality of life. These results could be used to develop tailored care and rehabilitation and improved support for persons living with post-COVID-19.
The participants in the current study were a heterogeneous selected group of patients of working age (18–65 years) who had persistent self-reported symptoms, including respiration, mental health and limited functional status. This sample made it possible to obtain valuable descriptions and experiences from a small group with symptoms that severely limit their daily life. As the number of participants in the study was small, results should be cautiously extrapolated. However, the current findings are consistent with previous research, increasing generalizability to other groups with persistent symptoms after COVID-19 symptoms.
Future research should investigate individual experiences of the recovery process due to persistent symptoms after COVID-19 and how it is affecting everyday life longitudinally. The discussed coping strategies, such as self-care methods, may also be important to explore, as these may help a large group of persons in society dealing with complex situations from persistent symptoms after COVID-19.
In conclusion, the current study increases our knowledge of the field, based on the individuals’ experiences. This information could be important to tailor care and rehabilitation for persons with persistent symptoms after COVID-19. When creating a safe and person-centred rehabilitation environment, it is important to learn more about how to approach and support patients with persistent symptoms after COVID-19. An interdisciplinary follow-up may be necessary, as the patterns of recovery are diverse. Unexpected symptoms in the recovery process were described and not always possible to forecast. Furthermore, COVID-19 is a new illness and phenomenon in society, and the challenges of the recovery phase have been largely unexplored.
ACKNOWLEDGEMENTS
We would like to thank our patients’ partners, Helena Strömberg and Tomas Angervik, for their knowledgeable contributions to the research question, interview guide and in discussing the results.
This study was funded by grants from the Swedish government under an agreement between the Swedish government and the county councils (ALF 73750, ALFGBG-942914), Forte/Formas (2020-02775), Vastragotaland regional research funding (VGFOUREG-940508, VGFOUREG-969267), the Sahlgrenska University Hospital research funds (SU-961051).
REFERENCES
- Roth PH, Gadebusch-Bondio M. The contested meaning of “long COVID” - Patients, doctors, and the politics of subjective evidence. Soc Sci Med 2022; 292: 114619.
- World Health Organization. Coronavirus disease (COVID-19): Post COVID-19 condition. 2021 20220429 [cited 2022 May 1]. Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 2021; 11: 16144–16144.
- Nasserie T, Hittle M, Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: A Systematic Review. JAMA Netw Open 2021; 4: e2111417.
- Galal I, Hussein AARM, Amin MT, Saad MM, Zayan HEE, Abdelsayed MZ, et al. Determinants of persistent post-COVID-19 symptoms: value of a novel COVID-19 symptom score. The Egypt J Bronchol 2021; 15: 10.
- Wahlgren C, Divanoglou A, Larsson M, Nilsson E, Östholm Balkhed Å, Niward K, et al. Rehabilitation needs following COVID-19: Five-month post-discharge clinical follow-up of individuals with concerning self-reported symptoms. EClinicalMedicine 2022; 43: 101219.
- Ghosn J, Piroth L, Epaulard O, Le Turnier P, Mentré F, Bachelet D, et al. Persistent COVID-19 symptoms are highly prevalent 6 months after hospitalization: results from a large prospective cohort. Clin Microbiol Infect 2021; 27: 1041.e1041–1041.e1044.
- Munblit D, Bobkova P, Spiridonova E, Shikhaleva A, Gamirova A, Blyuss O, et al. Incidence and risk factors for persistent symptoms in adults previously hospitalized for COVID-19. Clin Exp Allergy 2021; 51: 1107–1120.
- Schiavi M, Fugazzaro S, Bertolini A, Denti M, Mainini C, Accogli MA, et al. “Like before, but not exactly”: the Qualy-REACT qualitative inquiry into the lived experience of long COVID. BMC Public Health 2022; 22: 599.
- Peghin M, Palese A, Venturini M, De Martino M, Gerussi V, Graziano E, et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin Microbiol Infect 2021; 27: 1507–1513.
- Poudel AN, Zhu S, Cooper N, Roderick P, Alwan N, Tarrant C, et al. Impact of Covid-19 on health-related quality of life of patients: A structured review. PLoS One 2021; 16: e0259164–e0259164.
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). 2001 [cited 2022 May 1]. Available from: http://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf;jsessionid=581383C8A6450C19251CEF7BAAA6349B?sequence=1.
- Patel K, Straudi S, Yee Sien N, Fayed N, Melvin JL, Sivan M. Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks. Int. J. Environ. Res. Public Health 2020; 17: 6476.
- Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med 2021; 9: 1275–1287.
- Vrettou CS, Mantziou V, Vassiliou AG, Orfanos SE, Kotanidou A, Dimopoulou I. Post-Intensive Care Syndrome in Survivors from Critical Illness including COVID-19 Patients: A Narrative Review. Life (Basel) 2022; 12.
- Santiago-Rodriguez EI, Maiorana A, Peluso MJ, Hoh R, Tai V, Fehrman EA, et al. Characterizing the COVID-19 Illness Experience to Inform the Study of Post-acute Sequelae and Recovery. Int J Behav Med 2021; 10.1007/s12529-021-10045-7: 1–14.
- Macpherson K, Cooper K, Harbour J, Mahal D, Miller C, Nairn M. Experiences of living with long COVID and of accessing healthcare services: a qualitative systematic review. BMJ Open 2022; 12: e050979.
- Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv Res 2020; 20: 1144.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357.
- Larsson AC, Palstam A, Persson HC. Physical function, cognitive function, and daily activities in patients hospitalized due to COVID-19: a descriptive cross-sectional study in Sweden. Int J Environ Res Public Health 2021; 18.
- Larsson AC, Engwall M, Palstam A, Persson HC. Self-assessed aspects of health 3 months after COVID-19 hospitalization – A Swedish cross-sectional study. Int J Environ Res Public Health. 2022; 19 (13).
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. Bmj 2020; 370: m3026.
- Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network – United States, March–June 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 993–998.
- Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post COVID-19 condition or long COVID: a meta-analysis and systematic review. J Infect Dis 2022; 10.1093/infdis/jiac136.
- Humphreys H, Kilby L, Kudiersky N, Copeland R. Long COVID and the role of physical activity: a qualitative study. BMJ Open 2021; 11: e047632.
- Zhang H, Xie F, Yang B, Zhao F, Wang C, Chen X. Psychological experience of COVID-19 patients: a systematic review and qualitative meta-synthesis. Am J Infect Control 2022; 10.1016/j.ajic.2022.01.023.
- Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. 1987; 1: 141–169.
- Rossi Ferrario S, Panzeri A, Cerutti P, Sacco D. The psychological experience and intervention in post-acute COVID-19 inpatients. Neuropsychiatr Dis Treat 2021; 17: 413–422.
- Bergbom I. The process of recovery from severe illness, injury or surgical treatment. Recent Adv Res Updat 2008; 9: 413–431.
- Fan E, Dowdy DW, Colantuoni E, Mendez-Tellez PA, Sevransky JE, Shanholtz C, et al. Physical complications in acute lung injury survivors: a two-year longitudinal prospective study. Crit Care Med 2014; 42: 849–859.
- Dehelean L, Papava I, Musat MI, Bondrescu M, Bratosin F, Bucatos BO, et al. Coping strategies and stress related disorders in patients with COVID-19. Brain Sci [Internet]. 2021 2021/09//; 11 (10).
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull 2003; 129: 216–269.
- Polizzi C, Lynn SJ, Perry A. Stress and coping in the time of Covid-19: pathways to resilience and recovery. Clin Neuropsychiatr 2020; 17: 59–62.