ORIGINAL REPORT
PSYCHOLOGICAL DISTRESS, PAIN AND INSURANCE CLAIMS NEGATIVELY AFFECT LONG-TERM HEALTH-RELATED QUALITY OF LIFE AFTER ROAD TRAFFIC INJURIES
Kevin K. C. HUNG, MPH1, Annette KIFLEY, PhD2, Katherine BROWN, PhD3, Jagnoor JAGNOOR, PhD2,3, Ashley CRAIG, PhD2, Belinda GABBE, PhD4, Sarah DERRETT, PhD5, Alex COLLIE, PhD4, Michael DINH, PhD6, Bamini GOPINATH, PhD2,7 and Ian D. CAMERON, PhD2 on behalf of the FISH Investigators
From the 1Accident and Emergency Medicine Academic Unit, Chinese University of Hong Kong, Hong Kong, 2John Walsh Centre for Rehabilitation Research, Kolling Institute, Northern Sydney Local Health District, Sydney Medical School Northern, St Leonards, NSW, 3The George Institute for Global Health, University of New South Wales, Sydney, 4School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia, 5Injury Prevention Research Unit (IPRU), Preventive & Social Medicine, Dunedin, New Zealand, 6Royal Prince Alfred Hospital, The University of Sydney, Sydney and 7Macquarie University Hearing, Department of Linguistics, Macquarie University, NSW, Australia
Objective: A prospective cohort study to investigate how injury and early post-injury psychosocial factors influence health outcomes 12 months after road traffic injury.
Methods: Residents of New South Wales, Australia, with road traffic injury in the period 2013–16 were recruited. Explanatory factors were evaluated for outcomes over 12 months using 12-Item Short Form Survey (SF-12) Physical and Mental Component Scores (PCS and MCS). Path models and mediation analysis were used to examine the effect of injury severity and explanatory factors.
Results: SF-12 PCS and MCS outcomes were poorer among participants with baseline psychological distress, for all injury severities (β coefficients –3.3 to –9.3, p < 0.0001). Baseline pain and psychological distress, and baseline PCS and MCS were each involved in indirect effects of injury severity on 12-month PCS and MCS. Injury severity, baseline PCS and MCS, and baseline psychological distress were also associated with the likelihood of a compulsory third-party insurance claim, and claiming was negatively associated with 12-month PCS and MCS outcomes (beta coefficients –0.22 and –0.14, respectively, for both, p < 0.01).
Conclusion: Baseline factors, including pain, psychological distress and lodging a compulsory third-party insurance claim, negatively impact long-term physical and mental health status following road traffic injury, emphasizing the importance of early screening and intervention.
Trial registration: Australia New Zealand Clinical trial registry identification number: ACTRN12613000889752.
LAY ABSTRACT
Road traffic injury (RTI) can lead to adverse long-term physical and mental health outcomes. This study followed participants with RTI for 12 months to assess the effects of acute post-injury psychological distress and physical and mental health outcomes. For physical health outcomes, greater severity of injury leads directly to a more restricted physical state; pain and psychological distress soon after injury also contribute to negative physical outcomes for participants experiencing more severe injuries. For mental health outcomes, injury severity has no direct effect on worsening mental state; mental state and psychological distress soon after injury leads to worsening outcomes for participants experiencing more severe injury. Individuals with higher psychological distress or pain were more likely to lodge a motor vehicle insurance claim. These people had subsequently poorer 12-month physical and mental health outcomes. It is essential to understand how early screening and interventions for psychological distress and pain can affect recovery.
Key words: injury severity; psychological status; mediators; path analysis.
Citation: J Rehabil Med 2022; 54: jrm00310. DOI: http://dx.doi.org/10.2340/jrm.v54.30.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: May 19, 2022; Epub ahead of print: Jun 23, 2022; Published: Jul 5, 2022
Correspondence address: Ian D. Cameron, John Walsh Centre for Rehabilitation Research, Sydney Medical School Northern, Level 13, Kolling Building, St Leonards, NSW, Australia. E-mail: ian.cameron@sydney.edu.au
Competing interests and funding: The authors declare that they have no competing interests.
The study is funded by the Motor Accidents Authority (now known as the State Insurance Regulatory Authority) of New South Wales, Australia. The funder participates in the Steering Group for the study, but has no direct involvement with the scientific aspects of the study.
Morbidity arising from a road traffic injury (RTI) is a very serious problem, and age-standardized incidence rates of RTI increased between 1990 and 2017 (1). Globally, the number of motor vehicles increased from 0.85 billion in 2000 to 2.1 billion in 2016; despite this increase the rate of death decreased from 135 to 64 deaths per 100,000 vehicles over the same period (2). The increase in morbidity from RTI poses a huge challenge for health systems worldwide. Variations in functional outcomes have been found within groups with similar levels of injury severity, suggesting that a range of individual, secondary and social characteristics contribute to poor outcomes following RTI (3–4).
For people experiencing major trauma, recent research from Europe and Australia has found that functional outcomes, health status and return to work status are suboptimal after 2–5 years (4–6). Longitudinal studies of trauma patients have revealed that psychological factors, including emotional and cognitive perceptions, are negatively associated with functional outcomes following head injury (7) and lower extremity trauma (8).
The prevalence of psychopathology following injury was estimated to be 10–30% for post-traumatic stress disorder (PTSD), 6–42% for depression, and 4–24% for post-trauma anxiety disorders (9). Whiplash-associated disorder, spinal cord injury and mild-to-moderate traumatic brain injury have been found in a meta-analysis to be associated with elevated risk of psychological distress (10). Previous studies found that the prevalence of depression and anxiety tends to decline over the first few months following a traumatic event (11–12). Furthermore, the temporal sequencing of physical and mental health outcomes following RTI is complex (13). Survivors of major trauma could also have changing frames of reference, with what is known as the disability paradox (14).
The Factors Influencing Social and Health outcomes after motor vehicle crash injury (FISH) study is an inception cohort study including persons injured with varying injury severities, both hospitalized and non-hospitalized (15). Our previous study found increasing injury severity had a significant negative effect on the 12-Item Short Form Survey (SF-12) Physical Component Summary (PCS) and Mental Component Summary (MCS) scores at 12 months after injury. Using mediation analyses, baseline SF-12 scores, baseline pain, baseline psychological status and compulsory third-party (CTP) insurance claimant status were all involved in indirect pathways of effect of injury severity on 12-month SF-12 PCS and SF-12 MCS (16). Based on this previous work, the current study hypothesis is that injury severity affects 12-month SF-12 PCS and MCS through several pathways, and the aim of this study is to quantify the mediating factors involved.
METHODS
Inclusion and exclusion criteria
The FISH study recruited adult residents in New South Wales (NSW), Australia, who were injured in RTI between August 2013 and December 2016. Detailed methods for the FISH study have been published elsewhere (15). Participants included injured drivers, riders, passengers, pedestrians or cyclists involved in a motor vehicle crash. Participants were excluded if they had pre-existing cognitive impairment, or if they had severe traumatic brain injury, spinal cord injury, extensive burns or multiple amputations. Participants with injury due to self-harm, or those with minor isolated superficial soft-tissue injuries, such as bruises, abrasions or cuts, were also excluded.
Study design
Most participants were recruited from hospital emergency departments (5% from other sources) and were contacted within 28 days of injury by telephone to obtain baseline information. Interviews were conducted using computer-aided telephone interview by trained interviewers.
Participants were divided into 3 groups of injury severity according to their self-reported length of hospital stay (LOS), with mild injury defined as participants with LOS of 1 day or less (including participants who did not present or who were not admitted to hospital), moderate for participants with LOS 2–6 days and severe with LOS ≥ 7 days. The use of LOS as injury severity measure has been common practice (17) and this LOS cut-off has been reported previously (and is strongly correlated with Injury Severity Score) (16). Participants were assessed using a structured interview at baseline, and again at 6 and 12 months after injury.
Outcome measures
The primary outcomes were 12-month SF-12 Mental and Physical health Component Summary Scores (MCS and PCS, respectively) (18). The SF-12 is one of the most commonly used measures of health-related quality of life and utilizes 12 questions to derive the PCS and MCS (18). PCS and MCS at baseline post-injury were considered in the path modelling and mediation analyses. The FISH study used the acute form of the SF-12 questionnaire, which instructs the participants to recall the past week.
Key explanatory factors included baseline presence of pain and pain severity (numerical rating scale; NRS) (19), pain catastrophizing (Pain Catastrophizing Scale) (20), psychological status (Impact of Events Scale (21) and the Depression, Anxiety and Stress Scale (22)) and CTP insurance claimant status.
NRS for pain is a unidimensional measure of pain intensity in adults (19). The Pain Catastrophizing Scale is one of the most widely used instruments to measure catastrophic thinking related to pain and has been validated (20). We define high baseline pain catastrophizing as Pain Catastrophizing Scale >30 based on the recommendation by Sullivan (20). Impact of Events Scale-revised (IESR) is a validated measure for post-traumatic stress symptoms (21), and we define IESR ≥4.5 (out of 12) as high baseline IESR. Depression, Anxiety and Stress Scale 21 (DASS21) is a validated scale for negative emotional states of depressive mood, anxiety and stress (22), and we define DASS21 ≥ 30 at baseline post-injury as high baseline DASS (23). The cut-off scores of IESR and DASS21 were based on a previous study that established a cut off with reasonable sensitivity and specificity when detecting major depressive disorder and PTSD (23).
CTP insurance protects the driver from liability if they were to cause the death of or injure people in a motor vehicle crash, and is a requirement in NSW, Australia before motor vehicle drivers can register their vehicle. The insurance pays for the treatment and care of the injured, the loss of income, and the damages claim lodged. CTP insurance does not cover the cost of damaged vehicles or property, nor claims from drivers who were charged with serious driving offences. CTP claims need to be lodged within 6 months of the motor vehicle crash (24).
The study was conducted according to the Declaration of Helsinki and approved by the Central Sydney (Concord Hospital) Local Health District Human Research Ethics Committee.
Statistical analyses
Statistical analyses were performed using SAS v 9.4 (SAS Institute Inc., Cary, NC, USA) and MPLUS Version 7.3 (Muthén & Muthén, Los Angeles, CA, USA). First, linear mixed models were used to evaluate baseline pain and psychological distress (high DASS21, high IES-R and high pain catastrophizing) and CTP claimant status as explanatory factors for SF-12 PCS and MCS outcomes 12 months after the injury among individuals with mild and moderate-severe injury.
Effects of baseline pain were adjusted for recruitment source, pre-injury factors, and crash and injury factors. Effects of baseline psychological factors and CTP claimant status were adjusted for recruitment source, pre-injury factors, crash and injury factors, baseline pain and other baseline psychological factors. Where effects were identified, the presence of associations at the initial baseline post-injury time-point and the impact of additional adjustments are also noted.
The pre-injury covariables included were age group, sex, pre-injury paid work or self-employment, pre-injury social satisfaction, pre-injury educational level, pre-injury physical comorbidities (25), pre-injury anxiety or depression (25), and pre-injury EQ-5D-3L time trade-off (TTO) summary score derived using Australian-derived time-trade-off weights (26). Crash and injury-related covariables included were perceived danger and crash type.
Secondly, the current study examined the involvement of baseline psychological status, baseline pain severity and CTP claimant status in different pathways of effect of injury severity on 12-month SF-12 PCS and MCS outcomes. Initial baseline SF-12 PCS and MCS were also considered in the path models. For each step of the pathway, effects were estimated after adjusting for all pre-injury factors using the STDY standardization option.
In this paper we use the term “effect” in its statistical sense when discussing estimates from the linear mixed models and path analyses. We have applied causal inference principles in considering the temporal ordering events and to guide analyses based on regression adjustment for antecedent and coincident factors. However other covariables may be relevant which it was not possible to consider in the current analyses, therefore it is still possible that effects identified are not causal.
RESULTS
Of the 2,019 recruited participants, 2,018 provided self-reported hospital LOS, and 1,201 (60%) completed the 12-month follow-up. Table I shows pre-injury, crash and baseline factors by injury severity group. Longer hospital stay (LOS ≥ 7 days) was associated with older age (p < 0.0001), male sex (p < 0.0001), lower education level (p < 0.0001), rural hospital recruitment (p < 0.0001), being an unprotected road user (i.e. not a vehicle occupant, with the exception of being a bicyclist) (p < 0.0001) and claiming compensation (p < 0.0001).
Individuals with higher injury severity had worse PCS scores at all stages of the study (p < 0.0001). Even though the 6- and 12-month MCS scores were significantly lower with longer hospital LOS (p = 0.003 at 6-months and 0.02 at 12-months), the difference in MCS scores between the groups was small (Fig. 1).

Fig. 1. Unadjusted 12-Item Short Form Survey (SF-12) Physical and Mental Component Scores (PCS and MCS) at baseline, 6 and 12 months with different lengths of stay (LOS). 95% CI: 95% confidence interval. FISH: Factors Influencing Social and Health outcomes after motor vehicle crash injury study.
Injury severity and explanatory factors for 12-month SF-12 PCS and MCS outcomes
Table II shows the strength of association between the explanatory factors baseline pain, baseline psychological distress and CTP claimant status, and 12-month SF-12 PCS and MCS outcomes, after adjustment for covariables.
Consistent negative effects of CTP claimant status (beta estimate –5.0 to –5.1), baseline DASS21 (beta estimate –4.5 to –5.7), IESR (beta estimate –4.5 to –6.9), pain catastrophizing (beta estimate –7.7 to –7.8), and baseline pain rating of 4 or more (beta estimate –4.2 to –5.2) were seen on SF-12 PCS at 12-months post-injury. These effects were all similar to those seen among participants with milder injuries.
Consistent negative effects of baseline DASS21 (beta estimate –11.3 to –11.6), IESR (beta estimate –5.8 to –6.3), and pain catastrophizing at baseline (beta estimate –6.3 to –9.7) were found for SF-12 MCS at 12-months after all adjustments. These effects were all similar to those seen among individuals with milder injury, except that pain catastrophizing did not have a significant effect in the group with milder injury. CTP claimant status was also associated with 12-month SF-12 MCS (beta estimate –7.8 for LOS 7+ days and –2.3 for LOS ≤ 1 day). Baseline pain rating of 4 or more (beta estimate –4.2 for LOS 2–6 days and –3.0 for LOS ≤ 1 day) was associated with 12-month SF-12 MCS before, but not after, adjusting for other post-injury factors.
Fig. S1 shows the combined effect of increasing injury severity and baseline psychological distress on SF-12 PCS and MCS outcomes, using the example of high baseline DASS21.
Pathways of effect of injury severity on SF-12 PCS and SF-12 MCS
Considering SF-12 PCS 12 months after injury as the health outcome for people with moderate to severe injuries, the path analysis shows that initial injury severity and initial PCS have the main direct effects on this health outcome (Fig. 2). Increasing injury severity directly and negatively affected SF-12 PCS at baseline post-injury, with additional indirect effects mediated by increased baseline pain and pain severity, and, to a lesser extent, pain catastrophizing. Baseline SF-12 PCS was strongly associated with SF-12 PCS 12 months post-injury. Severe injury (LOS ≥ 7 days) had additional direct negative effects on SF-12 PCS at 12-months over and above those seen at baseline. Smaller indirect negative effects of injury severity on SF-12 PCS at 12 months were found to operate through baseline pain and pain severity, CTP claimant status and baseline psychological factors and/or SF-12 MCS.
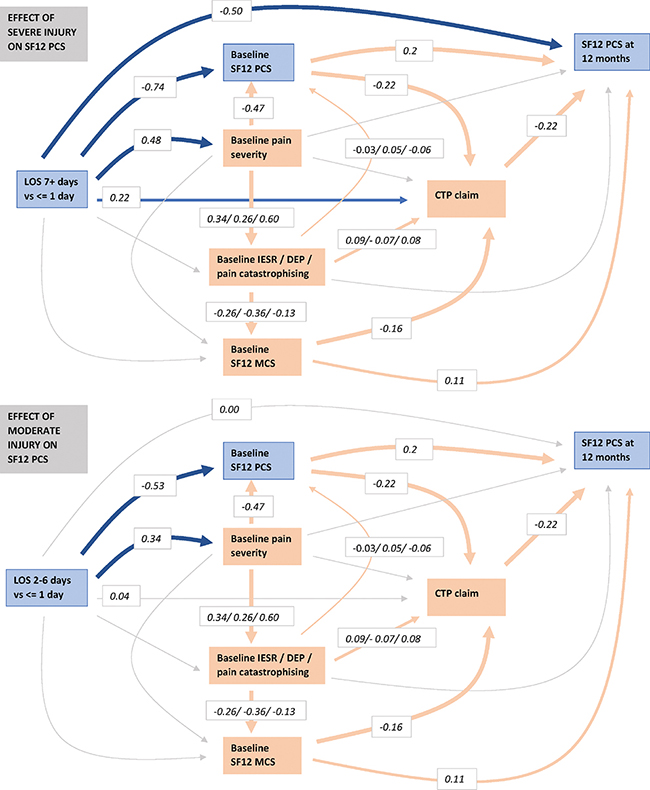
Fig. 2. Path models for 12-Item Short Form Survey (SF-12) Physical Component Score (PCS) at 12 months. Each step in the pathway has been adjusted for pre-injury factors.
IESR: Impact of Events-Revised Scale; PCS: Physical Component Summary score; MCS: Mental Component Summary score; CTP: Compulsory Third Party; LOS: Length of hospital stay; DEP: DASS-21 Depression Subscale Score.
Beta coefficient estimates based on STDY standardization. Blue or orange arrows of 4-point width represent p<0.0001. Blue or orange arrows of 2.5-point width represent p<0.01.
Blue or orange arrows of 1-point width represent p<0.05. Light grey arrows of 0.5-point width represent p≥0.05.
Severe injury, baseline physical health status, baseline psychological status and baseline SF-12 MCS all affected whether a CTP insurance claim was made, which then had a negative effect on SF-12 PCS at 12 months.
Considering the SF-12 MCS as the health outcome for people with moderate-to-severe injuries, the current study found that increasing injury severity did not directly affect baseline or long-term MCS. Rather, the effects of injury severity on MCS related to PCS, pain and baseline psychological status (Fig. 3).
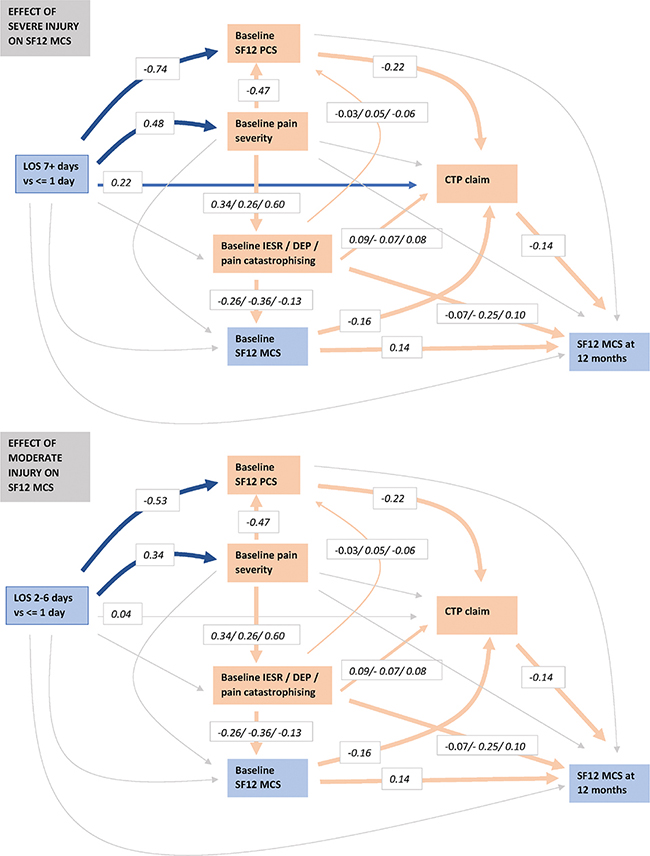
Fig. 3. Path models for 12-Item Short Form Survey (SF-12) Mental Component Score (MCS) at 12 months. Each step in the pathway has been adjusted for pre-injury factors. Beta coefficient estimates based on STDY standardization. Blue or orange arrows of 4-point width represent p<0.0001. Blue or orange arrows of 2.5-point width represent p<0.01. Blue or orange arrows of 1-point width represent p<0.05. Light grey arrows of 0.5-point width represent p≥0.05.
IESR: Impact of Events-Revised Scale; PCS: Physical Component Summary score; MCS: Mental Component Summary score; CTP: Compulsory Third Party; LOS: Length of hospital stay; DEP: DASS-21 Depression Subscale Score
Increasing injury severity indirectly and negatively affected SF-12 MCS at baseline post-injury through associations between increased baseline pain and pain severity and baseline psychological status. Baseline SF-12 MCS was strongly associated with SF-12 MCS at 12-months post-injury. Baseline psychological status also directly affected SF-12 MCS at 12-months, over and above its early effect on baseline SF-12 MCS.
Smaller indirect negative effects of injury severity on SF-12 MCS at 12 months were found to operate through CTP claimant status and baseline SF-12 PCS. Severe injury, baseline physical health, baseline psychological status and baseline mental health status all affected whether a CTP insurance claim was made, and that then had a negative effect on mental health outcome.
DISCUSSION
This study demonstrated that baseline pain and baseline psychological factors played an important role in long-term recovery after sustaining a moderate-severe RTI. This is a new finding and extends what is known about their influence on recovery after mild injury (27). Poorer long-term recovery in PCS was seen among individuals with poorer initial psychological reaction to injury across all levels of injury severity. Furthermore, innovative path modelling suggested that baseline psychological factors are involved via multiple pathways in longer-term negative effects of increasing injury severity, both for PCS and MCS of the SF-12. These effects include, but are not limited to, differences in insurance claiming behaviour, whereby individuals with higher psychological distress or pain catastrophizing were more likely to make a CTP claim, while those with higher depressive mood scores were less likely to claim. The connection between injury severity and baseline psychological status involved strong early links between post-injury baseline pain severity ratings and each aspect of baseline psychological reaction including post-traumatic psychological distress scores, depressive mood scores and catastrophizing scores.
Prior studies have found that immediate post-injury psychological state influences longer term health outcomes (12, 27–31). Our prior work from the FISH cohort using the same dataset found that mental health comorbidity is common following RTI, and mental health symptoms have strong interrelationships with pain (12). Using trajectory modelling, trajectories of depressed mood (based on DASS21 subscale), post-traumatic stress and pain interference were found. The relationship between mental health and pain interference trajectories revealed a high risk of poor quality of life due to chronic pain for those with chronic mental health symptoms, but not vice versa. This highlights the importance of addressing comorbid mental health symptoms early, to reduce long-term risk of prolonged pain interference in these vulnerable groups. Kenardy and colleagues studied a sample of compensable RTI in adult traffic injury patients in Queensland Australia. They found co-morbidity of psychological disorder was common, with only 33% of not meeting psychiatric criteria for either PTSD, generalized anxiety disorder (GAD), or major depressive episode (MDE) during first 2 years after injury (28). They also found substantial variability in the diagnoses of mental health disorders, as well as unstable diagnostic patterns over the first 2 years after RTI. Kenardy found that patients with pre-injury psychiatric history, poorer pre-injury health and social support, acute psychological distress and pain catastrophizing, were greater at risk of developing chronic mental disorders in the long term (28). Pozzato et al. found pre-injury and baseline vulnerability were predictive of longer-term mental health outcomes using pre-injury vulnerability factors (29) and autonomic recovery patterns with parasympathetic activity and heart rate (30).
The current analysis shows poorer psychological state post-injury means people were more likely to become involved in insurance claim processes. Prior publication of the analyses from the FISH dataset also found participants with higher number of injuries and longer duration of hospitalization, a higher perceived risk of dying and pain catastrophizing were more likely to have lodged a claim (29). Multiple theories exist to explain the poorer recovery of the injured claimants compared with non-claimants, and it is not conclusively established that claiming compensation directly causes poorer recovery (29, 31). Pozzato et al. identified a possibly circular nature of the relationship between seeking compensation and functional and psychological outcomes, whereby psychological and functional issues both contribute to and can be outcomes of seeking compensation (31).
Data from the FISH cohort suggested that “seeking compensation is not necessarily harmful to psychological health”, but stress vulnerability and injury-related disability were major risk factors for psychological distress (31). Studies have also identified legal services factors, such as advocating claimants to remain inactive in order to maximize compensation, can also be detrimental to physical and psychological recovery (32). However, the CTP scheme design in NSW and Australia does not preclude early initiation of treatment if people submit a claim (24).
CTP insurance claim was used in the current study, while there is other evidence that has examined the claiming process and described what elements of this process may be harmful to health (33–36). Anxiety/depression associated with claimant characteristics including female sex, coping style, and lawyer engagement had been reported previously (33). A cohort study from 3 Australian states found claimants reported high levels of stress trying to understand what needed to be done for their claim, claim delays, the number of medical assessments, and the compensation they received (34). It is important that safe compensation environments be developed with a focus on minimizing disability.
It is widely believed that reducing mental health symptoms could impact the post-trauma mental health trajectory. Interventions to prevent chronic mental disorders should be provided in the early post-injury period. A stepped care model provides a potentially cost-effective solution to the management of trauma-related psychopathology (37). Stepped care refers to the staged approach of practice of offering the least intrusive intervention first, and then increasing the intensity of intervention as necessary to achieve a desired outcome (37). O’Donnell et al. proposed a 3-stage model, consisting of early screening to identify those who are vulnerable for poor adjustment, monitoring those at risk, then offering early intervention to those who remain symptomatic after a period of time (38).
Currently, these screening and stepped care approaches are more likely to be located in the healthcare system, but they could also be embedded within injury compensation processes, depending on the compensation system. Based on the current study findings, it is necessary to have the screening and early intervention begin as early as possible post-injury, with the understanding that compensation and litigation decisions may be influenced by baseline and early post-injury experience. Once people enter a compensation scheme, there are additional factors that come into play that may influence longer term outcomes, so the compensation processes also need to be considered as part of the stepped care approach.
In the NSW and Australian context, the process of screening and stepped care could be initiated early in the claim lodgement process. Insurers and claims managers could institute a triage tool for detection of the level of risk of poor recovery and reviewed in a regular time-period. Once the risk is beyond a certain threshold, early intervention should be instituted. An example of this intervention can be the stepped collaborative care approach by Zatzick et al. (39). Their care approach utilized case management, motivational interviewing, pharmacotherapy, and cognitive behavioural therapy (CBT) (39). The involvement of a multidisciplinary team can potentially address other important mediators found in the current study, including pain interference and other environmental aspects not covered in the current path model.
The goal of this study was to highlight how and where baseline factors are operating to affect long-term outcomes. It confirmed that psychological/mental health factors had similar importance across levels of injury severity. The strength of this study lies in the use of innovative path modelling, which illustrated how baseline psychological factors are involved via multiple pathways in longer-term negative outcomes of injury severity. Individuals with higher psychological distress or pain catastrophizing were more likely to make a CTP claim, which was associated with poorer 12-month SF-12 results. This has clinical implications on the importance of early assessments for these factors early after injury (particularly a negative mental health history) and how to moderate them.
Even though this was a well-conducted large prospective cohort study with rigorous statistical analyses, there are several limitations. The follow-up rate was 60% at 12 months. However, statistical methods were used that take into account missing data due to loss to follow up, including the longitudinal mixed modelling and mediation analyses. Secondly, despite LOS being the most common indicator for injury severity used by transportation authorities worldwide (17), critics have argued that LOS will depend on comorbidity factors and also be affected by changes in healthcare delivery over time (40). However, from our previous analyses using the same dataset, it was found that the LOS and Injury Severity Score were strongly related, supporting the use of LOS in this study (16). The DASS21, IESR and Pain Catastrophizing Scale were chosen for this study because of the excellent criterion validity for detecting these psychological disorders in injured participants (23); nonetheless they are not intended for the purposes of diagnosis of psychological disorder and not comparable to clinical diagnosis by mental health professionals. For pre-injury measures obtained at baseline, there are potential recall biases even with the use of standardized instruments. However the 3-level version of the EQ-5D has very stark category distinctions (no problem at all, some problem, or an extreme problem), which would be less susceptible to this problem than a finer categorization. Lastly, other covariables could be relevant, which could not be considered in the current analyses; therefore we cannot infer causation from our findings.
CONCLUSION
Injury severity was associated with poorer 12-month physical and mental health outcomes through different mechanisms. Pain, psychological distress and motor vehicle crash insurance claims were all important mediators for negative health outcomes. Improved understanding of how early screening and interventions for pain and psychological distress may improve recovery trajectory and inform future models of clinical practice.
ACKNOWLEDGEMENTS
The authors would like to thank participants for partaking in the study, and NSW State Insurance Regulatory Authority for making this study possible.
Ethics approval and consent to participate
Ethics approval was obtained from the Central Sydney (Concord Hospital) Local Health District Human Research Ethics Committee.
Consent for publication
The manuscript did not contain individuals’ person-detailed data in any form.
Availability of data and materials
After conclusion of the FISH study, data may be available from the corresponding author on specific request.
Authors’ contributions
KH, AK and IC drafted the manuscript and contributed to the conception of the study. KB, JJ, AC, BG, SD, AC, MD and BG contributed to the conception of the study. JJ and IC contributed to the coordination of the study. IC designed the study, drafted the grant proposal, and is the principal investigator of the study. All authors critically revised the manuscript and agreed to the final version of the manuscript.
REFERENCES
- James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, et al. Morbidity and mortality from road injuries: results from the Global Burden of Disease Study 2017. Injury Prevention 2020; 26: i46–56.
- World Health Organization. Global status report on road safety 2018. [Accessed 25 March 2022]. Available from: https://www.who.int/publications/i/item/9789241565684
- MacKenzie EJ, Bosse MJ, Kellam JF, Pollak AN, Webb LX, Swiontkowski MF, et al. Early predictors of long-term work disability after major limb trauma. J Trauma Acute Care Surg 2006; 61: 688–694.
- Gabbe BJ, Simpson PM, Harrison JE, Lyons RA, Ameratunga S, Ponsford J, et al. Return to work and functional outcomes after major trauma: who recovers, when, and how well? Ann Surg 2016; 263: 623–632.
- Rainer TH, Hung KK, Yeung JH, Cheung SK, Leung YK, Leung LY, et al. Trajectory of functional outcome and health status after moderate-to-major trauma in Hong Kong: a prospective 5 year cohort study. Injury 2019; 50: 1111–1117. Available from: https://doi.org/10.1016/j.injury.2019.02.017
- Hung KK, Rainer TH, Yeung JH, Cheung C, Leung Y, Leung LY, et al. Seven-year excess mortality, functional outcome and health status after trauma in Hong Kong. Eur J Trauma Emerg Surg 2021: 1–10. Available from: https://doi.org/10.1007/s00068-021-01714-z
- Wilson JT, Pettigrew LE, Teasdale GM. Emotional and cognitive consequences of head injury in relation to the Glasgow Outcome Scale. J Neurol Neurosurg Psychiatr 2000; 69: 204–209.
- Castillo RC, Wegener ST, Heins SE, Haythornthwaite JA, MacKenzie EJ, Bosse MJ, LEAP Study Group. Longitudinal relationships between anxiety, depression, and pain: results from a two-year cohort study of lower extremity trauma patients. PAIN® 2013; 154: 2860–2866.
- O’Donnell ML, Bryant RA, Creamer M, Carty J. Mental health following traumatic injury: toward a health system model of early psychological intervention. Clin Psychol Rev 2008; 28: 387–406.
- Craig A, Tran Y, Guest R, Gopinath B, Jagnoor J, Bryant RA, et al. Psychological impact of injuries sustained in motor vehicle crashes: systematic review and meta-analysis. BMJ Open 2016; 6: e011993.
- O’Donnell ML, Elliott P, Lau W, Creamer M. PTSD symptom trajectories: From early to chronic response. Behav Res Ther 2007; 45: 601–606.
- Pozzato I, Craig A, Gopinath B, Kifley A, Tran Y, Jagnoor J, et al. Outcomes after traffic injury: mental health comorbidity and relationship with pain interference. BMC Psychiatry 2020; 20: 1–3. https://doi.org/10.1186/s12888-020-02601-4
- Valentine SE, Gerber MW, Nobles CJ, Shtasel DL, Marques L. Longitudinal study of mental health and pain-related functioning following a motor vehicle collision. Health Psychol 2016; 35: 742.
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med 1999; 48: 977–988.
- Jagnoor J, Blyth F, Gabbe B, Derrett S, Boufous S, Dinh M, et al. Factors influencing social and health outcomes after motor vehicle crash injury: an inception cohort study protocol. BMC Public Health 2014; 14: 199.
- Hung KK, Kifley A, Brown K, Jagnoor J, Craig A, Gabbe B, et al. Impacts of injury severity on long-term outcomes following motor vehicle crashes. BMC Public Health 2021; 21: 1–3. Available from: https://doi.org/10.1186/s12889-021-10638-7 [Accessed 25 March 2022]
- International Transport Forum. Reporting on serious road traffic casualties: combining and using different data sources to improve understanding of non-fatal road traffic crashes. IRTAD, International Traffic Safety Data and Analysis Group; 2012.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J Clin Epidemiol 1998; 51: 1171–1178.
- Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 1994; 56: 217–226.
- Sullivan MJ. The pain catastrophizing scale: user manual. Montreal: McGill University. 2009: 1–36.
- Weiss DS. The Impact of Event Scale: Revised. In: Wilson JP, Tang CS (editors) Cross-Cultural Assessment of Psychological Trauma and PTSD 2007 (pp. 219–238). International and Cultural Psychology Series. Springer, Boston, MA. Available from: https://doi.org/10.1007/978-0-387-70990-1_10 [Accessed 25 March 2022]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess 1998; 10: 176.
- Guest R, Tran Y, Gopinath B, Cameron ID, Craig A. Prevalence and psychometric screening for the detection of major depressive disorder and post-traumatic stress disorder in adults injured in a motor vehicle crash who are engaged in compensation. BMC Psychol 2018; 6: 4. Available from: https://doi.org/10.1186/s40359-018-0216-5 [Accessed 25 March 2022]
- State Insurance Regulatory Authority. What is a green slip? Available from: https://www.sira.nsw.gov.au/insurance-coverage/CTP-insurance-Green-Slips/what-is-a-green-slip [Accessed 25th March 2022].
- Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005; 58: 595–602.
- Viney R, Norman R, King MT, Cronin P, Street DJ, Knox S, et al. Time trade-off derived EQ-5D weights for Australia. Val Health 2011; 14: 928–936.
- Samoborec S, Ruseckaite R, Ayton D, Evans S. Biopsychosocial factors associated with non-recovery after a minor transport-related injury: a systematic review. PLoS One 2018; 13: e0198352.
- Kenardy J, Edmed SL, Shourie S, Warren J, Crothers A, Brown EA, et al. Changing patterns in the prevalence of posttraumatic stress disorder, major depressive episode and generalized anxiety disorder over 24 months following a road traffic crash: Results from the UQ SuPPORT study. J Affect Dis 2018; 236: 172–179.
- Pozzato I, Tran Y, Gopinath B, Cameron ID, Craig A. The contribution of pre-injury vulnerability to risk of psychiatric morbidity in adults injured in a traumatic road traffic crash: comparisons with non-injury controls. J Psychiatr Res 2021; 140: 77–86.
- Pozzato I, Tran Y, Gopinath B, Thuraisingham RA, Cameron ID, Craig A. The role of stress reactivity and pre-injury psychosocial vulnerability to psychological and physical health immediately after traumatic injury. Psychoneuroendocrinology 2021; 127: 105190.
- Pozzato I, Kifley A, Craig A, Gopinath B, Tran Y, Jagnoor J, et al. Effects of seeking compensation on the psychological health and recovery of injured patients: the role of stress vulnerability and injury-related disability. Psychol Med 2020: 1–12.
- Grant G, Studdert DM. Poisoned chalice? A critical analysis of the evidence linking personal injury compensation processes with adverse health outcomes. Melb Univ Law Rev 2009; 33: 865–885.
- Elbers NA, Akkermans AJ, Lockwood K, Craig A, Cameron ID. Factors that challenge health for people involved in the compensation process following a motor vehicle crash: a longitudinal study. BMC Public Health 2015; 15: 339.
- Grant GM, O’Donnell ML, Spittal MJ, Creamer M, Studdert DM. Relationship between stressfulness of claiming for injury compensation and long-term recovery: a prospective cohort study. JAMA Psychiatry 2014; 71: 446–453.
- Gabbe BJ, Simpson PM, Cameron PA, Ekegren CL, Edwards ER, Page R, et al. Association between perception of fault for the crash and function, return to work and health status 1 year after road traffic injury: a registry-based cohort study. BMJ Open 2015; 5: e009907.
- Murgatroyd DF, Casey PP, Cameron ID, Harris IA. The effect of financial compensation on health outcomes following musculoskeletal injury: systematic review. PLoS One 2015; 10: e0117597.
- Davison GC. Stepped care: doing more with less? J Consult Clin Psychol 2000; 68: 580–585.
- O’Donnell ML, Lau W, Tipping S, Holmes AC, Ellen S, Judson R, et al. Stepped early psychological intervention for posttraumatic stress disorder, other anxiety disorders, and depression following serious injury. J Traumatic Stress 2012; 25: 125–133.
- Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg 2013; 257: 390–399.
- Cryer C, Gulliver P, Langley JD, Davie G. Is length of stay in hospital a stable proxy for injury severity? Inj Prevent 2010; 16: 254–260.