ORIGINAL REPORT
UNILATERAL STRENGTH TRAINING AFTER TOTAL KNEE ARTHROPLASTY LEADS TO SIMILAR OR BETTER EFFECTS ON STRENGTH AND FLEXIBILITY THAN BILATERAL STRENGTH TRAINING – A RANDOMIZED CONTROLLED PILOT STUDY
Markus TILP, PhD1, Sebastian RINGLER, BSc1,2, Herwig MARIACHER, PhD2 and Dietmar RAFOLT, PhD3
From the 1Institute of Human Movement Science, Sport and Health, University of Graz, Graz, 2Maria Theresia Klinik, Bad Radkersburg, Austria and 3Center for Medical Physics and Biomedical Engineering, Medical University of Vienna, Vienna, Austria
Objective: Unilateral strength training has been shown to be more effective than bilateral training to increase strength in healthy people. The aims of this study were to test the feasibility of unilateral strength training during total knee arthroplasty (TKA) rehabilitation and compare it with standard bilateral training.
Methods: Twenty-four TKA patients from an inpatient rehabilitation programme were randomly assigned to unilateral and bilateral strength training groups. Both groups completed 6 strength training sessions during 3 weeks of rehabilitation. Isometric strength, knee joint flexibility, knee circumference, chair rise and walking abilities, and perceived exertion and pain were assessed before and after the training period.
Results: Both training groups increased isometric strength of both legs (+17–25%) and flexibility of the affected leg (+7.6%). Improvements in isometric strength of the healthy leg (+23% vs +11%) and flexibility of the affected leg (+10.7% vs +4.5%) were greater in the unilateral training group. Chair rise and 2-min walk test results improved in both groups, to the same extent. Perceived exertion decreased only in the unilateral training group (–20%), while perceived pain did not change in either group.
Conclusion: This study showed the feasibility of unilateral strength training in TKA rehabilitation. Strength and flexibility improved similarly or better with unilateral strength training compared with standard bilateral strength training. Future studies should analyse the efficacy of prolonged unilateral strength training following TKA.
LAY ABSTRACT
The rehabilitation process following a total knee replacement surgery is aimed at regaining strength and flexibility of the knee joint and improving the movements of daily living, such as walking and standing up from a chair. However, to date, it is not known which kind of strength training is most effective in achieving this aim within a rehabilitation programme. During standard rehabilitation, both legs are trained. The current study tested whether training of the affected leg only is feasible, and compared it with standard strength training of both legs. Training the affected leg only resulted in greater improvements in flexibility and similar or greater improvements in strength. Both types of training resulted in improvements in walking and standing up from a chair. In conclusion, strength training of the affected leg only is a feasible alternative to standard strength training with both legs in total knee replacement rehabilitation.
Key words: knee replacement; inpatient rehabilitation; walk test; chair rise; bilateral deficit; feasibility.
Citation: J Rehabil Med 2023; 55: jrm00381. DOI: https://dx.doi.org/10.2340/jrm.v55.3987.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Feb 14, 2023; Published: Apr 19, 2023
Correspondence address: Markus Tilp, Institute of Human Movement Science, Sport and Health, University of Graz, Graz, Austria. E-mail: markus.tilp@uni-graz.at
Competing interests and funding: The authors have no conflicts of interest to declare.
Knee osteoarthritis due to the degeneration of cartilage is a burden for many older people. If the pain becomes unbearable and other therapies are not successful, total knee arthroplasty (TKA) is the last resort. In Organization for Economic Co-operation and Development (OECD) countries, the number of TKAs performed increased by 35% between 2009 and 2019, with a mean incidence of 174 knee replacement surgeries per 100,000 population (1) in 2019. According to recent estimations, the incidence of TKA in Germany is anticipated to increase to 379 per 100,000 inhabitants by 2040 (2). This high incidence of TKA, especially in highly-developed countries, explains the need for well-suited rehabilitation programmes. Typical challenges after TKA surgery are a loss of strength and flexibility in the affected knee joint. These deficits significantly affect activities of daily living, such as walking, squatting, or climbing stairs, even a year after surgery (3).
The loss of strength in the muscles surrounding the knee joint is thought to be due to a combination of both atrophy and neuromuscular activation deficits (4). Therefore, guidelines for postoperative TKA rehabilitation include strength training/resistance exercise as a main pillar to regain knee joint function (5–7). While the need for strengthening exercise following TKA is undoubted, guidelines for rehabilitation are still in development, and further evidence-based recommendations are necessary.
A limited knee range of motion (ROM) following TKA may have several causes, and is significantly correlated with age, body mass index (BMI), implant design, surgical technique, pain, and preoperative ROM (8). The rehabilitation strategy used to increase knee ROM typically consists of passive knee ROM exercise, joint mobilization, cryotherapy, and functional training, including gait and stair stepping (7). Regaining a high level of knee flexibility is related to the fulfilment of patients’ expectations, their functional ability, and improved perception of their knee (9). An additional path to increasing ROM might be strength training. A recent review (10) showed that strength training, when applied over the whole ROM, has similar effects on flexibility as stretching exercises, at least in a healthy population.
Due to its multiple positive effects, bilateral strength training of the lower limbs is typically included in rehabilitation protocols. Training intensities are calculated from the bilateral one-repetition maximum (5). However, based on the theory of the bilateral deficit (11), i.e. reduced bilateral force production compared with the summed unilateral force production from the same homologous muscles, this might underestimate the muscle capacity, and hence limit the training result. Furthermore, unilateral strength training has been reported to produce greater increases in muscle strength than bilateral strength training in young women (12). Considering that most TKAs are performed only on 1 knee, and considering the limited training period for patients in an inpatient rehabilitation setting, unilateral strength training seems to be a promising and efficient way to improve strength and flexibility.
The aim of this study was to analyse the feasibility and the effects of unilateral strength training compared with routine bilateral strength training of the lower limbs on muscle strength, flexibility, and function in patients several weeks after TKA.
METHODS
Study design
Participants in this open-label randomized controlled study with parallel trials took part in an inpatient rehabilitation programme following TKA. At the beginning of their 3-week stay in the rehabilitation centre, eligible patients were informed about the study and invited to participate. Patients who agreed to participation were asked to blindly pick an envelope with the assignment to either an intervention group (IG) or a control group (CG). Both groups underwent the same routine rehabilitation programme, consisting of flexibility training, proprioception training, water aerobics, treadmill training, ergo cycle training, and strength training. This led, depending on organizational conditions, to an overall training load of 8–12 training sessions/week. The only difference between the groups was the strength training, which was performed unilaterally on the affected leg in the intervention group or bilaterally in the control group. Before the first session and following the 6 strength training sessions, the participants underwent tests of knee flexibility, muscular function, and isometric strength. These tests took place a day after the last strength training session or on the same day, but at least 3–4 h after the last strength training session. Furthermore, the rate of perceived exertion and subjective pain were recorded after each strength training session. All tests were performed at the rehabilitation centre.
Participants
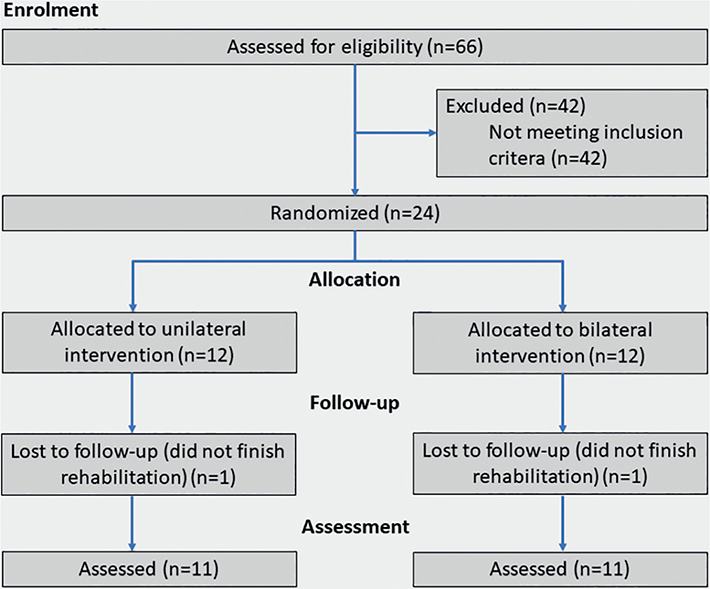
Patients were eligible to enter the study if they had undergone TKA surgery between 7 and 19 weeks previously. Exclusion criteria were a second TKA on the other leg or revision surgery of the affected knee. The sample size was calculated based on previous results from Botton et al. (12), who reported significantly greater changes in strength following unilateral compared with bilateral strength training, with a medium effect size (d = 0.61). Therefore, the minimum number of participants (mixed-factor repeated-measures analysis of variance (ANOVA) (factors: group (2) and time (2)), medium effect size (η²p = 0.1, f = 0.33), power = 0.8, alpha = 0.05, estimated correlation = 0.6) was calculated to be 9 participants/group, with G*Power (13). A total of 24 subjects agreed to participate in the study. Each participant provided written informed consent to participate in the study, which was approved by the University of Graz Ethics Commission (nr. 39/75/63 ex 2020/21). For reasons unrelated to the unilateral training, 2 participants (1 control group/1 intervention) did not finish the study, which led to 11 participants in each group (Fig. 1). Demographic and anthropometric data of the participants are shown in Table I.
Intervention
A sports scientist or a physiotherapist supervised each of the 6 strength training group sessions (4 participants/group) every other weekday. The strength training consisted of 4 exercises (leg press, calf raise, knee flexion, knee extension). Depending on the group assignment, the participants performed these exercises either unilaterally on only the affected leg or bilaterally. Each exercise was performed in 4 sets of 15 repetitions, with 1 min of rest between sets. The intensity of the exercises was controlled such that the patient could repeat the exercise 15 times in every set, so that the final 3 repetitions should be very exhausting. In case a participant would have been able to perform more than 15 repetitions in the first set, the weight was increased slightly for the following sets. Each strength training session was documented, including the patient’s subjective rate of perceived exertion and pain.
Outcomes
Isometric strength. The main outcome measure was isometric knee extension strength determined with an electronic force sensor (VPG Force Sensors, Model 1022, Tedea – Huntleigh, Netanya, Israel, 25 KHz) which was mounted to the wall. Each participant sat on a chair with their knee angle at 90° and was asked to push against the force sensor with maximum voluntary effort with the affected leg (isometric maximum voluntary contraction; IMVCTKA) and the healthy leg (IMVCH), respectively. No verbal encouragement or visual feedback was given. The maximum value of the isometric force curve (which was provided in kg) was recorded. After a rest break of 1 min, the test was repeated twice more, and the mean of the 2 best measurements was taken for further analysis. The intraclass correlation coefficients (2-way mixed) between the 2 best measurements from test day 1 were excellent with values of 0.99 (CI 0.976–0.996) and 0.98 (CI 0.944–0.990) for the affected and the healthy leg, respectively. This resulted in standard error of measurements of 0.63 and 0.83 kg for the affected and the healthy leg, respectively.
Flexibility and knee circumference. Flexibility was assessed using a handheld goniometer (Saehan 360-D2, Saehan Medical, South Korea) by an experienced physiotherapist. Handheld goniometers of this kind are reported to have an inter-rater reliability of 0.99 and a standard error of measurement of 0.84° (14). The knee circumference was measured using a flexible tape measure, 15 cm proximal to the superior patella edge, in a standing position, without any muscle activation.
Functional tests. To test the muscular function of the participants, a chair rise test (CRT) and a 2-min walking test (2MWT) were performed. During the CRT (15), the time for 5 consecutive stand-ups from a chair with arms crossed was measured with a stopwatch (15). During the 2MWT, which has been shown to be a valid and reliable test in TKA patients (16), the walking distance participants could cover in 2 min was measured on a 25-m track.
Rate of perceived exertion and pain. Participants provided information about their rate of perceived exertion, which was assessed using the 6–20 Borg scale (17), and the amount of pain on a 10-cm visual analogue scale (VAS) (18).
Statistical analysis
Data are presented as means and standard deviations, with 95% confidence interval, for changes from before to after the intervention. Data were tested for normal distribution using a Shapiro–Wilk test. To assess the effect of the intervention for normally distributed data, a 2-factor mixed ANOVA (between-factor: group; within-factor: time; interaction: group × time) was used. In the case of a significant interaction, post-hoc t-tests with corrections according to Holm (19) were used to determine possible differences in the changes between groups (IG vs CG). In the case of the data not being normally distributed (only for Borg, VAS) the effect of the intervention was assessed using Wilcoxon tests, to determine the changes within the groups. All statistical tests were performed using SPSS (version 27.0, SPSS Inc., Chicago, IL, USA), with alpha levels of 0.05. Effect sizes are given in terms of partial eta-squared measures (η²p). Effect sizes were interpreted as small ( > 0.01), medium ( > 0.06), and large ( > 0.14) (20).
RESULTS
Detailed values of the analysed parameters before (PRE) and after (POST) the rehabilitation period are summarized in Tables II and III.
| Variable | IG (unilateral) | CG (bilateral) | ||||
| PRE | POST | Δ (95% CI) | PRE | POST | Δ (95% CI) | |
| IMVCTKA (kg)a | 18.4 ± 6.6 | 22.7 ± 7.0 | 4.3 (2.5 to 6.3) | 16.7 ± 6.3 | 21.1 ± 5.9 | 4.3 (3.4 to 5.4) |
| IMVCH (kg)a,b | 21.1 ± 5.9 | 26.0 ± 5.8 | 4.9* (3.8 to 6.4) | 21.4 ± 4.3 | 23.9 ± 5.0 | 2.5 (1.2 to 4.1) |
| Flexibility (°)a,b | 101.8 ± 15.7 | 112.7 ± 17.1 | 10.9* (8.2 to 13.2) | 101.8 ± 12.1 | 106.4 ± 11.0 | 4.5 (1.9 to 7.5) |
| KC (cm) | 55.3 ± 7.9 | 55.6 ± 7.4 | 0.3 (−0.8 to 1.4) | 53.8 ± 4.2 | 53.5 ± 3.8 | −0.3 (−0.9 to 0.3) |
| CRT(s)a | 10.5 ± 2.5 | 8.1 ± 1.0 | −2.4 (−3.7 to −1.2) | 11.6 ± 1.5 | 8.8 ± 1.3 | −2.8 (−3.8 to −1.9) |
| 2MWT (m)a | 166.2 ± 36.8 | 193.6 ± 34.3 | 27.5 (20.2 to 34.4) | 142.9 ± 25.2 | 169.6 ± 23.2 | 26.7 (11.9 to 38.4) |
| aSignificant time effect, bsignificant interaction effect, *significantly different from control group (CG). IG: intervention group; Δ (95% CI): difference (95% CI); IMVCTKA/IMVCH: isometric knee extension force of the affected/healthy leg; KC: knee circumference of the affected knee, CRT: chair rise test, 2MWT: 2-min walk test. | ||||||
| Variable | IG (unilateral) | CG (bilateral) | ||
| PRE | POST | PRE | POST | |
| Borg | 12.0 ± 2.4 | 9.6 ± 1.4* | 12.1 ± 2.5 | 10.1 ± 2.7 |
| VAS | 3.2 ± 2.2 | 2.7 ± 1.6 | 3.6 ± 2.2 | 2.8 ± 1.9 |
| *Significantly different to PRE values. IG: intervention group; CG: control group; VAS: visual analogue scale. | ||||
The isometric force in the affected leg (IMVCTKA) increased in both groups, showing a significant time effect (F(1,20) = 60,898, p < 0.01, η²p = 0.753) but no interaction effect (F(1,20) = 0.003, p = 0.96, η²p < 0.01). The collapsed values for both groups increased significantly, from 17.54 to 21.86 kg (+25%, p < 0.01) (Fig. 2A).
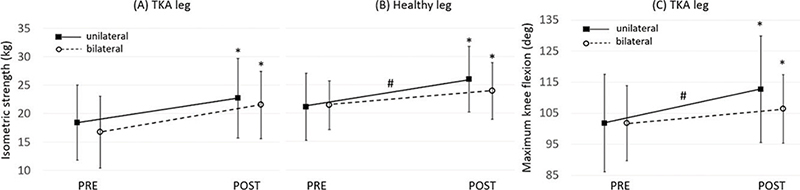
Fig. 2. Maximum isometric strength of the total knee arthroplasty (TKA) leg (A) and the healthy leg (B) and maximum knee flexion (C) before (PRE) and after (POST) unilateral and bilateral strength training. Mean and standard deviation (SD). *Significantly different from PRE, #significantly greater increase than after bilateral training.
The isometric force of the healthy leg IMVCH increased in both groups, showing a significant time effect (F(1,20) = 57.040, p < 0.01, η²p = 0.740, +17%), with a greater increase in the intervention group, as shown by the significant interaction effect (F(1,20) = 6,245, p = 0.02, η²p = 0.238) and a significant difference in the change from PRE to POST (IG: +4.94 kg; CG: +2.48 kg, p = 0.02) (Fig. 2B).
Knee flexion flexibility increased and showed a significant time effect (F(1,20) = 65.516, p < 0.01, η²p = 0.761) and a significant interaction effect (F(1,20) = 10.769, p < 0.01, η²p = 0.350). The increase in the intervention group was significantly greater than in the control group (IG: +10.9°; CG: +4.5°, p < 0.01) (Fig. 2C).
The ANOVA for knee circumference (KC) values did not show any significant time effect (F(1,20) = 0.001, p = 0.98, η²p < 0.01) or interaction effect (F(1,20) = 1.112, p = 0.30, η²p = 0.05).
CRT values decreased in both groups, showing a significant time effect (F(1,20) = 45.170, p < 0.01, η²p = 0.693) but no interaction effect (F(1,20) = 0.376, p = 0.55, η²p = 0.018). The collapsed values for both groups decreased from 11.1 to 8.5 s (p < 0.01).
The distance in the 2-min walk test (2MWK) increased in both groups, showing a significant time effect (F(1,20) = 47.274, p < 0.01, η²p = 0.703) but no interaction effect (F(1,20) = 0.009, p = 0.93, η²p < 0.01). The collapsed values for both groups increased from 154.5 to 181.6 m (p < 0.01).
A Wilcoxon test showed that the rate of perceived exertion (Borg) decreased significantly in the intervention group (p < 0.01), but not in the control group. Perceived pain following the strength training sessions did not change significantly (for detailed values, see Table III).
DISCUSSION
This study demonstrates that unilateral strength training is as feasible for participants as traditional bilateral strength training during TKA rehabilitation. Participants in both training groups increased the isometric strength of their knee extensors, with greater strength increases seen in the healthy leg in the unilateral training group. Both interventions increased the flexibility of the affected leg, with greater changes following unilateral training. Furthermore, both groups increased their functional performance in standing up from a chair and walking short distances, to the same extent. Perceived exertion decreased in the unilateral training group, but not in the bilateral training group. Only 1 participant terminated the programme in the unilateral group, for reasons not related to the strength training. Furthermore, the participants did not report any increase in subjective pain, as measured by VAS. Hence, unilateral strength training can be considered as safe and feasible in TKA rehabilitation.
Both training groups were able to increase the isometric strength of the affected leg significantly. However, in contrast to expectations, the strength gains were not greater in the unilateral training group. A previous study (12) on healthy individuals showed that unilateral strength training is more effective for strength gains than bilateral strength training. Besides the different participants (healthy vs TKA patients), another reason for the difference from the current study could be the short training period of only 3 weeks in this study, including only 6 strength training sessions, while the participants in the study by Botton et al. (12) trained for 12 weeks, including 24 training sessions. However, the inpatient programme following TKA in Austria is limited to 3 weeks, which might be too short to produce observable differences between the methods. Future studies should seek to increase the duration of unilateral strength training, e.g. by organizing an additional outpatient training opportunity and analysing the strength development over several months. Nevertheless, the overall strength gain of 25% within 3 weeks demonstrated that both training protocols can be used to successfully regain knee extension strength following TKA. It is notable that, at the end of the training programme, patients in both training groups reached isometric strength values for the affected leg that were similar to the values for the healthy leg at the beginning of the training programme. Since the training period was short, the observed strength gains were probably due to increases in muscle recruitment (21), but not in hypertrophy, as indicated by the unaffected knee circumference in both groups. However, the current study did not measure the electromyography (EMG) activity of the muscles during the tests. We therefore recommend including EMG measurements in similar future studies, to test this hypothesis.
The increase in isometric strength of the healthy leg (+23%) was greater in the unilateral group than in the bilateral group (+11%), despite this leg not being active during the strength training sessions of the unilateral group. While it was expected that the non-trained leg would also increase in strength, due to the contralateral effect on the corticomotor excitability on the untrained limb (22), the observed difference was surprising. Previous studies on unilateral training in healthy individuals have revealed smaller (23), similar (24), or even greater, changes (22) in the untrained limb. The differences between these previous studies are related to the different participants (healthy vs TKA patients), trained muscles (quadriceps vs wrist extensors), training duration and frequency (3 weeks vs up to several months), intensity, and contraction mode (concentric/eccentric/isometric) during the training and testing. A reason for the beneficial effect on the untrained limb in the current study could be that the healthy leg was also trained in the other training sessions of the rehabilitation programme (flexibility training, proprioception training, water aerobics, treadmill training, ergo cycle training), which included unilateral movements for both legs. Another possible reason could be that the healthy leg from the patients in the bilateral group was still fatigued from the training and could not reach maximum strength values during the testing. Hence, the strength of the healthy leg in the bilateral group would be underestimated. However, such an effect could not be observed on the affected leg in the unilateral group. Although it could also be expected that the unilateral training should be more tiring for the affected leg, the strength values at the end of the programme were not significantly different between the groups.
Besides the increase in strength, the rehabilitation programme also helped to increase knee joint flexibility in the affected leg in both groups, with significantly greater changes in the unilateral group (+10.9° = +10.7%) than the bilateral group (+4.5° = +4.5%). These values are greater or similar to targeted increases of ~6° from 1 to 3 months of physical and occupational therapy once a week following TKA surgery (25). Reviews (26, 27) of studies that analysed ROM changes following physiotherapy exercise intervention 3–6 months after TKA reported small to moderate advantages in knee flexion, compared with minimal intervention (+2.9°). However, the intervention protocols of the summarized studies were very heterogeneous, most often without supervised strength training, and therefore hardly comparable to the current study. The greater changes in the unilateral group could be explained by the unilateral strength training of the affected leg. Subjective feedback from the patients and trainers indicated that the specific focus on the affected leg during the unilateral strength training gave the patients greater confidence in the execution of the movement, possibly leading to greater ROM. This is in accordance with reports that strength training over the full ROM increases flexibility, in a similar way to stretching training (10).
In addition to improvements in strength and flexibility, participants were also able to increase their performance in functional movements, such as standing up from a chair (CRT) and walking short distances (2MWT). Both tests reflect daily tasks, which are especially important for elderly people to keep their independence, and to be able to participate actively in society (28). Both training programmes were able to induce positive changes to a similar extent. CRT improved by 23%, while 2MWT increased by 18%. These results underline the recommendation by Meier et al. (5), who recommended quadriceps strength to improve functional outcomes following TKA.
Implications for practice
These results show that unilateral strength training is feasible and effective in an inpatient rehabilitation programme following TKA. Unilateral strength training can be especially recommended for patients with limited flexibility.
Strengths and limitations
To the best of our knowledge, this is the first randomized controlled study to compare unilateral and bilateral strength training in rehabilitation following TKA. In addition to subjective feedback, this study also included objective strength measurements made with a force transducer to assess the training effects. A further strength of this study is the direct application in a real-world rehabilitation setting. However, the sample size of 11 participants per group is small, which impeded a more detailed analysis regarding sex, age, type of surgery, or time following surgery. It is possible that the results could have been affected by sex or BMI. However, post-hoc tests revealed no significant differences between distribution of sex (p = 0.39) or BMI means (p = 0.32) between the groups. Furthermore, changes in the different parameters were not significantly different between the sexes (p > 0.05) and correlations with BMI were very low (R = 0.01 (CRT) to 0.28 (VAS)). Therefore, we are confident that the results were not significantly affected by sex or BMI. Furthermore, the rehabilitation duration was limited to 3 weeks, due to national health system provision, and the results might differ for shorter or longer rehabilitation periods in other countries. It was not possible to take follow-up measurements to assess the long-term effect of the unilateral strength training. These limitations should be taken into account in future studies.
CONCLUSION
Three weeks of unilateral strength training as part of a TKA rehabilitation programme is feasible for patients and leads to similar (for the affected leg) or better (for the healthy leg) isometric strength and better improvements in knee joint flexibility than traditional bilateral strength training. Furthermore, both strength training programmes improve functional performance in standing up from a chair and walking short distances.
ACKNOWLEDGEMENTS
The authors would like to thank the patients for their active participation in the rehabilitation training and the supporting sport scientists and physiotherapists in the rehabilitation centre. Furthermore, the authors thank Dr Norbert Schrapf for technical support. The authors acknowledge the financial support by the University of Graz.
REFERENCES
- OECD. Health at a Glance 2021: OECD indicators. Paris: OECD Publishing; 2021.
- Rupp M, Lau E, Kurtz SM, Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res 2020; 478: 1622–1633.
- Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther 1998; 78: 248–258.
- Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty: the contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Jt Surg - Ser A 2005; 87: 1047–1053.
- Meier W, Mizner R, Marcus R, Dibble L, Peters C, Lastayo PC. Total knee arthroplasty: Muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther 2008; 38: 246–256.
- Pozzi F, Snyder-Mackler L, Zeni J. Physical exercise after knee arthroplasty: a systematic review of controlled trials. Eur J Phys Rehabil Med 2013; 49: 877–892.
- Jette DU, Hunter SJ, Burkett L, Langham B, Logerstedt DS, Piuzzi NS, et al. Physical therapist management of total knee arthroplasty. Phys Ther 2020; 100: 1603–1631.
- Oka T, Wada O, Asai T, Maruno H, Mizuno K. Importance of knee flexion range of motion during the acute phase after total knee arthroplasty. Phys Ther Res 2020; 23: 143–148.
- Devers BN, Conditt MA, Jamieson ML, Driscoll MD, Noble PC, Parsley BS. Does greater knee flexion increase patient function and satisfaction after total knee arthroplasty? J Arthroplasty 2011; 26: 178–186.
- Afonso J, Ramirez-Campillo R, Moscão J, Rocha T, Zacca R, Martins A, et al. Strength training versus stretching for improving range of motion: a systematic review and meta-analysis. Healthcare 2021; 9: 427.
- Steger J, Denoth J. Das bilaterale Defizit: Analysen anhand von Kraft-, EMG- und EEG-Messungen. Schweizerische Zeitschrift für Sport und Sport 1996; 44: 155–159.
- Botton CE, Radaelli R, Wilhelm EN, Rech A, Brown LE, Pinto RS. Neuromuscular adaptations to unilateral vs. bilateral strength training in women. J Strength Cond Res 2016; 30: 1924–1932.
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 2009; 41: 1149–1160.
- Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. J Exp Orthop 2018; 5.
- Runge M, Rittweger J, Russo CR, Schiessl H, Felsenberg D. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin Physiol Funct Imaging 2004; 24: 335–340.
- Yuksel E, Kalkan S, Cekmece S, Unver B, Karatosun V. Assessing minimal detectable changes and test-retest reliability of the timed up and go test and the 2-minute walk test in patients with total knee arthroplasty. J Arthroplasty 2017; 32: 426–430.
- Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–381.
- Downie WW, Leatham PA, Rhind VM, Wright V, Brancot JA, Andersont JA. Studies with pain rating scales. Ann Rheum Dis 1978; 37: 378–381.
- Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat 1979; 6: 65–70.
- Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic; 1988.
- Moritani T. Neuromuscular adaptations during the acquisition of muscle strength, power and motor tasks. J Biomech 1993; 26: 95–107.
- Goodwill AM, Pearce AJ, Kidgell DJ. Corticomotor plasticity following unilateral strength training. Muscle Nerve 2012; 46: 384–393.
- Lee M, Gandevia SC, Carroll TJ. Unilateral strength training increases voluntary activation of the opposite untrained limb. Clin Neurophysiol 2009; 120: 802–808.
- Hortobágyi T, Lambert NJ, Hill JP. Greater cross education following training with muscle lengthening than shortening. Med Sci Sports Exerc 1997; 29: 107–112.
- Mutsuzaki H, Takeuchi R, Mataki Y, Wadano Y. Target range of motion for rehabilitation after total knee arthroplasty. J Rural Med 2017; 12: 33–37.
- Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomised controlled trials. Br Med J 2007; 335: 812–815.
- Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord 2015; 16: 1–21.
- Gray M, Butler K. Preventing weakness and stiffness – a top priority for health and social care. Best Pract Res Clin Rheumatol 2017; 31: 255–259.