ORIGINAL REPORT
EVALUATION OF A STRUCTURALIZED SICK-LEAVE PROGRAMME COMPARED WITH USUAL CARE SICK-LEAVE MANAGEMENT FOR PATIENTS AFTER AN ACUTE MYOCARDIAL INFARCTION
Lars Tjessem, MD and Stefan Agewall, MD, PhD
From the Oslo University Hospital Ullevål, Oslo and Institute of Clinical Sciences, University of Oslo, Oslo, Norway
Objective: To compare a structuralized sick-leave programme with usual care sick-leave management in patients after an acute myocardial infarction. We hypothesize that a structured sick-leave programme will yield a faster return to work without negatively affecting quality of life.
Methods: Patients admitted to Oslo University Hospital due to an acute myocardial infarction were included in the study. Patients were randomized into an intervention group or a conventional care group. Patients randomized to the intervention group were provided with a standard programme with full-time sick leave for 2 weeks after discharge and then encouraged to return to work. The sick leave of the conventional group was mainly managed by their general practitioner.
Results: A total of 143 patients were included in the study. The conventional care group had a mean of 20.4 days absent from work, while that of the intervention group was significantly lower, with a mean of 17.2 days (p < 0.001) absent. There was no significant change in quality of life between the groups.
Conclusion: These findings strengthen the case for structuralized follow-up of patients with acute myocardial infarction, as this will have positive economic consequences for the patient and society as a whole, without making quality of life worse. Further investigation, with a larger study population, is warranted to determine the extent of health benefits conferred by early return to work.
LAY ABSTRACT
This study aimed to compare a structuralized sick-leave programme with usual care sick-leave management in patients after an acute myocardial infarction. The study included 143 patients who were admitted to Oslo University Hospital due to an acute myocardial infarction. Patients were randomized to an intervention group or a conventional care group. The intervention group followed a standard programme with full-time sick leave for 2 weeks after discharge, and were then encouraged to return to work. Intervention group patients had access to a telephone number to contact a cardiologist for advice if needed. The sick leave of the conventional group was mainly managed by their general practitioner. The sick leave of the intervention group was, 3.2 days shorter, whereas there was no difference in quality of life between the groups. In conclusion, these results indicate potentially large positive economic consequences of a structuralized sick-leave programme for patients and for society as a whole, with no worsening in quality of life.
Key words: myocardial infarction; quality of life; sick leave.
Citation: J Rehabil Med 2023; 55: jrm4569. DOI: https://doi.org/10.2340/jrm.v55.4569
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Apr 21, 2023; Published: Jul 24, 2023
Correspondence address: Stefan Agewall, Oslo University Hospital Ullevål, Oslo, Norway, and Institute of Clinical Sciences, University of Borgenveien 2A, NO-0370 Oslo, Norway. E-mail: Stefan.agewall@medisin.uio.no
Competing interests and funding: The authors have no conflicts of interest to declare.
The prevalence of cardiovascular disease is high (1). It poses a high economic burden in many countries (2). Treatment of acute myocardial infarction has changed radically during recent decades. Patients are usually re-vascularized and mobilized during the first few days after the event, and numerous research projects have been performed with the aim of improving the outcome of acute coronary syndrome (3–5).
Traditionally, much less effort has been put into optimizing the follow-up procedure after an acute life-threatening event, such as myocardial infarction, than has been applied to treatment (6). However, recent studies have shown that structured follow-up can be beneficial for patients’ quality of life after myocardial infarction (7–9).
Short- and long-term absence from work after an acute myocardial infarction is associated with substantial costs for society (2, 10). A long absence may also make it more difficult for the patient to return to work (11–14). In many countries there are no clear guidelines about the optimal duration and degree of sick leave with this condition, and scientific data guiding doctors are extremely sparse. Furthermore, sick-listing practices for cardiac patients vary considerably among countries (15). The Norwegian Directorate of Health recommends between 2 and 4 weeks’ sick leave after myocardial infarction (16). This observed different practice may be due to various factors, e.g. different health insurance systems, labour market conditions, culture and sick-listing traditions among physicians.
The aim of this study is to compare a structuralized sick-leave programme with usual care sick-leave management for patients after acute myocardial infarction.
METHODS
Participants and randomization
A total of 143 patients who were admitted to Oslo University Hospital due to an acute myocardial infarction were included in the study. All patients were assessed against the inclusion/exclusion criteria (Table I). Included patients were randomized into either an intervention group or a conventional care group by simple randomization (17); random allocation was performed by drawing a numbered ticket, corresponding to one of the 2 study groups. The number of tickets that were prepared for the study was set after calculating sample size, and ensured balanced randomization between the study groups.
Sample size calculations showed that approximately 50 patients per study groups would allow 80% power for detecting a clinically significant difference in each of the Medical Outcomes Study Short Form-36 (SF-36) health domains with p = 0.05. A total of 100 patients would also offer greater than 80% power to detect a clinically worthwhile 0.1 ± 0.2 standard deviation (SD) difference in utility scores on the Utility-Based Quality of Life – Heart (UBQ-H) questionnaire. In order to allow for patients lost to follow-up it was decided to include approximately 120 patients in the study.
ClinicalTrials.gov Identifier. NCT01108653.
Study groups
All patients were transferred back to their local hospitals after revascularization therapy at Oslo University Hospital.
The intervention group followed a structuralized programme with full-time sick-leave for 2 weeks after discharge. They were also given a telephone number to contact a cardiologist and a nurse at the department of cardiology, for support and questions during office time. After the initial 2-week sick leave, the patients were encouraged to return to work full time or part time according to individual requirements. The patients’ general practitioners were also instructed to help the patients to return to work as soon as possible.
The conventional group was sick-listed according to the discharging doctor’s assessment, and received no special follow-up or advice on when to return to work.
Outcome measures
Sick-leave duration. The length of every patient’s absence from work was recorded at the 12-month control. The duration of sick leave was calculated from the day of discharge from the hospital to the first day the subject returned to paid work.
Quality of life. Quality of life measures were performed at baseline and at 12 months, using the Utility-Based Quality of Life – Heart (UBQ-H), and the SF-36 and questionnaires.
The SF-36 from the RAND Corporation is a well-established survey of patient health, both physical and mental, and is validated for the use in monitoring and assessing care outcomes in adult patients. The SF-36 guides suggest that a difference of 10 points between groups per domain indicates a clinically significant difference (18, 19).
The UBQ-H was developed specifically for use in coronary artery disease. Components of UBQ-H include physical, psychological and social measures. It also includes 3 summary measures of quality of life; a time trade-off item, a rating scale and an ordinal health assessment item (20).
Statistical analysis
In this study a total of 143 patients were included to cover for patients lost to follow-up. Statistical analysis was performed using the SPSS Statistics 26 software. Data were tested for normality using the Kolmogorov–Smirnov test. Unpaired t-tests, χ2 tests and Mann–Whitney U tests for non-normal data were used for comparisons between groups. Statistical significance was inferred when p < 0.05. All results are presented unadjusted for multiple comparisons.
RESULTS
Study population and characteristics
A total of 143 patients were included in the study. However, 17 were lost to follow-up, of whom 13 did not attend for scheduled control and 4 were excluded for concurrent medical reasons.
All baseline characteristics were well balanced between the study groups (Table II). Of the 143 patients who entered the study, 98 (68.5%) had an index diagnosis of non-ST-elevation myocardial infarction (NSTEMI), while 45 (31.5%), had an index diagnosis of ST-elevation myocardial infarction (STEMI). Furthermore, 140 (97,9%) patients underwent percutaneous coronary intervention (PCI) as primary treatment, and 41 (28.7%) patients had a previous history of acute myocardial infarction or PCI.
| Characteristics | Conventional (n = 71) | Intervention (n = 72) |
| Physical characteristics | ||
| Sex (M:F), n | 38:33 | 37:35 |
| Age, years | 54.0 | 54.1 |
| Clinical details on index admission, n | ||
| Index diagnosis (NSTEMI:STEMI) | 48:23 | 50:22 |
| Prior acute myocardial infarction or PCI | 19 | 21 |
| Coronary risk factors*, n (%) | ||
| Family history for coronary artery disease | 18 (25.2) | 23 (31.9) |
| Hypercholesterolaemia | 32 (44.8) | 34 (46.9) |
| Hypertension | 30 (42) | 32 (44.6) |
| Current smoker | 15 (21) | 14 (19.3) |
| Diabetes mellitus | 12 (17.8) | 11 (15.1) |
| Obesity | 21 (29.4) | 24 (33.1) |
| Medication at discharge from primary hospitalization, n (%) | ||
| Aspirin | 71 (100) | 72 (100) |
| Antiarrhythmic agent | 8 (11.2) | 10 (11) |
| β-blocker | 69 (96.6) | 71 (97.9) |
| ACE-I | 27 (37.8) | 29 (40) |
| Diuretic | 11 (15.5) | 10 (13.8) |
| Insulin | 7 (9.8) | 4 (5.5) |
| Oral hypoglycaemic agent | 6 (8.5) | 6 (8.2) |
| Statin | 71 (100) | 72 (100) |
| M: male; F: female; AMI: acute myocardial infarction; PCI: percutaneous coronary intervention; ACE-I: angiotensin-converting-enzyme inhibitors. | ||
| *Family history of coronary artery disease: first degree relative aged < 60 years with an acute coronary event; hypercholesterolemia: total cholesterol level, 5,0 mmol/L; hypertension: blood pressure, 140/90 mmHg; diabetes: fasting plasma glucose level, 7.8 mmol/L; obesity: body mass index, > 30 kg·m-2). | ||
| All patient data were collected upon discharge from primary hospitalization. | ||
Absence from work
The whole study group was 18.8 (95% confidence interval (95% CI) 17.9–19.7) days absent from work.
The conventional care group had a mean of 20.4 (95% CI 18.9 – 21.8) days absent from work, while that of the intervention group was significantly lower, with a mean of 17.2 (95% CI 16.2-18.2) days absent (Fig. 1). The difference in absence between the 2 groups was statistically significant (2-sample t-test p-value < 0.001).
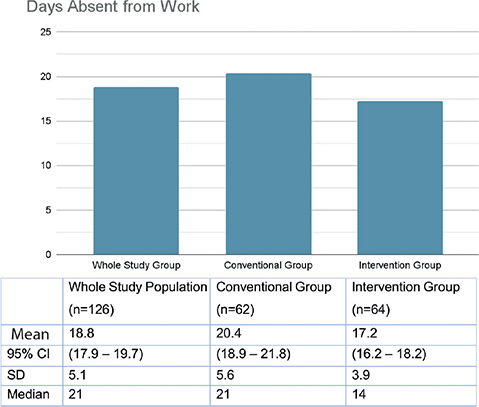
Fig. 1. Mean days absent from work after discharge. Comparing the 2 groups using unpaired t-test gives a p-value < 0.001. Days absent are calculated from the day of discharge from the hospital to the day of return to paid work. 95% CI: 95% confidence interval; SD: standard deviation.
Quality of life
Results at baseline (intervention vs control group) of quality of life using the UBQ-H questionnaire were not statistically different (0.9576 and 0.9587, respectively; p = 0.45 for difference between trial arms). Utility measures increased relative to baseline in both treatment arms over 12 months. At 12 months there was a non-significant improvement from baseline in both groups; 0.012 (95% CI 0.001–0.024) in the intervention group, and 0.010 (95% CI –0.001–0.022) in the control group. The difference between improvements in the study groups was not significant (p = 0.36).
At baseline the difference in SF-36 results between the 2 groups was not significant when assessing general health (p = 0.226). The conventional group scored 58.1 in the questionnaire, while the intervention group scored 59.5. After 12 months the results improved for both groups, although only marginally (p = 0.254) (Table III).
Readmissions and telephone use
During follow-up, 9 patients from the intervention group and 12 patients from the conventional group required readmission on a total of 36 occasions. The total number of readmissions was not significantly higher for the conventional group (20 vs 16; p = 0.50).
Also, 10 patients (16%) from the intervention group contacted the cardiologist or nurse by phone a total of 16 times. Of these calls 69% (n = 11) occurred within the first week after discharge from hospital.
DISCUSSION
This trial is one of the first to assess the effect of a structuralized sick-leave programme on patients after acute myocardial infarction. The results show that the structuralized sick-leave programme had an effect in decreasing the number of days absent from work, without affecting the quality of life negatively. Furthermore, there was no significant difference in the number of readmissions.
Patients in the intervention group had, on average, 3.2 days shorter absence from work than patients in the control group. This reduction in length of sick leave would have positive consequences from a health economic perspective, the details of which require further study.
These results show a significantly shorter absence from work compared with the studies of Català et al. (8) and Babić et al. (21). There may be several reasons for this. Firstly, Catelà et al. performed an observational, retrospective study, in which all patients aged 18–65 years hospitalized with ischaemic heart disease in Catalonia between 2008 and 2011 were included. There was no exclusion of patients on the basis of post-infarction heart failure (HF) or arrhythmia, or type of intervention. Secondly, the patient population also included patients with stable angina pectoris, a group that is often managed differently from patients with acute myocardial infarction.
Babić et al. reported a mean of 126 days absence from work in patients in Croatia with ST-elevation infarction (21). This study also differs from the current study, in that only patients with STEMI were assessed, and patients with post-infarction complications were included.
Furthermore, regional differences in sick-listing practices may also contribute to the difference in observed results. National guidelines in Norway suggest that 2–4 weeks of sick-leave is sufficient after uncomplicated acute myocardial infarction (16). This, in combination with the above-mentioned differences in study design, may have contributed to different results in the current study compared with those of Català et al. (8) and Babić et al. (21).
Both quality of life assessments in the current study indicate no negative change in quality of life measures for the intervention group. For the whole study population there is a non-significant, although positive, trend in quality of life measures when comparing baseline with 12 months. This is expected, as undergoing successful revascularization of stenotic coronary arteries can greatly alleviate the burden of symptoms.
Moreover, in the current study there was no significant difference in the number of readmissions between the 2 groups. In total 16.6% (n = 21) of the patients in the current study required readmission within the first year after discharge. This correlates well with other studies, and further supports the hypothesis that a structuralized sick-leave programme in this selected group of patients does not have a negative effect on physical or mental health (22, 23).
Interestingly, there was fairly low use of the telephone number issued to the patients in the intervention group. The majority of calls were made in the first week after discharge. This may indicate that some patients would benefit from a post-discharge call. However, it remains unclear which patients will benefit the most from this.
The major limitations of the current study include the small sample size and lack of continuity in inclusion and follow-up of the patients. Furthermore, the small sample size is likely to have limited the ability to detect significant changes that may exist in quality of life. It is also important to note that these findings apply to a select group of patients under the age of 65 years, without any form of post-myocardial infarction complications.
These findings strengthen the case for structuralized follow-up of patients with acute myocardial infarction, as this would have positive economic consequences for the patient and for society as a whole. Further research, with a larger study population, is warranted to determine the extent of health benefits conferred by early return to work.
ACKNOWLEDGEMENTS
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
The study was supported by Norwegian Helse South/east.
REFERENCES
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Executive summary: heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation 2014; 21: 399–410.
- Kotseva K, Gerlier L, Sidelnikov E, Kutikova L, Lamotte M, Amarenco P, et al. Patient and caregiver productivity loss and indirect costs associated with cardiovascular events in Europe. Eur J Prev Cardiol 2019; 26: 1150–1157.
- Kolloch R, Legler UF, Champion A, Cooper-Dehoff RM, Handberg E, Zhou Q, et al. Impact of resting heart rate on outcomes in hypertensive patients with coronary artery disease: findings from the INternational VErapamil-SR/trandolapril STudy (INVEST). Eur Heart J 2008; 29: 1327–1334.
- Girerd N, Magne J, Rabilloud M, Charbonneau E, Mohamadi S, Pibarot P, et al. The impact of complete revascularization on long-term survival is strongly dependent on age. Ann Thorac Surg 2012; 94: 1166–1172.
- Hall TS, von Lueder TG, Zannad F, Rossignol P, Duarte K, Chouihed T, et al. Relationship between left ventricular ejection fraction and mortality after myocardial infarction complicated by heart failure or left ventricular dysfunction. Int J Cardiol 2018; 272: 260–266.
- Edwards K, Jones N, Newton J, Foster C, Judge A, Jackson K. et al. The cost-effectiveness of exercise-based cardiac rehabilitation: a systematic review of the characteristics and methodological quality of published literature. Health Econ Rev 2017; 19: 37.
- Kavradim ST, Özer ZC. The effect of education and telephone follow-up intervention based on the Roy Adaptation Model after myocardial infarction: randomised controlled trial. Scand J Caring Sci 2020; 34: 247–260.
- Català Tella N, Serna Arnaiz C, Real Gatius J, Yuguero Torres O, Galván Santiago L. Assessment of the length of sick leave in patients with ischemic heart disease. BMC Cardiovasc Disord 2017; 17: 32.
- Briffa TG, Eckermann SD, Griffiths AD, Harris PJ, Heath MR, Freedman SB, et al. The cost-effectiveness of rehabilitation after an acute coronary event: a randomised controlled trial. Med J Aust 2005; 183: 450–455.
- Seghieri C, Berta P, Nuti S. Geographic variation in inpatient costs for acute myocardial infarction care: insights from Italy. Health Policy 2019; 123: 449–456.
- Lilliehorn S, Hamberg K, Kero A, Salander P. Meaning of work and the returning process after breast cancer: a longitudinal study of 56 women. Scand J Caring Sci 2013; 27: 267–274.
- Mewes JC, Steuten LMG, Groeneveld IF, de Boer AGEM, Frings-Dresen MHW, Ijzerman M, et al. Return-to-work intervention for cancer survivors: budget impact and allocation of costs and returns in the Netherlands and six major EU-countries. BMC Cancer 2015; 15: 899.
- Perk J, Alexanderson K. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 8. Sick leave due to coronary artery disease or stroke. Scand J Public Health Suppl 2004; 63: 181–206.
- Isaaz K, Coudrot M, Sarby MH, Cerisier A, Lamaud M, Robin C, et al. Return to work after acute ST-segment elevation myocardial infarction in the modern era of reperfusion by direct percutaneous coronary intervention. Arch Cardiovasc Dis 2010; 5: 310–316.
- Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med 2004; 46: 398–412.
- Norwegian Directorate of Health (2016). Acute coronary infarction (K75) Oslo: Helsedirektoratet (updated 18. May 2017, retrieved 25. February 2022). Available from: https://www.helsedirektoratet.no/veiledere/sykmelderveileder/diagnosespesifikke-anbefalinger-for-sykmelding/hjerte-karsystemet-k/akutt-hjerteinfarkt-k75
- Kim J, Shin W. How to do random allocation (randomization). Clin Orthop Surg 2014; 6: 103–109.
- Ware J, Sherbourne C. The MOS 36-Item Short-Form Health Survey (SF36). Med Care 1992; 30: 473–483.
- Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ 1993; 306: 1437–1440.
- Martin AJ, Glasziou PP, Simes RJ. A cardiovascular extension of the Health Measurement Questionnaire. J Epidemiol Community Health 1999; 53: 548–557.
- Babić Z, Pavlov M, Oštrić M, Milošević M, Misigoj Duraković M, Pintarić H. Re-initiating professional working activity after myocardial infarction in primary percutaneous coronary intervention networks era. Int J Occup Med Environ Health 2015; 28: 999–1010.
- Khot UN, Johnson MJ, Wiggins NB, Lowry AM, Rajeswaran J, Kapadia S, et al. Long-term time-varying risk of readmission after acute myocardial infarction. J Am Heart Assoc 2018; 7: e009650.
- Rymer JA, Chen AY, Thomas L, Fonarow GC, Peterson ED, Wang TY. Readmissions after acute myocardial infarction: how often do patients return to the discharging hospital? J Am Heart Assoc 2019; 8: e012059.