REVIEW ARTICLE
GOAL ATTAINMENT SCALING IN REHABILITATION: AN EDUCATIONAL REVIEW PROVIDING A COMPREHENSIVE DIDACTICAL TOOL BOX FOR IMPLEMENTING GOAL ATTAINMENT SCALING
Rachel BARD-PONDARRÉ, OT, MRES1, Claire VILLEPINTE, OT, PhD2,3, Fabienne ROUMENOFF, MD1, Hélène LEBRAULT, OT, MRES4,5, Céline BONNYAUD, PT, PhD6,7, Charles PRADEAU, MD8, Djamel BENSMAIL, MD9,10, Marie-Eve ISNER-HOROBETI, MD, PhD8,11 and Agata KRASNY-PACINI, MD, PhD8,1,2
From the 1French Red Cross, Lyon, France – French Red Cross, Lyon, France, 2University of Toulouse, Toulouse NeuroImaging Center, Toulouse, France, 3Toulouse University Hospital, School of Occupational Therapy, Toulouse, France, 4Saint-Maurice Hospitals, Department of Congenital Neurological Diseases, St-Maurice, France, 5Sorbonne University, Biomedical Imaging Laboratory, Paris, France, 6Raymond Poincaré Hospital, Motion Analysis Laboratory, Department of Functional Investigations, Garches, France, 7University of Paris-Saclay, Versailles, France, 8Physical Medicine and Rehabilitation Department, Clemenceau Institute and Strasbourg University Hospital, Strasbourg, France, 9Raymond Poincaré Hospital, Rehabilitation Department, Garches, France, 10End:icap Laboratory, Inserm, Versailles, France, 11Strasbourg University, Federation of Translational Medicine of Strasbourg, France 12Strasbourg University, Cognitive Neuropsychology and Pathophysiology of Schizophrenia, Inserm, Strasbourg, France
Context: Goal Attainment Scaling (GAS) is a person-centered and collaborative approach, allowing to assess the effectiveness of an intervention on personally relevant goals. However, GAS is not a “scale” but a heterogeneous group of methodologies, including many variations and lack of consensus on high quality GAS.
Objective: The aim of this communication is to: 1. provide updated didactical information on GAS use in PRM practice and research; 2. increase awareness of GAS methodological challenges; 3. guide use of GAS as an integrated process of rehabilitation after goal setting and; 4. provide updated resources for self-directed learning and extensive supplemental material to increase knowledge and practical skills in GAS use.
Methods: Educational literature review about current GAS applications relevant to PRM fields.
Results: Practical advice is provided regarding clinical challenges in GAS: definition of 0 level, time-frame and means employed to attain the goal, dealing with unforeseen pattern of improvement, synthesizing the numerous significations of “SMART” goal acronym to guide best use of GAS, and thinking flexibility on the type of relevant goals that can be set. Challenges with GAS in rehabilitation research are presented in order to promote researcher’s and reviewer’s awareness on reliable use of GAS and encouraging best-use of GAS.
LAY ABSTRACT
The goal attainment scaling methodology is a relevant way of measuring the effectiveness of a treatment, by creating scales to measure whether the goals previously identified with the person have been achieved through the treatment. There are many goal attainment scaling methodological variants, with a significant impact on results, of which users are not always aware. The aims of this review of the literature regarding current applications of goal attainment scaling in Physical and Rehabilitation Medicine fields, are to: (i) provide up-to-date didactic information on the use of goal attainment scaling in Physical and Rehabilitation Medicine practice and research; (ii) raise awareness of the methodological challenges of goal attainment scaling; (iii) guide the use of goal attainment scaling to support the rehabilitation process after goal setting; and (iv) provide up-to-date resources for self-directed training. Practical guidelines are provided for the use of goal attainment scaling in clinical practice, and the challenges of use of this methodology in rehabilitation research are presented in order to educate researchers and evaluators on the reliable use of goal attainment scaling.
Key words: goal attainment scaling; rehabilitation; person-centred; scales; clinimetric properties; quality appraisal; outcome.
Citation: J Rehabil Med 2023; 55: jrm6498. DOI: https://doi.org/10.2340/jrm.v55.6498.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Apr 5, 2023; Published: Jun 14, 2023
Correspondence address: Rachel Bard-Pondarré, Massues Center – French Red Cross, 92, rue Edmond Locard, FR-69322 Lyon Cedex 05, France. E-mail: bard.rachel@orange.fr; Rachel.BardPondarre@croix-rouge.fr
Competing interests and funding: The authors have conflicts of interest to declare.
Goal attainment scaling (GAS) (1) is a systematic method for the development of personalized evaluation scales. GAS provides an individualized measure of a person’s goal achievement that can be used as an outcome measure to quantify progress towards person-centred goals on an ordinal scale (2), typically ranging from –2 or –3 (3) to +2 (4) (see Fig. 1, which sets out 4 clinical situations with corresponding examples of use of GAS presented in a stair form, either with all 5 levels/steps or with only the 3 milestones described in detail. Also see Appendix S1 for examples of GAS in other fields of Physical and Rehabilitation Medicine (PRM)). GAS is a way of enhancing a person-centred approach in rehabilitation (5, 6). It provides a framework for focusing intervention on what matters most to the person (7). As such, the use of GAS is increasing rapidly, in both research and clinical PRM practice (Table SI). Practical guidelines on GAS (4, 8, 9) and a number of literature reviews (10–15) have been published previously, but little attention has been devoted to the diversity of use of GAS, with regard to GAS formulation, scoring, or themes.
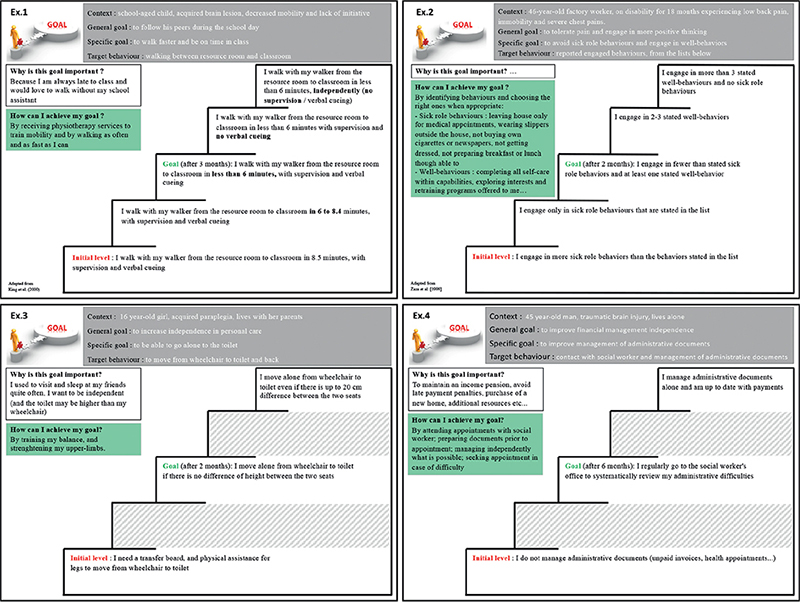
Fig. 1. Examples of goal attainment scaling (GAS). Because aiming at a “0” score can be depressing for patients, Bard et al. (64) developed a stair visual analogy to facilitate patient visualization of progress on the scale, as shown in these examples.
GAS formulation varies from precise scales, explicitly describing 5 levels of goal attainment, written by an independent team, controlling for difficulty, adequacy of GAS levels (17, 18), content validity (18), and taking precautions to minimize bias, such as controlling the measure’s context to avoid environmental influence; to formulation of the goal only, without specification of levels of goal attainment, by a single therapist (20, 21) or client/family (19, 21), with no review of validity and reliability of the scale and no exterior checking of goal adequacy.
GAS scoring also varies, from objective measures of goal attainment by an independent examiner (20), who is blinded to treatment (19), based on performance, and taking into account the ordinal nature of GAS data (22), to subjective ratings by a client’s therapist, or based on interviews with proxies (23) through phrases such as “worse than expected” and “much better than expected”, which are then transformed into T-scores, which wrongly give the reader the impression of a truly standardized, interval scale.
Finally, GAS themes vary from important goals regarding participation, activity and function, in domains that are important and meaningful for the client (24) and not measured by other standardized measures (26, 27), to goals relating to body functions (28, 29) (e.g. range of motion), without a clear measure of functional benefit in the GAS, and transforming numerical measures (e.g. visual analogue scale, range of motion) (29) into less arithmetically valid (2,30) GAS T-scores.
Consequently, GAS can be considered not as a scale but as a heterogeneous group of methodologies aiming at transforming goals into measures of goal attainment (see Fig. 2, which presents the different variants of GAS methodologies used reported in the literature, and Appendix S2 for examples of studies using these different GAS variants; these variants may concern the persons who set the goals, the types of goals set, the number of goals set, the level defined as initial level, the assessment methods, the scoring method, and the way of presenting results, as well as the person who finally scores the GAS). Due to variations in methodologies and lack of consensus on best practice in GAS, non-optimal GAS variants may be implemented by both clinicians and researchers (31). Researchers may not be aware of how inadequate use of GAS can influence the results of clinical trials that use GAS as an outcome measure (32), as clinimetric qualities are dependent on the way GAS scales are written (i.e. clinicians, researchers and reviewers cannot solely rely on GAS metrological properties presented in other studies and/or domains). In 2016, Krasny-Pacini et al. proposed criteria to appraise GAS quality in rehabilitation research. Following these criteria, a review by Harpster et al. (31) found that GAS quality in published trials is poor and, moreover, that methodological quality features of trials (i.e. randomization, blinding etc.) do not correlate with the quality of GAS methodology. This poor quality may be due to insufficient knowledge and practice in GAS by researchers and clinicians, which could be enhanced by providing a comprehensive literature-based didactical “tool box” for optimal implementation of GAS.
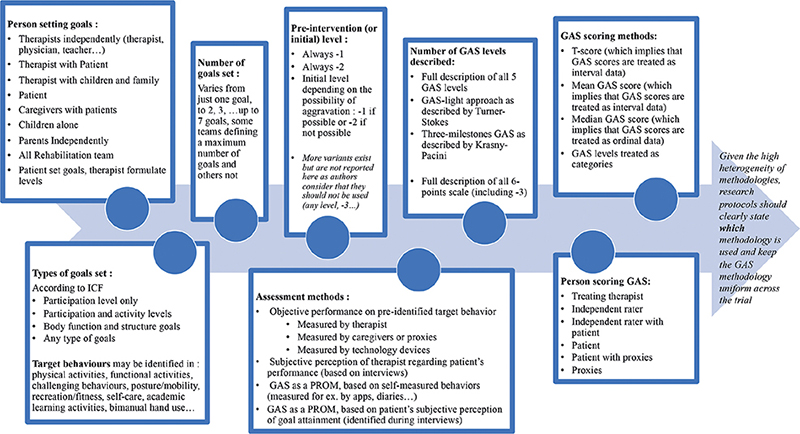
Fig. 2. The different variants of goal attainment scaling (GAS) methodologies reported to be used in literature; these variants may concern the persons who set the goals, the types of goals set, the number of goals set, the level defined as initial level, the assessment methods, the scoring method and how the results are presented, as well as the person who finally scores the GAS.
A PubMed search was performed using the single keyword: “goal attainment scaling”, from 2016 to July 2020. The search identified 143 publications, of which 29 were excluded as they were not related to PRM (e.g. no rehabilitation, dementia or autism domains). The remaining 114 papers were reviewed for additional useful information and/or novel approaches. Given the large number of papers retrieved in this search, no additional databases and addition keywords were used. Therefore, the paper cannot be considered a systematic and scoping review, but a narrative educational review. Papers relating to GAS methodology prior to 2016 have been analysed by the authors in a previous paper (32), and were also used here to include a broad and historical view of GAS. Each new use of GAS since 2016, reported in these 114 papers, was discussed by the group for its relevance and utility for this toolbox. A paper was cited if the group considered it could help clinicians or researchers gain a better understanding of the variation in the use of GAS, or the area of application of GAS. As this is not a systematic review, the papers cited are examples and not an exhaustive list of studies using GAS.
The aims of this educational review are to: (i) provide updated didactical information and tools on the use of GAS in PRM clinical practice and research; (ii) increase awareness of GAS methodological challenges; (iii) guide the use of GAS as an integrated process of rehabilitation after goal setting; and (iv) provide updated resources for self-directed training. This paper outlines the general methodology for creating goal attainment scales, and presents a broader perspective including goal identification and goal support. Other challenges related to GAS in rehabilitation research are discussed, and recommendations are set out.
GENERAL METHODOLOGY FOR CREATING GOAL ATTAINMENT SCALES
How to define GAS levels (i.e. how to transform a goal into a 5-point scale)
The general frameworks for GAS procedure in rehabilitation is shown in Table I, with different steps adapted from Ottenbacher & Cusick (33). Task analysis provides a tool for the identification of actions or sub-tasks required to achieve a task or particular goal, that are useful for the development of appropriate GAS levels (8). Consideration of both individual factors (i.e. biomechanical, sensory-motor, cognitive and/or psychosocial) (8) and environmental factors (i.e. physical, cultural, social, economic and political) contribute to context-specific GAS levels (8).
| Step | |
| Step 1 | Identify an overall (general) objective. |
| Step 2 | Identify specific problem areas that should be addressed. |
| Step 3 | Specifically identify what behaviours or events would indicate improvement in each of the areas selected in Step 2. |
| Step 4 | Determine the methodology that will be used to collect the desired information. |
| Step 5 | Select the expected level of performance (0 level). |
| Step 6 | Identify the most favourable outcome (+2), the least favourable outcome (–2) and intermediate levels (+1 and –1) of the client’s performance (GAS levels). |
| Step 7 | Verify whether there are overlapping levels, gaps between levels, or more than 1 indicator in a problem area and so on (see GAS checklist). |
| Step 8 | Verify the client’s current status and determine the timing of future evaluations to document progress. |
Perhaps the most essential logic to apply when formulating GAS levels is that only 1 aspect should be manipulated from 1 level to the other, considering: (i) the quantity (e.g. time, distance, number of behaviours) or; (ii) the context (e.g. cueing, walking aid, supervision), but not both at the same time. King et al. (34) provide an example reported in Fig. 1, example 1. Bovent’Eerdt’s (8) method provides the foundation for this logic, and Ruble (16) developed this notion, proposing a series of GAS content that can be modulated to obtain levels for domains that may be difficult to translate into goals (e.g. cognitive, psychological and social goals). These include: frequency of a skill, type of prompting (from direct, physical, to simple supervision, or independence), frequency of prompting, cueing needed to succeed (from specific and external cues to non-specific or self-generated cues), number/type of person with whom a behaviour is possible (from the therapist, family to co-workers and strangers), type of context (structured, unstructured, unusual), and type of material (manages with a specific type of technical device, to any type of aid).
SMART goals: SMART GAS
Numerous definitions of the SMART acronym are presented within the studies. The Specific, Measurable, Attainable, Relevant, Time-determined definition demonstrates most relevance to rehabilitation. “Relevant” is preferred to the often used “Realistic”, as the terms Attainable and Realistic refer to the same concept. While the acronym is widely used, and most clinicians both acknowledge and practice “SMART” goal setting, the meaning behind the 5 terms continues to be interpreted in different ways.
What is a “specific” goal? The term “specificity” has a range of relevant significations:
- General goals should be transformed into more specific goal attainment indicators. e.g. “one participant needed to demonstrate that he could manage his fortnightly income (general goal), so it was agreed that he would likely achieve this if he could establish and meet a fortnightly budget, plan ahead and set money aside for future expenditure, and regularly save money (specific goal).” (25);
- Goals should be specific to individual personal and unique needs; e.g. for an intervention focusing on improving executive functions in daily life (general goal), the specific goal would be for patient A: being able to prepare child’s school bag with nothing missing; for patient B: being able to cook a meal unsupervised; for patient C: return to work part-time;
- In research, GAS defined after inclusion should be specific to the aim of the intervention; e.g. a goal of budget planning is specific to the aim of an intervention focusing on improving executive functions in daily life, but improving social skills isn’t, even if it is more relevant to the patient at the time of the intervention. When GAS is used as an outcome measure in interventional studies, goals are intervention-determined, i.e. the patient and goal setter are required to choose a goal that is relevant and specific to the intervention being tested. This can be different to clinical practice, in which the intervention is goal-determined, i.e. patient’s goals are listed and intervention(s) chosen according to patient’s goals.
What defines a “measurable” goal? Differing views describe whether goals should rely on interview-based, subjective perception of goal attainment or a performance-based objective measure of goal attainment. While both offer insight into rehabilitation effects, the 2 approaches are fundamentally different. The former is a patient-reported outcome measure (PROM), involving patients in the measurement of rehabilitation effects. It offers the possibility of capturing non-measurable effects (i.e. intervention effects in daily life and ecological context), and is particularly easy to use in daily practice. The latter is an objective measure, in which the patient participates at the initial stage of setting goals, but GAS then becomes an objective (though personalized) scale. It measures patient’s true progress, based on a selected target behaviour thought to reflect patient’s progress towards his/her goal. On the one hand, this method allows us to objectively measure goal attainment, which may differ from patient’s perception of progress; on the other hand, it is time-consuming if its reliability and validity are to be sufficient. Both interview-based and performance-based GAS approaches coexist and have their advantages. In all cases, Kiresuk recommended to “anchor scale points with behavioural or other evidence that will be meaningful to the client and readily scored by the rater” (35). A dialectical approach between these 2 methods could be to use both ecological participant-rated GAS as a PROM (with the risk of being subjective and less measurable), and performance-based GAS (with the risk of being less ecological). We believe that, even if GAS is used as a subjective PROM, every effort should be conducted to make it measurable by the participant. For example, keeping a diary of the chosen target behaviour (e.g. number of anger outbursts) could be more reliable than just asking the patient if they attained the goal “I can manage my anger 75% of the time” (10).
Being “attainable” is a major challenge for goals for patients and therapists in rehabilitation. GAS literature emphasizes that all levels should be realistic; however, this proves challenging for patients who lack self-awareness. They may have difficulties in identification of realistic goals and of what needs to be done for attainment. While original GAS literature requires that all GAS levels should be realistic, a clinically used technique in patients lacking self-awareness and insight is to use the patient’s unrealistic goal as the +2 level and use a therapist-chosen realistic goal as the 0 level. This enables both therapists and patients to agree which goal to work on, even if an agreement cannot be obtained as to what to expect within the given time-frame. Another approach is to keep the patient’s unrealistic goal as a (very) long-term goal, but to involve the patients in setting more realistic subgoals.
The term “relevant” refers to a goal that is: (i) personalized to the patient and specific to his/her context (i.e. environmental and psychological); (ii) clinically relevant for function (or at least a subgoal towards function or comfort); and (iii) with clinically relevant change across each GAS level. Being relevant to the patient and being relevant clinically may diverge, as many clinically relevant goals are often used in rehabilitation even if the patient does not find them relevant (e.g. maintain trunk equilibrium in seated position before learning transfers after spine injury). Discussing the clinical relevance of the goal with patients often contributes to achievements of personal relevance. Conversely, the main goal of a patient may differ from a therapist’s view of relevant functioning. While it is a challenge in the early stages of rehabilitation, for rehabilitation concerning chronic disabilities, an effort should be made by therapists to orient rehabilitation on the person’s goals, even if therapists have other goals that they consider relevant for the patient.
“Time-determination” is essential, encompassing many components that should be considered: (i) time-frames post-intervention are determined for GAS scoring (e.g. assessment at 3 months after botulinum toxin injection, 2 weeks after cognitive rehabilitation completion, 3 months after effective wearing of orthosis, etc.); (ii) time-determination also allows breaking down long-term goals into short-term goals and helps patients to plan small goals or subgoals, eventually leading to life goal achievement (e.g. learning to use a smartphone alarm to attend appointments on time is a short-term goal, but constitutes a step towards a life goal of returning to previous employment after brain injury) and; (iii) maintenance of goal attainment over time is also a common objective of rehabilitation. Table II proposes a checklist for clinical use, for checking if goal attainment scales are “SMART” enough.
| GAS checklist |
|
| *Note: This checklist is intended for clinical use. When GAS is used as an outcome measure, more comprehensive and quantitative GAS quality scales should be used (refer to (32)). |
Definition of 0 level, time-frame and means employed to attain the goal
The 0 level is usually defined in terms of intuitive clinically-based impressions: (i) “Minimally acceptable outcome to both provider and client” (10); (ii) “What the clinician truly believes would be clinically meaningful and what the client will most likely achieve” (11) and; (iii) “Level the patient can achieve in the specific time with rehabilitation but not exceptional effort”(10). From a methodological and statistical point of view, the 0 level was intended to be chosen in a way to have a maximum of 0 scores after intervention and +2 and –2 scores to occur in 5–10% of similar participants (36). Traditionally, the aim was to yield a Gaussian normal curve of T-scores centred by a T-score of 50 and a standard deviation (SD) of 10.
Therefore, looking at the literature, setting the correct 0 level could be based on: (i) probability of achievement, with emphasis on the attainability/realism of the goal and; (ii) clinical acceptability and importance, emphasizing the relevance of the 0 level. The rationale behind attainability of goals is complex, as goal attainability depends on 3 implicit clinical reasoning factors needed to set realistic goals: time-frame, knowledge of possible gains, and means to achieve the goal. For example, a family goal of “walking without aid” for a hemiparetic child with cerebral palsy may be realistic in a 1-year time period, but unattainable if the time frame for evaluating GAS is 1 month (i.e. at the end of a short clinical trial for a novel intervention). Knowledge of pathology, possible gains and expertise of intervention by the professional setting the scale are crucial factors that impact GAS validity and realism of levels. Furthermore, goals are set, bearing in mind that improvement (or lack of improvement) is influenced by many factors, independent of intervention including: the natural course of the condition (e.g. cerebral palsy vs evolutive aetiologies of spasticity), associated deficits (e.g. seizures, pain), patient’s psychological factors, age, chronicity, etc.
Finally, it is often overlooked that goals are negotiated taking into account the therapeutic means that can be employed for the goal. For example, when setting the goal of independent ambulation, the clinician already projects which interventions are available, and the realistic 0 level will depend on access to orthopaedic surgery, intensive physiotherapy, repeated botulinum toxin injections, etc. Experienced clinicians usually integrate all these in clinical reasoning defining what constitutes a realistic and relevant goal to inform collaborative goal setting with the patient.
When used as an outcome measure in research, GAS should be set: (i) prior to randomization, (ii) by professionals demonstrating expertise in expected outcomes associated with treatment, (iii) in order to set adequate (and comparable across trial groups) 0 levels, it should be specified if 0 levels are defined considering what can be obtained in care-as-usual or what can be obtained due to the novel intervention being tested. (iv) Furthermore, it should be explicit to goal setters if the 0 level is to be attained at the first evaluation (e.g. after a 3-month intervention) or at follow-up (e.g. at 6 or 12 months). The majority of research protocols lack this information, with some exceptions (37–42). Most authors only state if “goals were assessed after intervention and at follow up” without specifying if the intended time frame of 0 level was at post-intervention or follow up (43, 44). In addition, protocols with multiple measurement time-points could provide a clear explanation of what is to be done if a goal is achieved at the first evaluation, i.e. set a new goal for the rest of the intervention or evaluate maintenance of the original goal. In research, goals need to be specific to the intervention being tested and of equal difficulty in control/experimental groups. Therefore, a synthetic definition of the 0 level could be “the clinically relevant progress this patient will most probably attain after x months of interventions y (y being the “reference” for goal setting in both groups).” GAS setters must compromise the patient’s ideal progress with the probability of that progress to set the 0 level.
For clinical practice, 0 level is often simply the patient’s “goal”, assuming all possible means will be employed to achieve it, within a given time-frame that may be extended without being a threat to GAS validity.
Dealing with unforeseen patterns of improvement
A major challenge and source of frustration in GAS may occur when patients make unquestionable clinical progress that is not captured by the scale. This may be because the patient’s performance does not “fit” within the levels that were set. For example, GAS levels may have predicted that the patient would walk a greater distance; however, progress was not on the walking distance but on walking ability on uneven ground. Alternatively, patients may change or reorient their goal. For example, GAS on walking to the bakery, whereas the patient now bakes their own bread; or GAS on adapted employment, whereas the patient has enrolled on a university degree. Two useful approaches can be used in such cases, as follows.
First, the 3-milestones GAS (45) (see last 2 examples in Fig. 1) provides a way of explaining GAS levels. This is an appropriate intermediate between time-consuming processes of describing all 5 levels (3) and the GAS light method (9) (see previous literature-based GAS update (4)). It explicitly describes the initial –2 level, the 0 level and the +2 level, whereas intermediate points –1 and +1 are not described, but are implicit (levels –2, 0 and +2 are milestones that indicate the transition to the next level). Originally proposed as a compromise between reliability and time needed to describe the levels, emerging data suggest that it is, in fact, more reliable than the usual way of describing all 5 levels (Personal communication. A rating system to evaluate the quality of goal attainment scales used as outcome measures in rehabilitation). Intermediate levels allow more variation or “room” for unexpected patterns of progress (e.g. if goal attainment did not reach the 0 level but there is some progress towards the goal, a –1 score can be attributed). They also allow scoring of progress irrespective of how the change occurred (e.g. without having to foresee exactly if the progress will relate to higher frequency of a behaviour, or better accuracy, or fading of necessary cues etc.).
Secondly, Zaza et al. (46), in the area of chronic pain (see example 2 in Fig. 1), offers an interesting possibility to define GAS steps using behaviours lists. Rather than agreeing on a single type of pain-related avoidance behaviour to be reduced, a list of problematic behaviours expected to decrease after intervention is set out, and GAS levels are expressed as the decreased number of sick role behaviours. This kind of approach is particularly useful when a set of goal behaviours is identified and when it is difficult to choose which is the most relevant sensitive to change. Rather than transforming each behaviour into separate goal attainment scales, goal attainment levels may use the number of target behaviours.
Goal types
GAS can relate to any goal, and different types of goal attainment scales can be set for 1 general goal for 1 patient (see Fig. 3, which presents a conceptual framework for the different types of goals, that could be (or not be) converted in a goal attainment scale, and examples of its application in Appendix S3). Using more than 1 scale for a general goal increases awareness of related processes. For example: (i) Skill acquisition, such as being able to drive a powered wheelchair in a rehabilitation centre and ecological application of the skill (i.e. actual use of the wheelchair alone in the community); (ii) Symptom reduction (e.g. decreased anxiety) and its impact on quality of life (choosing a meaningful goal could then be based on “what would you want to do if you were less anxious?”). GAS can also serve as a transfer/generalization measure (23), reflecting whether a particular behaviour, trained and observed in therapy sessions, is also observed in the person’s natural context (i.e. transferred) or even observed in untrained activities (i.e. generalized). In any case, GAS should be used with relevance to International Classification Functioning, Disability and Health (ICF) activity and participation levels (47), not body structures and functions (32).
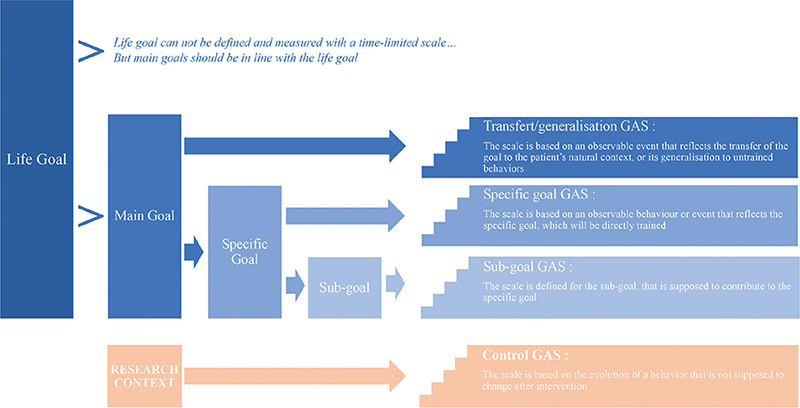
Fig. 3. Framework for goal types. A conceptual framework for the different types of goals, that could be converted (or not converted) in a goal attainment scale (GAS). A life goal cannot be defined and measured with a time-limited scale, but the main goals should be in line with the life goal. Main goals can sometimes be directly converted into scales, or may need to be specified before being defined into a scale, or may sometimes need to be divided into subgoals. Control GASs are specific to the research context.
A BROADER PERSPECTIVE ON GAS: GOAL IDENTIFICATION AND GOAL SUPPORT
GAS is mostly used for setting SMART goals and defining goal attainment scales. In the following section, we discuss useful steps prior to (i.e. goal identification) and after goal setting (i.e. goal support and coaching). Fig. 4 represents a chronological line, where the different steps are identified from goal emergence to goal attainment assessment. This underlines the necessary steps prior to and after goal setting, and the unavoidable collaboration between the person being cared for and the therapeutic team.
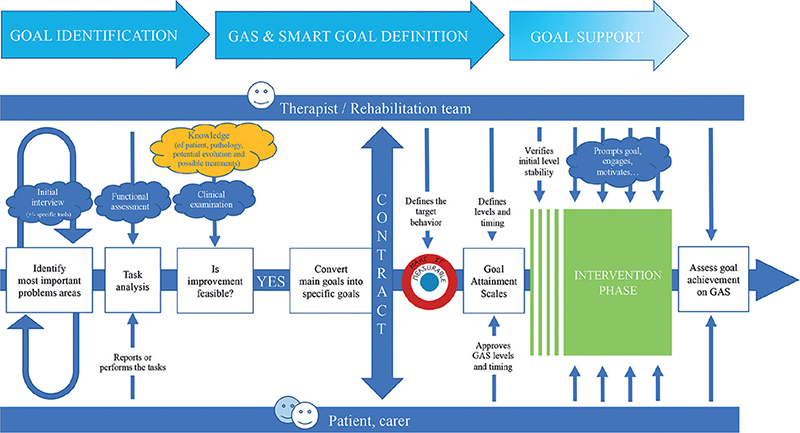
Fig. 4. From goal identification to goal support framework. A chronological line, on which the different steps are identified, from goal emergence to goal attainment assessment. This underlines the necessary steps prior to and after goal setting, and the unavoidable collaboration between the person being cared for and the therapeutic team.
Goal identification
Individuals may have difficulty defining goals or even specific problem areas. Turner-Stokes (48) noted that, when initially asked to state their goals for treatment, patients often expressed goals in terms of long-term aspirations and hope for a cure. During goal setting, long-term aspirations (e.g. patient independence) are broken down by the team into medium-term objectives for the treatment programme and a series of staged goals aimed at achieving those objectives, which can be converted into GAS (see Fig. 3). In chronic conditions on the other hand, when patients do not aim at recovery, they may not see what could be improved. Tools such as the Canadian Occupational Performance Measure (COPM) in combination with GAS help patients to establish goals (49), based on the functional problems they face in their daily lives, rather than problems of body function and structure. Other resources for goal identification prior to setting GAS scales are summarized in Table SII.
Whichever method is used, it should be person (and/or family)-centred and collaborative. This will ensure that the goals are important to patients, thus enhancing motivation involvement in the achievement of those goals.
Goal support
Steps for guiding goal support and coaching of patients are shown in Table III. In clinical practice, every effort should always be made to help clients, their therapists and their families to remember, practice and implement their goals in daily life. In research, however, the way in which goal support is, or is not, part of the intervention should be explained clearly in the study methods, as this will impact the results. (i) At one extreme, some interventions clearly test how goals can be supported. Goal support is, in fact, the heart of the intervention (7) and those goals are trained. (ii) At the other extreme, some protocols use GAS as a generalization measure, whereby goals are not trained and not supported, precisely to investigate whether clients spontaneously use the skills they are taught to achieve their goals (23). (iii) In between these extremes, any degree of goal support may or may not be part of the intervention: (a) an intervention may be goal-focused (i.e. training the client on their specific goal), but without any support for implementation of that goal in daily life; (b) an intervention may provide general skills or train separate functions analytically, but include goal support to increase the probability that these skills will be implemented in daily life. However, even in research, interventions are more likely to be effective in daily life if goal support is included in the intervention (and unless the protocol explicitly seeks to extract a specific intervention effect from the non-specific motivational and coaching effects). It may be relevant in research protocols to include goal support as a standard comparison, i.e. to provide goal support in the control group or the control condition/baseline (i.e. in single-case experimental designs).
| Steps in implementing GAS | |
| 1 | Remind the patient (and team) of the goals (NB: crucial step if the patient has a cognitive impairment): For example, at the beginning of every rehabilitation session (56), by text messages (65), reminding carers and family of the goal through additional phone coaching (56), by portable voice organizers (66), by apps (e.g. Goal Map). |
| 2 | Plan how to attain the goal and provide written support for its attainment; i.e. who, where, when, and how? What the rehabilitation team will do and most importantly what the patient will do, where (as much as possible in his/her natural settings) when (how frequently), and how (e.g. define amount of assistance): refer to examples (38, 67–72) |
| 3 | Help implement goals into the patient’s daily life For example:
|
| 4 | Give concrete support for reaching goals throughout intervention: Home/work/school-visits, logbooks, notebooks with advices, apps, photographs, or any support to visualize activity to work towards goal… (7) |
| 5 | Encourage, engage, increase goal commitment* and give feedback on goal attainment to the patient (42, 83). |
| *Goal commitment: this paper does not aim at reviewing methods for obtaining goal commitment, which is another crucial component of goal-based rehabilitation. Readers can refer to the abundant literature on this subject, especially literature on motivational interviewing (84–87), life goal concept (88), self-regulation theory (73, 89, 90) and the work of Siegert & Levack (91). Increasing literature emphasizes that: (i) motivating clients is as important as providing adequate therapy; (ii) emotions play a crucial role in rehabilitation; and (iii) looking for a dialectic between motivation to change and acceptance of reality is often the most effective skill to deal with adverse emotions associated with not attaining goals and to regulate those emotions (see literature on dialectical behaviour therapy (92)). | |
OTHER CHALLENGES WITH GAS IN REHABILITATION RESEARCH
Previous literature has detailed difficulties associated with GAS use as an outcome measure (15, 32, 51). Rigorous applications of GAS use in research (32) was proposed in 2016 in Archives of Physical Medicine and Rehabilitation, based on studies appraising the quality of scales generated in trials (16, 52). Therefore, the current paper does not focus on GAS in research, but readers can refer to the paper specifically discussing GAS in research (32) or to the new GAS checklist for research use (Personal communication. A rating system to evaluate the quality of goal attainment scales used as outcome measures in rehabilitation). In addition to using a GAS quality appraisal system (32), it seems crucial for adequate GAS quality and understanding of methodology that authors: (i) define precisely which GAS variant they used (see Fig. 2); (ii) always report if GAS is used as a PROM measure, i.e. “patient-reported goal attainment” (50, 53) or as a performance-based objective measure, i.e. “measured goal attainment” (3, 22, 54); (iii) report if GAS was set before randomization; (iv) report whether experimental and control groups had homogenous number and type of goals and the number of goals set per patient (note: higher correlation between goals and number of goals will affect T-scores) (56).
Applying the 2016 GAS quality guidelines (32), a recent systematic review showed the poor methodological rigour (mean quality of GAS was 4.7 out of 17 quality points) in using GAS in paediatric rehabilitation research (31). Also, not formally assessed, the same applies in adult rehabilitation. The most preoccupying finding of the review by Harpster et al. (31) was that the high quality of the trials (i.e. randomization, blinding, etc.) did not correlate with the quality of GAS methodology. This may suggest that: (i) reviewers and editors of journals are more concerned with the trial methodology than the quality of the outcome measure, even though both influence trial findings; (ii) there is insufficient awareness of the idiosyncratic nature of goal attainment scales, demonstrating different clinimetric properties, based on level of rigour used for its development; (iii) researchers tend to consider GAS as a valid scale, rather than a heterogeneous methodology to generate scales; (iv) GAS methodology variations and guidelines for research are not yet widely known. Harpster et al. found that only 20% of studies reported any kind of training for GAS use, and less than 10% reported reliability of the GAS generated within the trial.
Reliability of GAS remains a major challenge (15, 32, 51, 55) affected by: (i) the manner in which the scale is constructed. For example, the scale may not be reliable, due to non-equidistant levels, erroneous starting pre-intervention levels, goals/GAS levels that are too easy, an unspecified time-frame for goals attainment influencing the difficulty of attaining a specific goal at the generic post-intervention assessment time-point, etc.); (ii) rating reliability of scale (i.e. inter-rater reliability (IRR) is likely to be low if levels are not precisely described, if the scale uses subjective criteria for goal attainment with poor measurability, if GAS scales are multidimensional, and/or if there is no control for context of measurement). When authors report their trial or apply for funding, they need to convince readers, experts and reviewers of the reliability of the GAS set for the trial. Two objective ways to report a reliable IRR are to include a double rating of goal attainment during the participant’s performance, or a blinded a posteriori rating based on videotaped performance (Personal communication. Riding my bike, reading my watch, and tying my shoes: can CO-OP help children and young people with executive function deficits following acquired brain injury reach their goals? A replicated single case experimental study with randomized multiple baseline across participants and goals). If the GAS is used as a PROM (which should be avoided in research whenever goals can be transformed into a performance-based objective measure), IRR is not feasible, but reporting on the family’s or treating therapist’s perception of goal attainment can provide valuable information to support the client’s view.
From a pragmatic point of view, and in addition to trial requirements, protocols implementing rigorous GAS could consider: (i) adequate training and experience of investigators involved in GAS setting and definition; (ii) independent staff for (a) writing GAS scales (before randomization); (b) providing the intervention/therapy; (c) checking the quality (reliability and validity) of scales; (d) scoring the scales at the end of the intervention (with staff blind to the intervention and independent from those who wrote the GAS with the client); (e) repeated scoring of GAS at the end of the intervention to investigate the individual IRR of the scales (in that domain, that study, with those patients and those setters creating scales); (f) rating final GAS quality for reporting. Using a goal setter independent from the therapist could have advantages, but is not always optimal in terms of therapeutic alliance and commitment and it may be difficult for the therapist to deliver the therapy without having previously discussed its aims (and related means) with the client. Recent trial protocols, published after the publication of quality guidelines, lack focus on GAS rigour; however, some protocols consider the challenges of GAS measurement properties (16, 52, 54).
Original ways of using GAS in research contributing to trial reliability include: (i) randomizing goals to be trained vs goals on a waiting list to prove intervention specificity (56); (ii) using control GAS based on behaviours that are not related to the intervention, to ensure that the measured changes are due to the intervention and not just to a developmental effect, motivation effect or spontaneous recovery; (iii) using GAS as a generalization measure (i.e. have untrained goals to demonstrate progress after intervention aimed at other goals) (23, 42); (iv) writing a series of GAS for the same goal to increase validity and reliability (3). In all cases, it is essential that scales are set before randomization. This is because goal setters (client or therapist) are likely to be biased towards setting goals based on the intervention they have in mind, which would lead to GAS not being comparable across groups (see the section “Definition of 0 level, time-frame and means employed to attain the goal” above).
Finally, GAS is being developed in single-case experimental designs (SCED) and N-of-1 trials, where goal attainment is measured repeatedly across phases with and without intervention (57–60). Combining SCED and GAS methods is particularly promising, both in research and clinical practice (Personal communication. A proposed regulatory and ethical framework for single-case experimental design studies in rehabilitation research and clinical practice), especially in randomized multiple baseline across goals designs (61). In this SCED, 3 goals are set for a single participant. Randomization determines in which order and at which time-points each goal will begin to be trained (see, for example (62, 63)). Clinically, it is current and recommended practice not to pursue too many goals at the same time; hence, a staggered introduction of goals (and related goal-based interventions) in a single participant, through this type of design is close to current clinical practice, bridging research and clinical practice.
ADDITIONAL REFLECTIONS
It was not possible to report and synthesize all issues relevant to GAS application in PRM from the current literature; however, Table IV provides references for further reading on some of these issues.
| GAS, eHealth and Apps | |
| Positive and negative aspects | See supplemental material Table SIII. Negative and positive aspects of application of GAS, to help reflect on these aspects, especially before use of GAS as an outcome measure |
| Statistical aspects | Recommendations and precautions regarding statistical interpretation of GAS results (2, 30, 55, 94) |
| GAS with cognitive impairment | Using GAS with cognitive impairment: is essential even if intervention is not aimed at cognitive impairment (e.g. spasticity management after stroke), as associated cognitive comorbidities impact GAS management, from selecting realistic goals, to retaining, and implementing them. Cognitive abilities impact directly on goal achievement when functional performance is involved (98). Remembering personal goals and implementing them is particularly difficult for individuals with cognitive impairment (96, 97): deficits in executive function and memory can make it difficult to spontaneously plan, formulate and monitor progress towards goals. Difficulties with emotional regulation and cognitive impairment will also impact a person’s ability to feel a sense of energy or drive towards achieving goals. Aphasia and cognitive limitations may discourage therapist use of GAS, even if relevant and valuable (98–100), given that basic language (e.g. 2–3 word verbal cues) and non-verbal communication (e.g. gestures, sign language) can be used (43). Unfortunately, research exploring motor function interventions with GAS (e.g. in stroke), does not address cognitive limitations that impede goal retention, implementation and commitment. The use of meta-cognitive and/or behavioural rehabilitation approaches for patients with cognitive and/or behavioural impairments seems to be an interesting option to support the achievement of GAS goals (38, 67, 80, 82, 101). |
| Goal-focused rehabilitation | Implementation of GAS in routine clinical practice is not just about introducing personalized outcome-measures. It also provides a framework for patient/caregiver collaboration and engagement toward goal achievement through patient-centred rehabilitation. Planning of rehabilitation should be conducted according to patient priorities and follow-up meetings to provide individualized therapy based on patient goals. GAS implementation across clinical rehabilitation teams can rely on goal focused rehabilitation frameworks, i.e. using GAS as a mean to think about and plan personalized treatment (71, 72, 102, 103). |
LIMITS
This paper is intended as a toolbox and a practical guide to implement the GAS method with an understanding of the chosen variant and its consequences. As this paper is not based on a systematic review, other ways of using GAS could have been missed. The intent was not to provide a scoping review, although some of the topics and tools presented here could benefit in the future from such a methodology using a systematic review process, in specific PRM fields (given the abundance of GAS literature).
RECOMMENDATIONS AND CONCLUSION
GAS is relevant for both clinical practice and research. Its use promotes active engagement of patients in rehabilitation, while overcoming potential lack of sensitivity of individualized goals associated with standardized scale use. Depending on the level of methodological rigour implemented, it can be a sensitive personalized objective or a subjective, PROM, measure. Time associated with GAS administration can be overcome with the use of goal banks and/or goal identification aids (see Supplementary data Table SII). Goal coaching and support for acquisition are powerful goal attainment enhancers, which could also be aimed at use outside of goal-focused therapies. GAS is not a standardized scale, but a heterogeneous group of methodologies aiming at quantifying patient evolution on personal goals. Both clinicians and researchers wishing to use GAS with individuals should be aware of heterogeneity, idiosyncratic clinimetric properties, as well as positive and negative aspects of its application. Reliability and validity will be dependent on the experience of the goal setter in patient pathology and the interventions proposed, as well as their expertise in the GAS processes. Increased awareness is necessary for the appropriate selection of target behaviours, in order to avoid general goal attainment scales that are difficult to measure.
To guide the user, the authors propose both a framework for the use of GAS in clinical practice, when practitioners wish to provide client-centred and goal-directed therapies (see Fig. 4) and a framework for the use of GAS in research (Fig. 5). The latter conceptualizes the different steps in this process and highlights the reflections that need to be conducted when designing a study, as well as the variety of options from which the researcher can choose.
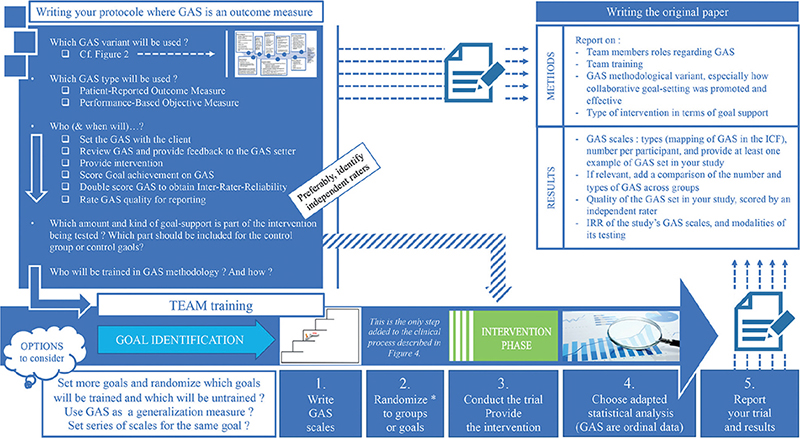
Fig. 5. Framework for the use of goal attainment scaling (GAS) in research. Randomization can be applied in different ways: the researcher can decide to set multiple goals and then randomize the ones to be trained and the controls that will not be trained; or the researcher can set multiple goals and randomize the order in which each of them is trained, as can be done in single-case experimental designs (SCEDs), with multiple baselines across goals; or randomization can be applied between groups.
Reviewers and editors are encouraged to appraise the quality of goal attainment scales when used as outcome measures in clinical trials.
REFERENCES
- Kiresuk TJ, Smith A, Cardillo JE (eds). Goal attainment scaling. 1st edition. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 1994.
- Tennant A. Goal attainment scaling: current methodological challenges. Disabil Rehabil 2007; 29: 1583–1588.
- Steenbeek D, Ketelaar M, Lindeman E, Galama K, Gorter JW. Interrater reliability of goal attainment scaling in rehabilitation of children with cerebral palsy. Arch Phys Med Rehabil 2010; 91: 429–435.
- Krasny-Pacini A, Hiebel J, Pauly F, Godon S, Chevignard M. Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med 2013; 56: 212–230.
- Scobbie L, Wyke S, Dixon D. Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin Rehabil 2009; 23: 321–333.
- Levack WM, Weatherall M, Hay-Smith EJ, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev. 2015; 20: 1–166.
- Löwing K, Bexelius A, Brogren Carlberg E. Activity focused and goal directed therapy for children with cerebral palsy – do goals make a difference? Disabil Rehabil 2009; 31: 1808–1816.
- Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil 2009; 23: 352–361.
- Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil 2009; 23: 362–370.
- Malec JF. Goal attainment scaling in rehabilitation. Neuropsychol Rehabil 1999; 9: 253–275.
- Schlosser RW. Goal attainment scaling as a clinical measurement technique in communication disorders: a critical review. J Commun Disord 2004; 37: 217–239.
- Konovalov NA, Nazarenko AG, Krut’ko AV, Glukhikh DL, Durni P, Duris M, et al. [Results of surgical treatment for lumbar spine segmental instability]. Zh Vopr Neirokhir Im N N Burdenko 2017; 81: 69–80 (in Russian).
- Bouwens SFM, van Heugten CM, Verhey FRJ. Review of goal attainment scaling as a useful outcome measure in psychogeriatric patients with cognitive disorders. Dement Geriatr Cogn Disord 2008; 26: 528–540.
- Vu M, Law AV. Goal-attainment scaling: a review and applications to pharmacy practice. Res Soc Adm Pharm 2012; 8: 102–121.
- Gaasterland CMW, Jansen-van der Weide MC, Weinreich SS, van der Lee JH. A systematic review to investigate the measurement properties of goal attainment scaling, towards use in drug trials. BMC Med Res Methodol 2016; 16: 99.
- Ruble L, McGrew JH, Toland MD. Goal attainment scaling as an outcome measure in randomized controlled trials of psychosocial interventions in autism. J Autism Dev Disord 2012; 42: 1974–1983.
- Ruble LA, Dalrymple NJ, McGrew JH. The effects of consultation on individualized education program outcomes for young children with autism: the collaborative model for promoting competence and success. J Early Interv 2010; 32: 286–301.
- Palisano RJ. Validity of goal attainment scaling in infants with motor delays. Phys Ther 1993; 73: 651–658; discussion 658–660.
- Lowe K, Novak I, Cusick A. Repeat injection of botulinum toxin A is safe and effective for upper limb movement and function in children with cerebral palsy. Dev Med Child Neurol 2007; 49: 823–829.
- Bovend’Eerdt TJ, Dawes H, Sackley C, Izadi H, Wade DT. An integrated motor imagery program to improve functional task performance in neurorehabilitation: a single-blind randomized controlled trial. Arch Phys Med Rehabil 2010; 91: 939–946.
- Ten Berge SR, Boonstra AM, Dijkstra PU, Hadders-Algra M, Haga N, Maathuis CGB. A systematic evaluation of the effect of thumb opponens splints on hand function in children with unilateral spastic cerebral palsy. Clin Rehabil 2012; 26: 362–371.
- Steenbeek D, Meester-Delver A, Becher JG, Lankhorst GJ. The effect of botulinum toxin type A treatment of the lower extremity on the level of functional abilities in children with cerebral palsy: evaluation with goal attainment scaling. Clin Rehabil 2005; 19: 274–282.
- Krasny-Pacini A, Limond J, Evans J, Hiebel J, Bendjelida K, Chevignard M. Context-sensitive goal management training for everyday executive dysfunction in children after severe traumatic brain injury. J Head Trauma Rehabil 2014; 29: E49–E64.
- Phillips MF, Robertson Z, Killen B, White B. A pilot study of a crossover trial with randomized use of ankle-foot orthoses for people with Charcot-Marie-tooth disease. Clin Rehabil 2012; 26: 534–544.
- Grant M, Ponsford J, Bennett PC. The application of goal management training to aspects of financial management in individuals with traumatic brain injury. Neuropsychol Rehabil 2012; 22: 852–873.
- Bergsma D, Baars-Elsinga A, Sibbel J, Lubbers P, Visser-Meily A. Visual daily functioning of chronic stroke patients assessed by goal attainment scaling after visual restorative training: an explorative study. Top Stroke Rehabil 2014; 21: 400–412.
- Mall V, Heinen F, Siebel A, Bertram C, Hafkemeyer U, Wissel J, et al. Treatment of adductor spasticity with BTX-A in children with CP: a randomized, double-blind, placebo-controlled study. Dev Med Child Neurol 2006; 48: 10–13.
- Lowe K, Novak I, Cusick A. Low-dose/high-concentration localized botulinum toxin A improves upper limb movement and function in children with hemiplegic cerebral palsy. Dev Med Child Neurol 2006; 48: 170–175.
- Turner-Stokes L, Baguley IJ, De Graaff S, Katrak P, Davies L, McCrory P, et al. Goal attainment scaling in the evaluation of treatment of upper limb spasticity with botulinum toxIn: a secondary analysis from a double-blind placebo-controlled randomized clinical trial. J Rehabil Med Off J UEMS Eur Board Phys Rehabil Med 2010; 42: 81–89.
- Stucki G, Daltroy L, Katz JN, Johannesson M, Liang MH. Interpretation of change scores in ordinal clinical scales and health status measures: the whole may not equal the sum of the parts. J Clin Epidemiol 1996; 49: 711–717.
- Harpster K, Sheehan A, Foster EA, Leffler E, Schwab SM, Angeli JM. The methodological application of goal attainment scaling in pediatric rehabilitation research: a systematic review. Disabil Rehabil 2019; 41: 2855–2864.
- Krasny-Pacini A, Evans J, Sohlberg MM, Chevignard M. Proposed criteria for appraising goal attainment scales used as outcome measures in rehabilitation research. Arch Phys Med Rehabil 2016; 97: 157–170.
- Ottenbacher KJ, Cusick A. Goal attainment scaling as a method of clinical service evaluation. Am J Occup Ther 1990; 44: 519–525.
- King GA, McDougall J, Palisano RJ, Gritzan J, Tucker MA. Goal Attainment Scaling: its use in evaluating pediatric therapy programs. Phys Occup Ther Pediatr 2000; 19: 31–52.
- Kiresuk TJ, Smith A, Cardillo JE (editors). Goal attainment scaling: applications, theory, and measurement. New York: Psychology Press; 2013.
- Kiresuk TJ, Sherman RE. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment Health J 1968; 4: 443–453.
- Churilov I, Brock K, Churilov JM, Sutton E, Murphy D, MacIsaac RJ, et al. Goal attainment scaling outcomes in general inpatient rehabilitation: association with functional independence and perceived goal importance and difficulty. J Rehabil Med 2020; 52: jrm00054.
- Ghorbani N, Rassafiani M, Izadi-Najafabadi S, Yazdani F, Akbarfahimi N, Havaei N, et al. Effectiveness of cognitive orientation to (daily) occupational performance (CO-OP) on children with cerebral palsy: a mixed design. Res Dev Disabil 2017; 71: 24–34.
- Koski J, Richards LG. Reliability and sensitivity to change of goal attainment scaling in occupational therapy nonclassroom educational experiences. Am J Occup Ther 2015; 69: 6912350030p1–6912350030p5.
- Löwing K, Thews K, Haglund-Åkerlind Y, Gutierrez-Farewik EM. Effects of botulinum toxin-A and goal-directed physiotherapy in children with cerebral palsy GMFCS Levels I & II. Phys Occup Ther Pediatr 2017; 37: 268–282.
- Vroland-Nordstrand K, Eliasson A-C, Jacobsson H, Johansson U, Krumlinde-Sundholm L. Can children identify and achieve goals for intervention? A randomized trial comparing two goal-setting approaches. Dev Med Child Neurol 2016; 58: 589–596.
- Willis C, Nyquist A, Jahnsen R, Elliott C, Ullenhag A. Enabling physical activity participation for children and youth with disabilities following a goal-directed, family-centred intervention. Res Dev Disabil 2018; 77: 30–39.
- Casey AF, Pickard V, Ullrich C, MacNeil Z. An adapted walking intervention for a child with Pitt Hopkins syndrome. Disabil Rehabil Assist Technol 2017; 13: 25–30.
- Rosenberg L, Maeir A, Gilboa Y. Feasibility study of a therapeutic mobility summer camp for children with severe cerebral palsy: power fun. Phys Occup Ther Pediatr 2020; 40: 395–409.
- Krasny-Pacini A, Pauly F, Hiebel J, Godon S, Isner-Horobeti M-E, Chevignard M. Feasibility of a shorter Goal Attainment Scaling method for a pediatric spasticity clinic – the 3-milestones GAS. Ann Phys Rehabil Med 2017; 60: 249–257.
- Zaza C, Stolee P, Prkachin K. The application of goal attainment scaling in chronic pain settings. J Pain Symptom Manage 1999; 17: 55–64.
- World Health Organization (WHO). International Classification of Functioning, Disability and Health (ICF). Geneva: WHO; 2001. [accessed Dec 15, 2015]. Available from: http://www.who.int/classifications/icf/en/
- Turner-Stokes L, Ashford S, Esquenazi A, Wissel J, Ward AB, Francisco G, et al. A comprehensive person-centered approach to adult spastic paresis: a consensus-based framework. Eur J Phys Rehabil Med 2018; 54: 605–617.
- Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther Rev Can Ergother 1990; 57: 82–87.
- Herdman KA, Vandermorris S, Davidson S, Au A, Troyer AK. Comparable achievement of client-identified, self-rated goals in intervention and no-intervention groups: reevaluating the use of goal attainment scaling as an outcome measure. Neuropsychol Rehabil 2019; 29: 1600–1610.
- Steenbeek D, Ketelaar M, Galama K, Gorter JW. Goal attainment scaling in paediatric rehabilitation: a critical review of the literature. Dev Med Child Neurol 2007; 49: 550–556.
- Keenan S, King G, Curran CJ, McPherson A. Effectiveness of experiential life skills coaching for youth with a disability. Phys Occup Ther Pediatr 2014; 34: 119–131.
- Dolovich L, Oliver D, Lamarche L, Agarwal G, Carr T, Chan D, et al. A protocol for a pragmatic randomized controlled trial using the Health Teams Advancing Patient Experience: Strengthening Quality (Health TAPESTRY) platform approach to promote person-focused primary healthcare for older adults. Implement Sci IS 2016; 11: 49.
- Estival S, Krasny-Pacini A, Laurier V, Maugard C, Thuilleaux D, Postal V. Cognitive training targeting planning dysfunction in adults with prader-willi syndrome: brief report of a study protocol. Dev Neurorehabilitation 2019; 22: 569–575.
- Urach S, Gaasterland C, Posch M, Jilma B, Roes K, Rosenkranz G, et al. Statistical analysis of goal attainment scaling endpoints in randomised trials. Stat Methods Med Res 2019; 28: 1893–1910.
- Behn N, Marshall J, Togher L, Cruice M. Setting and achieving individualized social communication goals for people with acquired brain injury (ABI) within a group treatment. Int J Lang Commun Disord 2019; 54: 828–840.
- Bard-Pondarre R, Vuillerot C, Al-Abiad N, Verdun S, Chabrier S, Chaléat-Valaer E. BB-Bim – early bimanual stimulation for infants at risk of unilateral cerebral palsy: a randomized, multiple baseline, single-case study. Am J Occup Ther; under revision.
- Krasny-Pacini A, Evans J. Single-case experimental designs to assess intervention effectiveness in rehabilitation: a practical guide. Ann Phys Rehabil Med 2018; 61: 164–179.
- Tate RL, Rosenkoetter U, Wakim D, Sigmundsdottir L, Doubleday J, Togher L, et al. The Risk of Bias in N-of-1 Trials (RoBiNT) Scale: an expanded manual for the critical appraisal of single-case reports. Sydney: The PsycBITE Group; 2015.
- Tate RL, Perdices M, Rosenkoetter U, Shadish W, Vohra S, Barlow DH, et al. The Single-Case Reporting Guideline In BEhavioural Interventions (SCRIBE) 2016 Statement. Phys Ther 2016; 96: e1–e10.
- Krasny-Pacini A. Single-case experimental designs for child neurological rehabilitation and developmental disability research. Dev Med Child Neurol 2023; dmcn.15513.
- Tate RL, Wakim D, Sigmundsdottir L, Longley W. Evaluating an intervention to increase meaningful activity after severe traumatic brain injury: a single-case experimental design with direct inter-subject and systematic replications. Neuropsychol Rehabil 2020; 30: 641–672.
- Lebrault H, Chavanne C, Abada G, Latinovic B, Varillon S, Bertrand A-F, et al. Exploring the use of the Cognitive Orientation to daily Occupational Performance approach (CO-OP) with children with executive functions deficits after severe acquired brain injury: a single case experimental design study. Ann Phys Rehabil Med 2021; 64: 101535.
- Bard-Pondarré R, Castan C. Intérêts et limites de l’utilisation des tests quantitatifs d’évaluation fonctionnelle du membre supérieur de la personne paralysée cérébrale. Mot Cérébrale Réadapt Neurol Dév 2017; 38: 59–70.
- Culley C, Evans JJ. SMS text messaging as a means of increasing recall of therapy goals in brain injury rehabilitation: a single-blind within-subjects trial. Neuropsychol Rehabil 2010; 20: 103–119.
- Hart T, Hawkey K, Whyte J. Use of a portable voice organizer to remember therapy goals in traumatic brain injury rehabilitation: a within-subjects trial. J Head Trauma Rehabil 2002; 17: 556–570.
- Kramer JM, Helfrich C, Levin M, Hwang I-T, Samuel PS, Carrellas A, et al. Initial evaluation of the effects of an environmental-focused problem-solving intervention for transition-age young people with developmental disabilities: Project TEAM. Dev Med Child Neurol 2018; 60: 801–809.
- Bexelius A, Carlberg EB, Löwing K. Quality of goal setting in pediatric rehabilitation: a SMART approach. Child Care Health Dev 2018; 44: 850–856.
- Buitrago JA, Bolaños AM, Caicedo Bravo E. A motor learning therapeutic intervention for a child with cerebral palsy through a social assistive robot. Disabil Rehabil Assist Technol 2020; 15: 357–362.
- Keegan LC, Murdock M, Suger C, Togher L. Improving natural social interaction: Group rehabilitation after traumatic brain injury. Neuropsychol Rehabil 2020; 30: 1497–1522.
- Ostensjø S, Oien I, Fallang B. Goal-oriented rehabilitation of preschoolers with cerebral palsy – a multi-case study of combined use of the Canadian Occupational Performance Measure (COPM) and the Goal Attainment Scaling (GAS). Dev Neurorehabil 2008; 11: 252–259.
- Ketelaar M, Vermeer A, Hart H, van Petegem-van Beek E, Helders PJ. Effects of a functional therapy program on motor abilities of children with cerebral palsy. Phys Ther 2001; 81: 1534–1545.
- Emmons RA. Striving and feeling: Personal goals and subjective well-being. En: The psychology of action: linking cognition and motivation to behavior. New York, NY: The Guilford Press; 1996, p. 313–337.
- van Vulpen LF, de Groot S, Rameckers EAA, Becher JG, Dallmeijer AJ. Effectiveness of functional power training on walking ability in young children with cerebral palsy: study protocol of a double-baseline trial. Pediatr Phys Ther Off Publ Sect Pediatr Am Phys Ther Assoc 2017; 29: 275–282.
- Ylvisaker M, McPherson K, Kayes N, Pellett E. Metaphoric identity mapping: facilitating goal setting and engagement in rehabilitation after traumatic brain injury. Neuropsychol Rehabil 2008; 18: 713–741.
- Schweiger Gallo I, Gollwitzer PM. Implementation intentions: a look back at fifteen years of progress. Psicothema 2007; 19: 37–42.
- Orbell S, Hodgkins S, Sheeran P. Implementation intentions and the theory of planned behavior. Pers Soc Psychol Bull 1997; 23: 945–954.
- da Silva MAV, São-João TM, Brizon VC, Franco DH, Mialhe FL. Impact of implementation intentions on physical activity practice in adults: a systematic review and meta-analysis of randomized clinical trials. PLoS One 2018; 13: e0206294.
- Radomski MV, Giles G, Finkelstein M, Owens J, Showers M, Zola J. Implementation intentions for self-selected occupational therapy goals: two case reports. Am J Occup Ther 2018; 72: 7203345030p1–7203345030p6.
- Levine B, Robertson IH, Clare L, Carter G, Hong J, Wilson BA, et al. Rehabilitation of executive functioning: an experimental-clinical validation of goal management training. J Int Neuropsychol Soc JINS 2000; 6: 299–312.
- McPherson KM, Kayes N, Weatherall M. A pilot study of self-regulation informed goal setting in people with traumatic brain injury. Clin Rehabil 2009; 23: 296–309.
- Miotto EC, Evans JJ, Souza de Lucia MC. Rehabilitation of executive dysfunction: a controlled trial of an attention and problem solving treatment group. Neuropsychol Rehabil 2009; 19: 517–540.
- Gaffney E, Gaffney K, Bartleson L, Dodds C. Goal attainment scaling made easy with an app: GOALed. Pediatr Phys Ther Off Publ Sect Pediatr Am Phys Ther Assoc 2019; 31: 225–230.
- Kucheria P, Moore Sohlberg M, Machalicek W, Seeley J, DeGarmo D. A single-case experimental design investigation of collaborative goal setting practices in hospital-based speech-language pathologists when provided supports to use motivational interviewing and goal attainment scaling. Neuropsychol Rehabil 2022; 32: 579–610.
- O’Halloran PD, Blackstock F, Shields N, Holland A, Iles R, Kingsley M, et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin Rehabil 2014; 28: 1159–1171.
- William MR, Rollnick S. Motivational interviewing, third edition: helping people change. 3rd edn. New York, NY: Guilford Press; 2012.
- Ponsford J, Lee NK, Wong D, McKay A, Haines K, Alway Y, et al. Efficacy of motivational interviewing and cognitive behavioral therapy for anxiety and depression symptoms following traumatic brain injury. Psychol Med 2016; 46: 1079–1090.
- Ogawa T, Omon K, Yuda T, Ishigaki T, Imai R, Ohmatsu S, et al. Short-term effects of goal-setting focusing on the life goal concept on subjective well-being and treatment engagement in subacute inpatients: a quasi-randomized controlled trial. Clin Rehabil 2016; 30: 909–920.
- Siegert RJ, McPherson KM, Taylor WJ. Toward a cognitive-affective model of goal-setting in rehabilitation: is self-regulation theory a key step? Disabil Rehabil 2004; 26: 1175–1183.
- Siegert RJ, Taylor WJ. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil Rehabil 2004; 26: 1–8.
- Siegert RJ, Levack WMM (eds). Rehabilitation goal setting: theory, practice and evidence. 1st edn. Boca Raton, FL: CRC Press; 2014.
- Linehan MM. DBT® skills training manual. 2nd edn. New York: Guilford Press; 2015.
- Javadi D, Lamarche L, Avilla E, Siddiqui R, Gaber J, Bhamani M, et al. Feasibility study of goal setting discussions between older adults and volunteers facilitated by an eHealth application: development of the Health TAPESTRY approach. Pilot Feasibility Stud 2018; 4: 184.
- Cardillo JE, Smith A. Psychometric issues. In: Kiresuk TJ, Smith A, Cardillo J (editors) Goal attainment scaling: applications, theory, and measurement. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1994, p. 199.
- Jung Y, Sim J, Park J, Kim J, Kim M. Usefulness of goal attainment scaling in intensive stroke rehabilitation during the subacute stage. Ann Rehabil Med 2020; 44: 181–194.
- Evans JJ. Goal setting during rehabilitation early and late after acquired brain injury. Curr Opin Neurol 2012; 25: 651–655.
- Hart T, Evans J. Self-regulation and goal theories in brain injury rehabilitation. J Head Trauma Rehabil 2006; 21: 142–155.
- Sherratt S, Worrall L, Pearson C, Howe T, Hersh D, Davidson B. “Well it has to be language-related”: speech-language pathologists’ goals for people with aphasia and their families. Int J Speech Lang Pathol 2011; 13: 317–328.
- Hersh D, Worrall L, Howe T, Sherratt S, Davidson B. SMARTER goal setting in aphasia rehabilitation. Aphasiology 2012; 26: 220–233.
- Worrall L, Sherratt S, Rogers P, Howe T, Hersh D, Ferguson A, et al. What people with aphasia want: their goals according to the ICF. Aphasiology 2011; 25: 309–322.
- Gould KR, Ponsford JL, Hicks AJ, Hopwood M, Renison B, Feeney TJ. Positive behaviour support for challenging behaviour after acquired brain injury: an introduction to PBS + PLUS and three case studies. Neuropsychol Rehabil 2021; 31: 57–91.
- Ahl LE, Johansson E, Granat T, Carlberg EB. Functional therapy for children with cerebral palsy: an ecological approach. Dev Med Child Neurol 2005; 47: 613–619.
- Sorsdahl AB, Moe-Nilssen R, Kaale HK, Rieber J, Strand LI. Change in basic motor abilities, quality of movement and everyday activities following intensive, goal-directed, activity-focused physiotherapy in a group setting for children with cerebral palsy. BMC Pediatr 2010; 10: 26.