ORIGINAL REPORT
ADHERENCE TO GUIDELINES FOR ACUTE REHABILITATION IN THE NORWEGIAN TRAUMA PLAN
Christoph SCHÄFER, MD1–4, Håkon ØGREID MOKSNES, MD1,4, Mari S. RASMUSSEN, PhD1,5, Torgeir HELLSTRØM, MD, PhD1, Helene LUNDGAARD SOBERG, PhD1,5, Olav RØISE, MD, PhD6,7, Cecilie RØE, MD, PhD1,4,7, Shirin FRISVOLD, MD, PhD2,8, Kristian BARTNES MD, PhD2,9, Pål AKSEL NÆSS, MD, PhD7,10, Christine GAARDER, MD, PhD7,10, Eirik HELSETH, MD, PhD7,11, Cathrine BRUNBORG, MSc12, Nada ANDELIC, MD, PhD1,4 and Audny ANKE MD, PhD2–4
From the 1Department of Physical Medicine and Rehabilitation, Oslo University Hospital, Oslo, 2Faculty of Health Sciences, Department of Clinical Medicine, UiT The Arctic University of Norway, Tromsø, 3Department of Rehabilitation, University Hospital of North Norway, Tromsø, 4Institute of Health and Society, Research Centre for Habilitation and Rehabilitation Models & Services (CHARM), Faculty of Medicine, University of Oslo, 5Faculty of Health Sciences, Oslo Metropolitan University, 6Norwegian Trauma Registry, Division of Orthopaedic Surgery, Oslo University Hospital, Oslo, 7Institute of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, 8Department of Intensive Care Medicine and 9Division of Cardiothoracic and Respiratory Medicine, University Hospital North Norway, Tromsø, 10Department of Traumatology, Oslo University Hospital, 11Department of Neurosurgery, Division of Emergencies and Critical Care, Department of Research and Development and 12Oslo Centre for Biostatistics and Epidemiology, Research Support Services, Oslo, Norway
Objective: To evaluate adherence to 3 central operational recommendations for acute rehabilitation in the Norwegian trauma plan.
Methods: A prospective multi-centre study of 538 adults with moderate and severe trauma with New Injury Severity Score > 9.
Results: Adherence to the first recommendation, assessment by a physical medicine and rehabilitation physician within 72 h following admission to the intensive care unit (ICU) at the trauma centre, was documented for 18% of patients. Adherence to the second recommendation, early rehabilitation in the intensive care unit, was documented for 72% of those with severe trauma and ≥ 2 days ICU stay. Predictors for early rehabilitation were ICU length of stay and spinal cord injury. Adherence to the third recommendation, direct transfer of patients from acute ward to a specialized rehabilitation unit, was documented in 22% of patients, and occurred more often in those with severe trauma (26%), spinal cord injury (54%) and traumatic brain injury (39%). Being employed, having head or spinal chord injury and longer ICU stay were predictors for direct transfer to a specialized rehabilitation unit.
Conclusion: Adherence to acute rehabilitation guidelines after trauma is poor. This applies to documented early assessment by a physical medicine and rehabilitation physician, and direct transfer from acute care to rehabilitation after head and extremity injuries. These findings indicate a need for more systematic integration of rehabilitation in the acute treatment phase after trauma.
LAY ABSTRACT
Three recommendations for acute rehabilitation in the Norwegian trauma plan were evaluated in 538 adults with moderate to severe injuries. Recommendation one: Examination by a rehabilitation physician within 72 h after hospital admission. This was documented in 18% of the patients. Recommendation two: Start of early rehabilitation in the intensive care unit. This was given to 72% of those with severe trauma. Early rehabilitation was more frequent in patients with spinal cord injury, and with long intensive care stays. Recommendation three: Patients are directly transferred from acute care in the trauma centre to specialized rehabilitation. This was followed for 22% of the patients. This happened more often in patients with severe injuries, spinal cord injury and brain injury. Being in work and longer intensive care stays increased the probability for direct transfer. Conclusion: Overall compliance with the guidelines is poor, except for early therapist rehabilitation in the intensive care unit.
Key words: guideline adherence; continuity of patient care; health service research; multiple trauma; rehabilitation; trauma centres; wounds and injuries; pathway.
Citation: J Rehabil Med 2023; 55: jrm6552. DOI: https://doi.org/10.2340/jrm.v55.6552.
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Apr 20, 2023; Published: Jun 27, 2023
Correspondence address: Christoph Schäfer, Department of Physical Medicine and Rehabilitation, University Hospital of North Norway, PO Box 100, NO-9038 Tromsø, Norway. E-mail: christoph.schafer@unn.no
Trauma is a significant cause of death and disability worldwide (1). Traffic accidents and falls are major causes of injuries and lead to many years lived with disability (2). Many individuals who have undergone severe trauma live with residual impairments several years later (3). The sequelae of such trauma may affect physical, mental, cognitive and social functioning (4, 5). Provision of rehabilitation services varies (6, 7) and guidelines for rehabilitation management in patients with trauma are often not implemented (8). Notably, current practice for rehabilitation of patients with orthopaedic trauma is variable (9).
World Health Organization (WHO) Guidelines for Essential Trauma care recommend systematic rehabilitation as part of trauma care systems to maximize functional recovery (10). Historically, establishing dedicated spinal injuries centres profoundly improved long-term survival (11, 12). Integration of rehabilitation into a multiple-trauma care system was associated with reduced length of stay, mortality and better functional outcomes (13, 14). Kreitzer et al. (15) found that a majority of healthcare workers in acute trauma care support early rehabilitation interventions, defined as “acute therapies, such as range of movement, strengthening, ambulation, neurostimulation”. A “fast track model” for multi-trauma patients, presented by Bouman et al. (16), integrating rehabilitation into acute care, led to faster recovery. However, consulting multidisciplinary teams have not shown benefit over standard care (17).
Patients with severe injuries, specifically with pelvic, lower extremity, spine or head trauma, are more frequently transferred to inpatient rehabilitation than patients with minor-to-moderate injuries or injuries in other organ regions (18). For patients with traumatic brain injury (TBI), basic intensive care unit (ICU) interventions, such as mobilization, can improve recovery (19), and direct transfer from acute care to specialized rehabilitation improves functional outcome (7, 20–22). In their review, Naess et al. defined “early rehabilitation” as interdisciplinary team rehabilitation within 1 week of admission (23). This approach has shown favourable outcomes compared with delayed rehabilitation for patients with TBI (20, 24, 25).
Norwegian trauma care guidelines from 2017 give recommendations for acute rehabilitation after severe trauma based on best practise and available evidence (26).Three central operational recommendations are set out in these guidelines: (i) assessment by a specialist in rehabilitation medicine within 72 h following admission to the ICU at the trauma centre; (ii) early rehabilitation starting in the ICU; (iii) prioritization of direct transfer of patients from the acute care department in the trauma centre to a specialized rehabilitation unit.
The aim of this study is to evaluate adherence to the Norwegian recommendations for acute rehabilitation in a population-based study of patients with moderate to severe trauma at 2 trauma centres in Norway. Adherence to the 3 operational recommendations in the guidelines was investigated in association with sociodemographic factors, type and severity of injury, substance use at time of injury, and length of ICU stay.
METHODS
Design and setting
A prospective, multi-centre, observational study was conducted at 2 university trauma centres in Norway: Oslo University Hospital (OUH) and the University Hospital of North Norway (UNN), which are the trauma centres in the Southeast and Northern regions of Norway, respectively. A protocol article for the main study was published in 2021 (27). The study was approved by the Committee for Medical Research Ethics, Health Region South East (reference number 31676) and the The Data Protection Officers at OUH and UNN (approval number 19/26515 and 02423). The STROBE checklist was used to report this study.
Participants
The study included patients aged 18 years or older, resident in Norway, admitted directly to the regional trauma centres or transferred from local hospitals within 72 h after injury, with at least a 2-day hospital stay and a New Injury Severity Score (NISS) > 9. The 1-year inclusion period was from 1 January 2020 to 31 December 2020 at OUH and from 1 February 2020 to 31 January 2021 at UNN. The NISS score criteria pertain to patients with moderate to profound injuries. Exclusion criteria for the current study were age below 18 years, non-Norwegian residents, insufficient command of Norwegian/English language and death during the stay in the acute departments of the trauma centre. Patients, or their relatives if patients were unable to consent themselves, were informed orally about the study and via a written form and asked to provide written consent.
Data collection
Patients were identified by the project’s physicians through participation in trauma department meetings for reporting and planning action related to trauma patients, lists on new hospitalized patients registered by the trauma department, and search performed in the medical record system using an admission diagnosis of trauma. Patients identified through these sources were mainly those who were admitted with trauma team activation on arrival at hospital. Patients who were admitted to hospital with an activated trauma team, and otherwise identified patients who fulfilled the inclusion criteria, were assessed. The study physicians, who are certified Abbreviated Injury Scale scores (AIS) registrars, estimated AIS and calculated NISS on a daily basis from Monday to Friday for eligibility for study inclusion. In Norway the 2008 update of the 2005 version of the AIS is used in the trauma register (28). The AIS codes the body region affected and the severity of each injury. Injury severity is graded 1–6, where 1 is a minor and 6 a maximal injury. Injuries graded 1–2 were classified as minor to moderate and injuries graded 3–6 as severe to maximal (28). The NISS is a summary measure of anatomical injury and is defined as the sum of the squares of the AIS scores of each patient’s 3 most severe injuries, regardless of the body region in which they occur (29). AIS scores received from the local trauma registers at OUH and UNN were used for analysis. A NISS score of 9–15 indicates moderate injury, and NISS > 15 indicates severe injury (30). Pre-injury health was estimated with the Norwegian version of the American Society of Anaesthesiologists Physical Status Classification System (ASA), as used in the definition catalogue for the national Norwegian Trauma Register (31). Pre-injury ASA was categorized into healthy/without substantial functional limitations (score I–II) and moderate disease/disability to severe disease/disability (score III–V) (32).
Demographic variables collected from the patient’s electronic records were sex, age, living situation, duration of education, and occupation. Missing data about participants’ personal characteristics were obtained in the 6-month follow-up interviews. Clinical data obtained from patients’ records were diagnoses, non-surgical treatment, length of stay in the ICU, and disciplines and professions involved during acute treatment. Information about the type of accident was also registered.
Assessment by a physical medicine and rehabilitation physician in the ICU within 72 h after admission according to the guidelines was counted when documented in the electronic medical records. The study considered all documented interventions by therapeutic professions provided to the patients in the ICU as acute rehabilitation services. Therapist treatment in the ICU was defined as treatment by 1 therapeutic professional in addition to physicians and nurses. Therapeutic professionals were physiotherapists, occupational therapists, social workers, psychologists and speech therapists. The study registered the first involved professional and all types of professionals involved. Two or more professions involved, in addition to physicians and nurses, was considered as multidisciplinary intervention. Furthermore, the number of contacts while patients were under acute care was noted. Discharge destinations from acute care, defined as treatment in the (neuro-) ICU or surgical wards (mainly neurosurgery, orthopaedics, and thoracic surgery) at the trauma centre were defined as home, local hospital, rehabilitation unit or nursing home/others. Rehabilitation was defined as treatment in specialized hospital departments or specialized rehabilitation institutions.
Statistical analysis
IBM SPSS Statistics Version 28 (IBM Corp:, Armonk, NY, USA) was used for statistical analysis. Descriptive data are presented as proportions (percentages), medians with range and means with standard deviation (SD). Univariate and multivariable binary logistic regression analyses were used to test the association between independent variables and the outcome variables: (i) acute ICU therapist treatment received or not; and (ii) direct or not direct transfer from acute care in the trauma centre to rehabilitation. “Not direct transfer” was discharge to home, local hospital or nursing home/other. Since all patients with spinal cord injury received acute ICU therapist treatment, a regression analysis could not be performed for this variable and the association was computed with Fisher’s exact test. All variables were included both in the univariate and the multivariable models based on prior knowledge from the literature and by expert opinion. We present here the full multivariable model without subsequent elimination of variables. The following sociodemographic and injury-related factors were included: patients’ age, sex, living situation (living alone/not living alone), work situation (working or studying/not working or pensioned), educational level (high education > 13 years/lower education ≤ 13 years), pre-injury ASA (dichotomized into score 1–2 vs 3–4), substance use at the time of injury (yes/no), and the acute injury-related variables type and severity of injuries. The acute injury variables were the NISS, spinal cord injury (yes/no), and AIS scores of 3–5 of the defined body regions (yes/no). The results are given as odds ratios (ORs) with 95% confidence interval (95% CI). Level of significance was set at p < 0.05. The degree of multicollinearity was checked using the correlation matrix and Spearman’s correlation coefficient ≥ 0.7 as a cut-off. Model fit was assessed with the Hosmer and Lemeshow goodness-of-fit test, and the degree of pseudo-explained variance was reported according to Nagelkerke R2.
RESULTS
Patient characteristics
In total, 538 patients with moderate or severe trauma were included in the study (see Fig. 1 for inclusion process). The main reason for exclusion was NISS < 10. Of 647 eligible adult participants, 109 (17%) did not respond or declined participation. There were no differences considering age and sex between non-responders/decliners and those included in the study (median age 54 years (range 18–95) vs 53 years (range 18–93) and proportion of women 26% vs 24%, respectively).
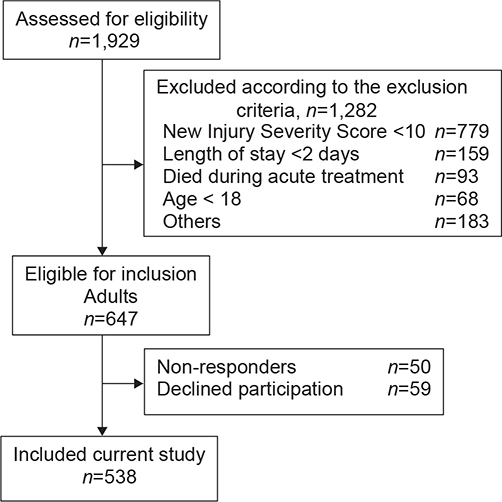
Fig. 1. Study inclusion flowchart.
As shown in Table I, 40% of participants had higher education, defined as more than 13 years at school, and 56% were working or studying at the time of injury. Injury-related characteristics are shown in Table II. Falls (41%) and traffic accidents (38%) were the most common causes of injury. Median NISS was 22 (range 10–75), and 76% of participants had a NISS of 16 or above, corresponding to severe injuries. Head (46%), thorax (34%) and extremities (18%) were the regions with the largest proportion of AIS scores of 3–5. Thirty-nine participants (7%) had spinal cord injuries. Eighty-eight percent of patients were treated in the ICU (Table III). Therapist treatment in the acute departments included: 71% received physiotherapy, 7% had occupational therapy, 33% had contact with social workers, and 16% met with psychologists.
| Participants N=538 | |
| Type of accident, n (%) | |
| Transport | 205 (38) |
| Fall | 220 (41) |
| Violence | 18 (3) |
| Other | 95 (18) |
| Substance use at time of the accident, n (%) | 129 (24) |
| Pre-injury ASA, n (%) | |
| Healthy (ASA I) | 267 (50) |
| Moderate disease, no disability (ASA II) | 202 (38) |
| Severe disease, disability (ASA III–V) | 69 (13) |
| Injury Severity Score (ISS) | |
| Median (range) | 17 (4–66) |
| ISS 16 or above, n (%) | 297 (55) |
| New Injury Severity Score (NISS) | |
| Median (range) | 22 (10–75) |
| Moderate NISS 10–15, n (%) | 127 (24) |
| Severe NISS 16–75, n (%) | 411 (76) |
| Abbreviated Injury Scale (AIS) 1–5, n (%)a | |
| Head | 248 (46) |
| Face | 180 (33) |
| Neck | 22 (4) |
| Thorax | 215 (40) |
| Abdomen | 84 (16) |
| Spine | 176 (33) |
| Extremities | 325 (60) |
| External and other | 73 (14) |
| AIS-scores 3–5, n (%)a | |
| Head | 223 (41) |
| Face | 14 (3) |
| Neck | 10 (2) |
| Thorax | 185 (34) |
| Abdomen | 58 (11) |
| Spine | 74 (14) |
| Extremity | 95 (18) |
| External and other | 2 (0.4) |
| Spinal cord injury, n (%) | 39 (7) |
| aParticipants may have injuries in more than one body region. | |
| ASA: American Society of Anaesthesiologists Physical Status Classification System. | |
Physician assessment
Out of the 194 participants staying in the ICU in the trauma centre for 3 or more days, 35 (18%) had an assessment within 3 days after admission to the ICU by a physical medicine and rehabilitation physician registered in the medical record. Of the patients seen by a specialist, 34 (97%) had severe or profound injuries (NISS > 15), 31 (89%) had severe head injuries (AIS 3–5), 12 (34%) had severe thorax injuries (AIS 3–5), and 4 (11%) severe extremities injuries. Severe injuries in other organ areas were less frequent.
Therapist intervention in the intensive care unit
Of all participants with at least 2 days length of stay in the ICU (n = 262), 70% received therapist intervention. The rate was 84% for participants who stayed for at least 3 days. For participants with NISS > 15 and at least 2 days of stay in the ICU (n = 169), the proportion who received therapist intervention was 72% (Table IV). Median for first day of treatment was 3 days (range 1–12). A physiotherapist was the first active therapist for 88%; this was a social worker for 12% of participants. Multidisciplinary therapist intervention was provided to 31% of the participants with NISS > 15 and at least 2 days of stay in the ICU.
| N 235 (100%) | Therapist treatment ICU 169 (72%) | No therapist treatment ICU 66 (28%) | Univariate | Multivariable | |||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Demographics | |||||||||
| Age, years, median (range) | 56 (18–91) | 56 (18–91) | 55 (20–88) | 1.0 | 0.99–1.01 | 0.814 | 1.0 | 0.98–1.03 | 0.952 |
| Sex, female, n (%) | 55 (23) | 44 (77) | 11 (23) | ||||||
| Male, n (%) | 180 (77) | 125 (69) | 55 (31) | 1.76 | 0.85–3.66 | 0.131 | 1.85 | 0.73–4.69 | 0.193 |
| Education, low, n (%)a | 142 (60) | 108(76) | 34 (24) | ||||||
| Education, high, n (%) | 83 (35) | 55 (66) | 28 (34) | 0.62 | 0.34–1.12 | 0.114 | .57 | 0.25–1.28 | 0.175 |
| Living alone, n (%)2 | 88 (37) | 60 (68) | 28 (32) | ||||||
| Not living alone, n (%) | 147 (62) | 109 (74) | 38 (26) | 1.34 | 0.75–2.39 | 0.325 | 1.37 | 0.60–3.16 | 0.455 |
| Not working, n (%)a | 112 (48) | 83 (74) | 29 (26) | ||||||
| Working, n (%) | 119 (51) | 83 (70) | 36 (30) | 0.81 | 0.45–1.43 | 0.462 | 1.01 | 0.41–2.55 | 0.972 |
| Acute injury-related variables | |||||||||
| Per-injury ASA, (1–2), n (%) | 202 (86) | 142 (70) | 60 (30) | ||||||
| Pre-injury ASA, (3–4), n (%) | 33 (14) | 27 (82) | 6 (18) | 1.90 | 0.75–4.84 | 0.178 | 1.61 | 0.49–5.32 | 0.433 |
| Substance use at time of injury, n (%) | 55 (23) | 35 (63) | 20 (37) | ||||||
| No substance use, n (%) | 180 (77) | 134 (74) | 46 (26) | 0.60 | 0.32–1.14 | 0.121 | 0.484 | 0.18–1.32 | 0.155 |
| NISS, median (range) | 27 (16–75) | 33 (16–75) | 27 (16–57) | 1.04 | 1.02–1.07 | 0.002 | 1.01 | 0.97–1.06 | 0.523 |
| Length of stay ICU, median (range) | 6 (2–50) | 7 (2–50) | 2 (2–26) | 1.33 | 1.19–1.48 | < 0.001 | 1.25 | 1.12–1.41 | < 0.001 |
| Head AIS 0–2, n (%) | 105 (45) | 76 (72) | 29 (28) | ||||||
| Head AIS 3–5, n (%) | 130 (55) | 93 (72) | 37 (28) | 0.95 | 0.54–1.70 | 0.886 | 1.33 | 0.47–3.79 | 0.592 |
| Face AIS 0–2, n (%) | 226 (96) | 161 (71) | 65 (29) | ||||||
| Face AIS 3–5, n (%) | 9 (4) | 8 (89) | 1 (11) | 3.23 | 0.40–26.34 | 0.274 | 3.13 | 0.27–37.13 | 0.365 |
| Neck AIS 0–2, n (%) | 228 (97) | 164 (72) | 64 (28) | ||||||
| Neck AIS 3–5, n (%) | 7 (3) | 5 (71) | 2 (29) | 0.98 | 0.19–5.16 | 0.977 | 0.542 | 0.05–5.57 | 0.606 |
| Thorax AIS 0–2, n (%) | 134 (57) | 91 (69) | 43 (31) | ||||||
| Thorax AIS 3–5, n (%) | 101 (43) | 78 (68) | 23 (22) | 1.60 | 0.89–2.89 | 0.117 | 1.80 | 0.80–4.02 | 0.153 |
| Abdomen AIS 0–2, n (%) | 209 (89) | 151 (72) | 58 (28) | ||||||
| Abdomen AIS 3–5, n (%) | 26 (11) | 18 (69) | 8 (31) | 0.86 | 0.36–2.10 | 0.747 | 0.85 | 0.24–2.97 | 0.80 |
| Spine without spinal cord AIS 0–2, n (%) | 219 (93) | 157 (72) | 62 (28) | ||||||
| Spine without spinal cord AIS 3–5, n (%) | 16 (7) | 12 (75) | 4 (25) | 1.19 | 0.37–3.81 | 0.776 | 2.08 | 0.51–8.50 | 0.308 |
| Extremity AIS 0–2, n (%) | 187 (80) | 131(70) | 56 (30) | ||||||
| Extremity AIS 3–5, n (%) | 48 (20) | 38 (79) | 10 (21) | 1.62 | 0.76–3.49 | 0.213 | 1.42 | 0.46–4.37 | 0.541 |
| No Spinal cord injury | 205 (87) | 139 (68) | 66 (32) | ||||||
| Spinal cord injury, n (%) | 30 (13) | 30 (100) | 0 (0) | 0.001b | |||||
| aThree demographic variables (education, work and living situation) had missing data, with education the highest proportion (4%). | |||||||||
| bFisher’s exact test. | |||||||||
| Results in bold fond are statistically significant. | |||||||||
| ICU: intensive care unit, OR: odds ratio; 95% CI: 95% confidence interval; ASA: American Society of Anaesthesiologists Physical Status Classification System; NISS: New Injury Severity Scale; AIS: Abbreviated Injury Scale. | |||||||||
Univariate and multivariable regression analysis of predictors for therapist intervention in the ICU are shown in Table IV. Only longer length of ICU stay was a significant predictor in multivariable analysis (OR 1.25, 95% CI 1.12–1.41), having a spinal cord injury could not be included in these analyses because of single-sided distribution (Table IV). All patients who had spinal cord injury received rehabilitation within 2 days of ICU stay. Nagelkerke R2 showed with 0.46 satisfying explanation of the variance in the model. Hosmer and Lemeshow goodness-of-fit test showed a good fitting model (p = 0.076).
Direct transfer from acute ward to specialized rehabilitation
Discharge destinations were specialized rehabilitation (22% of 538 participants), local hospitals (42%), and home (33%) (Table III). The proportion of participants transferred directly to rehabilitation was highest for patients with spinal cord injury (54%) and severe head injury (39% for AIS 3–5 and 48% for AIS 4–5). Of the participants transferred directly, 91% had severe or profound injuries (NISS > 15). Of these 411 participants with NISS > 15, 106 (26%) were transferred directly to rehabilitation (Table V). Multivariate logistic regression showed working status (OR 2.75, 95% CI 1.32–5.74), severe head injury (AIS 3–5) (OR 3.78, 95% CI 1.53–9.31), spinal cord injury (OR 6.8, 95% CI 2.35–19.67) and length of stay in the ICU (OR 1.1, 95% CI 1.04–1.15) to be significant predictors of direct discharge from acute trauma care to a specialized rehabilitation unit. Nagelkerke R2 (at 0.43) showed satisfying explanation of the variance in the model. Hosmer and Lemeshow goodness-of-fit test showed a good fitting model (p = 0.725).
| N n=411 (100%) | Direct transfer n=106 (26%) | Not direct n=305 (74%) | Univariate | Multivariable | |||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||||
| Demographics | |||||||||
| Age, years, median (range) | 411 | 51 (18–79) | 55 (18–93) | 0.99 | 0.97–1.0 | 0.094 | 1.0 | 0.98–1.02 | 0.885 |
| Sex, female, n (%) | 96 | 20 (21) | 76 (79) | ||||||
| Male, n (%) | 315 | 86 (27) | 229 (73) | 0.70 | 0.40–1.22 | 0.206 | 0.61 | 0.29–1.28 | 0.19 |
| Education, low, n (%)a | 233 | 61 (26) | 172 (74) | ||||||
| Education, high, n (%) | 161 | 43 (27) | 118 (73) | 1.03 | 0.65–1.62 | 0.907 | 0.84 | 0.45–1.56 | 0.58 |
| Living alone, n (%)a | 159 | 41 (26) | 118 (74) | ||||||
| Not living alone, n (%) | 251 | 65 (26) | 186 (74) | 1.00 | 0.64–1.58 | 0.98 | 0.66 | 0.35–1.24 | 0.198 |
| Not working, n (%)a | 174 | 31 (18) | 143 (82) | ||||||
| Working, n (%) | 230 | 73 (32) | 157 (68) | 2.15 | 1.33–3.46 | 0.002 | 2.75 | 1.32–5.74 | 0.007 |
| Acute injury-related variables | |||||||||
| Per-injury ASA, (1–2), n (%) | 361 | 98 (27) | 263 (73) | ||||||
| Pre-injury ASA, (3–4), n (%) | 50 | 8 (16) | 42 (84) | 0.51 | 0.232–1.13 | 0.096 | 0.47 | 0.17–1.30 | 0.146 |
| Substance use at time of injury, n (%) | 100 | 33 (33) | 67 (67) | ||||||
| No substance use, n (%) | 311 | 73 (23) | 238 (77) | 1.61 | 0.98–2.63 | 0.059 | 1.01 | 0.52–1.94 | 0.982 |
| NISS, median (range) | 411 | 34 (16–75) | 24 (16–66) | 1.05 | 1.03–1.07 | < 0.001 | 1.02 | 0.99–1.05 | 0.195 |
| Length of stay ICU, median (range) | 411 | 7 (1–39) | 2 (0–50) | 1.10 | 1.07–1.14 | < 0.001 | 1.10 | 1.04–1.15 | < 0.001 |
| Head AIS 0–2, n (%) | 203 | 24 (12) | 179 (88) | ||||||
| Head AIS 3–5, n (%) | 208 | 82 (39) | 126 (61) | 4.85 | 2.92–8.07 | < 0.001 | 3.78 | 1.53–9.31 | 0.004 |
| Face AIS 0–2, n (%) | 399 | 103 (26) | 296 (74) | ||||||
| Face AIS 3–5, n (%) | 12 | 3 (25) | 9 (75) | 0.96 | 0.25–3.61 | 0.949 | 0.35 | 0.07–1.79 | 0.207 |
| Neck AIS 0–2, n (%) | 403 | 102 (25) | 301 (75) | ||||||
| Neck AIS 3–5, n (%) | 8 | 4 (50) | 4 (50) | 2.95 | 0.73–12.02 | 0.131 | 4.48 | 0.4–49.72 | 0.222 |
| Thorax AIS 0–2, n (%) | 239 | 80 (32) | 159 (68) | ||||||
| Thorax AIS 3–5, n (%) | 172 | 26 (15) | 146 (85) | 0.354 | 0.22–0.58 | < 0.001 | 0.55 | 0.275–1.12 | 0.098 |
| Abdomen AIS 0–2, n (%) | 360 | 101 (28) | 259 (72) | ||||||
| Abdomen AIS 3–5, n (%) | 51 | 5 (10) | 46 (90) | 0.279 | 0.11–0.72 | 0.008 | 0.47 | 0.14–1.56 | 0.218 |
| Spine without spinal cord AIS 0–2, n (%) | 388 | 104 (27) | 284 (73) | ||||||
| Spine without spinal cord AIS 3–5, n (%) | 23 | 2 (9) | 21 (91) | 0.26 | 0.06–1.13 | 0.072 | 0.13 | 0.15–1.19 | 0.082 |
| Extremity AIS 0–2, n (%) | 337 | 96 (28) | 241 (72) | ||||||
| Extremity AIS 3–5, n (%) | 74 | 10 (14) | 64 (86) | 0.39 | 0.19–0.80 | 0.009 | 0.42 | 0.15–1.19 | 0.102 |
| No spinal cord injury | 377 | 87 (23) | 290 (77) | ||||||
| Spinal cord injury | 34 | 19 (56) | 15 (44) | 4.22 | 2.06–8.66 | < 0.001 | 6.8 | 2.35–19.67 | < 0.001 |
| aThree demographic variables (education, work and living situation) had missing data, with education the highest proportion (4%). | |||||||||
| Results in bold fond are statistically significant. | |||||||||
| ICU: intensive care unit; OR: odds ratio; 95% CI: 95% confidence interval; ASA: American Society of Anaesthesiologists Physical Status Classification System; NISS: New Injury Severity Scale; AIS: Abbreviated Injury Scale. | |||||||||
DISCUSSION
This study investigated adherence to 3 central operational recommendations for acute rehabilitation in the Norwegian national trauma plan. Of patients who stayed 3 or more days in the ICU, assessment by a physical medicine and rehabilitation physician within 72 h after admission was documented in 18% of patients. Therapist treatment in the ICU was given to 70% of the 262 participants with an ICU stay of 2 days or longer. Of all participants, 22% were transferred directly from acute ward in the trauma centre to a specialized rehabilitation unit. With a high proportion of participants with severe trauma (76%) and 88% of patients with ICU treatment, the population in this study has more severe injuries than in the retrospective embedded rehabilitation studies of Scott et al. (13) after major trauma and the study of Wu et al. (17) after road trauma, but less severe injuries than in the multiple trauma studies of Bouman et al. (16).
Except from the UK National Clinical Audit for Specialist Rehabilitation following major Injury (NCASRI 2019) (33), to our knowledge, this is one of the first studies to evaluate adherence to operational recommendations for acute rehabilitation in trauma guidelines for a general trauma population.
The Norwegian Trauma Plan recommends assessment by a physical medicine and rehabilitation physician within 72 h after admission to the ICU in the trauma centre, and early onset of rehabilitation in the ICU. Furthermore, they recommend that patients needing inpatient rehabilitation to be directly transferred from acute departments in the trauma centre to a specialized rehabilitation unit. National institute for Health and Care Excellence (NICE) guidelines for rehabilitation after traumatic injury (34) give similar, detailed, but less precise, recommendations for assessment and start of rehabilitation. The American College of Surgeons has integrated recommendations for rehabilitation into their best practice guidelines for orthopaedic trauma and spine injury (35, 36), but not for traumatic brain injury (37). The orthopaedic guidelines emphasize early assessment and integration of rehabilitation in acute care; the recommendations for spine injuries specify onset of therapy within the first week after admission, and discharge to a specialized inpatient rehabilitation facility.
Physician assessment
Several authors recommend assessment by a physical medicine and rehabilitation physician in the first days after ICU admission as part of a structured rehabilitation programme after traumatic brain injury (24), multiple trauma (16) or major trauma (13). Time for the specialist visit varies from 2 days after hospital admission (16) to within 72 h (24), to 2–4 days (13), comparable to the Norwegian guidelines, which recommend specialist assessment within 72 h. An integrated multidisciplinary approach is often recommended (13, 24). The NCASRI 2019 found that 54% of patients were assessed within 10 days according to NICE guidelines, compared with 18% in the current study assessed within 3 days. In the same study only 40% of the patients who were identified as requiring further specialist inpatient rehabilitation actually received it (33). In the study by Wu et al. (17) use of consulting interdisciplinary teams, after patient transfer from the ICU and to an acute ward, did not change length of stay in acute care. A continuous chain in treatment from acute rehabilitative care to specialized inpatient rehabilitation is important for short- and long-term recovery (16, 20). Systematic early specialist assessment of rehabilitation needs is a way to secure an effective treatment process, and the low degree of recorded assessments found in the current study raises concern that rehabilitation needs may not be recognized or documented. The optimum time to start is not clearly defined (23) and must be somewhat pragmatic. However, routines must ensure identification of all patients needing intervention, which should start without delay. Overall, a recommendation for assessment by a physical medicine and rehabilitation physician within 72 h after admission to trauma centre ICU is supported by the literature and clinical experience.
Therapist intervention in the intensive care unit
Activation and mobilization should start when patients are stabilized, but is often delayed (38). Injury-specific limitations for early mobilization, such as specific fractures, severe internal bleeding and neurotrauma may limit activation and mobilization in the subacute phase (39), making the ideal time to start activity unclear. The 70% of participants receiving therapy from at least 1 professional in addition to physicians and nurses in the ICU is higher than reported by Nickels et al. (38) (57%) in a general ICU population and by Bartolo et al. (40) (65%) in a population with all types of brain injury. The median time of 3 days until first treatment found in the current study is, however, later than observed in other studies (38, 41, 42). Nearly all critical care patients benefit from rehabilitation (41, 42) and hyperacute specialized rehabilitation services are shown to be cost-effective (25). OUH has a programme for early interdisciplinary rehabilitation integrated into acute care for patients with severe TBI in the Early Rehabilitation Section of the Neuro ICU (20), but there is no corresponding organized early rehabilitation service for other trauma patients, except for those with spinal cord injury. In the current study patients with spinal cord injury were treated by a therapist more often than patients with other trauma types. Multidisciplinary therapist intervention to 31% of the participants with severe injuries and at least 2 days of stay in the ICU, is a low rate considering the complex functional and psychosocial challenges faced by patients with severe injuries.
Direct transfer from acute ward to specialized rehabilitation
Debus et al. (18), using comparable inclusion criteria as in the current study, found a somewhat higher direct transfer rate of 32%, compared with 22% in the current study. In comparison, Dinh et al. (43) found a direct transfer rate to specialized rehabilitation of 4% in a population with lower injury severity (median Injury Severity Score (ISS) 4). However, Dijkink et al. (44) found a significant disparity in transfer rates (47% vs 10%) between an American and a Dutch trauma centre in populations that were similar. This is probably caused by different organization of the treatment chain.
Evidence from several studies (7, 21, 22) shows that direct transfer to specialized rehabilitation is positive for the outcome of patients with severe brain injury. In the current study population, the direct transfer rate for participants with severe head injury was 39%, which is comparable to earlier Norwegian studies (7, 21), taking into consideration that the proportion of patients with AIS 4–5 is lower in the current study. Shorter hospital stay and more rapid gain of function is shown for patients with severe orthopaedic injuries who are transferred directly from acute ward to rehabilitation (14, 16). In contrast to the current study, both Debus et al. (18) and Dinh et al. (43) found extremity injuries to be a predictor for direct transfer to rehabilitation. In the current study only 13% of the participants with severe injuries to the extremities (AIS 3–5) were transferred directly to inpatient rehabilitation. Even taking into account that injury severity does not necessarily correspond to rehabilitation needs, the overall percentage of participants transferred directly, especially among orthopaedic patients, is low.
Patients with moderate injuries less frequently received treatment according to the guidelines than did patients with more severe injuries. For instance, the proportion with direct transfer to rehabilitation was 9% among those with moderate injuries (NISS 10–15) and 26% among those with severe injuries (NISS > 15). Moderately injured patients may experience significant loss of function; therefore, this group probably has unmet needs for rehabilitation.
Study strengths and limitations
The prospective design of the study is a strength. A relatively low rate of 17% of the eligible adults were non-responders or declined participation. However, the study found that adults with psycho-social and/or drug problems more often left the hospital early against medical advice or were more often non-responders. Therefore, this group may be underrepresented in the study material.
Unrecorded informal assessments led to some understatement of the percentage of patients assessed by a physical medicine and rehabilitation physician. In addition, patients with SCI are routinely referred to rehabilitation by attending traumatologists or health professionals from the regional SCI rehabilitation unit. They are often directly transferred to specialized rehabilitation and, less frequently, after preceding assessment by a physical and rehabilitation medicine physician. A low rate may also be due to limited resources. The current study has few missing data, providing a good basis for analysis.
CONCLUSION
Early therapist intervention in the ICU is provided to more than two-thirds of the patients with severe trauma. Initiation of treatment is somewhat later than in other studies. Otherwise, compliance with the guidelines is poor. This applies especially to assessments by a physical medicine and rehabilitation physician within 72 h after admission registered in medical records. Furthermore, the overall proportion of participants transferred directly to specialized in-patient rehabilitation is low. Direct transfer is common after spinal cord injury, less common after severe head injury, and patients with severe extremity injuries are rarely given priority. Findings indicate a need for more systematic integration of rehabilitation in the acute treatment phase after trauma.
ACKNOWLEDGEMENTS
The authors thank all the patients and caregivers who participated in this study, Tone Fjeld Hansen, Ruhina Biswas, Maria Solvang and Arne Gya for substantial contributions in patient recruitment and data collection, Lilian Fricke and the Department of Traumatology, OUH, for their help with identifying the patients, Hege Margrethe Lauritzen and the OUH and UNN trauma registries and Marianne Dahlhaug at the Norwegian Trauma Registry for their help with assigning and validating the trauma scores, and the user panel and the Norwegian Association for the Injured for help with the design of the study.
REFERENCES
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204–1222. DOI: 10.1016/S0140-6736(20)30925-9.
- Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 2016; 22: 3–18. DOI: 10.1136/injuryprev-2015-041616.
- Anke AG, Stanghelle JK, Finset A, Roaldsen KS, Pillgram-Larsen J, Fugl-Meyer AR. Long-term prevalence of impairments and disabilities after multiple trauma. J Trauma 1997; 42: 54–61. DOI: 10.1097/00005373-199701000-00010.
- Soberg HL, Finset A, Bautz-Holter E, Sandvik L, Roise O. Return to work after severe multiple injuries: a multidimensional approach on status 1 and 2 years postinjury. J Trauma 2007; 62: 471–481. DOI: 10.1097/TA.0b013e31802e95f4.
- Kaske S, Lefering R, Trentzsch H, Driessen A, Bouillon B, Maegele M, et al. Quality of life two years after severe trauma: a single-centre evaluation. Injury 2014; 45: S100–105. DOI: 10.1016/j.injury.2014.08.028.
- Kamenov K, Mills JA, Chatterji S, Cieza A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil 2019; 41: 1227–1237. DOI: 10.1080/09638288.2017.1422036.
- Sveen U, Roe C, Sigurdardottir S, Skandsen T, Andelic N, Manskow U, et al. Rehabilitation pathways and functional independence one year after severe traumatic brain injury. Eur J Phys Rehabil Med 2016; 52: 650–661.
- Al Hanna R, Amatya B, Lizama LE, Galea MP, Khan F. Multidisciplinary rehabilitation in persons with multiple trauma: a systematic review. J Rehabil Med 2020; 52: jrm00108. DOI: 10.2340/16501977-2737.
- Miclau T, Hoogervorst P, Shearer DW, El Naga AN, Working ZM, Martin C, et al. Current status of musculoskeletal trauma care systems worldwide. J Orthop Trauma 2018; 32: S64–S70. DOI: 10.1097/BOT.0000000000001301.
- Mock C LJ, Goosen J, Joshipura M, Peden M. Guidelines for essential traumacare. Geneva: World Health Organization; 2004: 45–48.
- Lidal IB, Snekkevik H, Aamodt G, Hjeltnes N, Biering-Sorensen F, Stanghelle JK. Mortality after spinal cord injury in Norway. J Rehabil Med 2007; 39: 145–151. DOI: 10.2340/16501977-0017.
- Savic G, DeVivo MJ, Frankel HL, Jamous MA, Soni BM, Charlifue S. Long-term survival after traumatic spinal cord injury: a 70-year British study. Spinal Cord 2017; 55: 651–658. DOI: 10.1038/sc.2017.23.
- Scott J, Kandala NB, Fearon P, Robinson L. Embedded rehabilitation in major trauma: Retrospective pre-post observational study of service and patient outcomes. Injury 2021; 52: 160–166. DOI: 10.1016/j.injury.2020.11.009.
- Khan F, Amatya B, Hoffman K. Systematic review of multidisciplinary rehabilitation in patients with multiple trauma. Br J Surg 2012; 99 Suppl 1: 88–96. DOI: 10.1002/bjs.7776.
- Kreitzer N, Rath K, Kurowski BG, Bakas T, Hart K, Lindsell CJ, et al. Rehabilitation practices in patients with moderate and severe traumatic brain injury. J Head Trauma Rehabil 2019; 34: E66–E72. DOI: 10.1097/HTR.0000000000000477.
- Bouman AI, Hemmen B, Evers SM, van de Meent H, Ambergen T, Vos PE, et al. Effects of an integrated ‘fast track’ rehabilitation service for multi-trauma patients: a non-randomized clinical trial in the Netherlands. PLoS One 2017; 12: e0170047. DOI: 10.1371/journal.pone.0170047.
- Wu J, Faux SG, Estell J, Wilson S, Harris I, Poulos CJ, et al. Early rehabilitation after hospital admission for road trauma using an in-reach multidisciplinary team: a randomised controlled trial. Clin Rehabil 2017; 31: 1189–1200. DOI: 10.1177/0269215517694462.
- Debus F, Lefering R, Lang N, Oberkircher L, Bockmann B, Ruchholtz S, et al. Which factors influence the need for inpatient rehabilitation after severe trauma? Injury 2016; 47: 2683–2687. DOI: 10.1016/j.injury.2016.06.035.
- Bartolo M, Bargellesi S, Castioni CA, Intiso D, Fontana A, Copetti M, et al. Mobilization in early rehabilitation in intensive care unit patients with severe acquired brain injury: an observational study. J Rehabil Med 2017; 49: 715–722. DOI: 10.2340/16501977-2269.
- Andelic N, Bautz-Holter E, Ronning P, Olafsen K, Sigurdardottir S, Schanke AK, et al. Does an early onset and continuous chain of rehabilitation improve the long-term functional outcome of patients with severe traumatic brain injury? J Neurotrauma 2012; 29: 66–74. DOI: 10.1089/neu.2011.1811.
- Anke A, Andelic N, Skandsen T, Knoph R, Ader T, Manskow U, et al. Functional Recovery and life satisfaction in the first year after severe traumatic brain injury: a prospective multicenter study of a Norwegian national cohort. J Head Trauma Rehabil 2015; 30: E38–49. DOI: 10.1097/HTR.0000000000000080.
- Godbolt AK, Stenberg M, Lindgren M, Ulfarsson T, Lannsjo M, Stalnacke BM, et al. Associations between care pathways and outcome 1 year after severe traumatic brain injury. J Head Trauma Rehabil 2015; 30: E41–51. DOI: 10.1097/HTR.0000000000000050.
- Naess HL, Vikane E, Wehling EI, Skouen JS, Bell RF, Johnsen LG. Effect of early interdisciplinary rehabilitation for trauma patients: a systematic review. Arch Rehabil Res Clin Transl 2020; 2: 100070. DOI: 10.1016/j.arrct.2020.100070.
- Lui SK, Ng YS, Nalanga AJ, Tan YL, Bok CW. A pilot project of early integrated traumatic brain injury rehabilitation in Singapore. Rehabil Res Pract 2014; 2014: 950183. DOI: 10.1155/2014/950183.
- Turner-Stokes L, Bavikatte G, Williams H, Bill A, Sephton K. Cost-efficiency of specialist hyperacute in-patient rehabilitation services for medically unstable patients with complex rehabilitation needs: a prospective cohort analysis. BMJ Open 2016; 6: e012112. DOI: 10.1136/bmjopen-2016-012112.
- Wisborg T, Gaarder C, Geisner T, Rolandsen BA. Ny nasjonal Traumeplan [New national trauma care plan]. Tidsskr Nor Laegeforen 2017; 137. DOI: 10.4045/tidsskr.17.0792.
- Soberg HL, Moksnes HO, Anke A, Roise O, Roe C, Aas E, et al. Rehabilitation needs, service provision, and costs in the first year following traumatic injuries: protocol for a prospective cohort study. JMIR Res Protoc 2021; 10: e25980. DOI: 10.2196/25980.
- The Abbreviated Injury Scale (AIS) 2005, Update 2008. 2008 [cited 2022 December 14]; Available from: https://www.aaam.org/abbreviated-injury-scale-ais/
- Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma 1997; 43: 922–925; discussion 925–926. DOI: 10.1097/00005373-199712000-00009.
- Palmer CS, Gabbe BJ, Cameron PA. Defining major trauma using the 2008 Abbreviated Injury Scale. Injury 2016; 47: 109–115. DOI: 10.1016/j.injury.2015.07.003.
- Nasjonalt traumeregister. Definisjonskatalog for Nasjonalt Traumeregister. In: Olav Roise MD, Peder Hoem, editor. 2019 14.09.22. Oslo: Oslo Universitetssykehus HF; 2019, p. 32–33.
- Economics ACo. ASA Physical Status Classification System. 2014 [cited 2022 19.09.]; Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
- NCASRI Project team LT-SL. Final report of the National Clinical Audit of Specialist Rehabilitation following major Injury: NHS-London North West University Healthcare; 2019.
- Rehabilitation after traumatic injury (NICE guideline [NG211]). 2022 [cited 2022 December 14]; Available from: https://www.nice.org.uk/guidance/ng211
- Best Practices in the Management of Orthopedic Trauma. acs tqip – Trauma Quality Improvement Program 2015 [cited 2022 December 14]; Available from: https://www.facs.org/media/mkbnhqtw/ortho_guidelines.pdf
- Trauma Co. Best practice guidelines – spine injury. Trauma Quality Programs 2022 [cited 2022 December 14]. Available from: https://www.facs.org/media/k45gikqv/spine_injury_guidelines.pdf
- Best practices in the management of traumtic brain injury. ACS TQIP 2015 [cited 2022 December 14]. Available from: https://www.facs.org/media/mkej5u3b/tbi_guidelines.pdf
- Nickels MR, Aitken LM, Walsham J, Crampton LJ, Barnett AG, McPhail SM. Exercise interventions are delayed in critically ill patients: a cohort study in an Australian tertiary intensive care unit. Physiotherapy 2020; 109: 75–84. DOI: 10.1016/j.physio.2019.06.011.
- Engels PT, Beckett AN, Rubenfeld GD, Kreder H, Finkelstein JA, da Costa L, et al. Physical rehabilitation of the critically ill trauma patient in the ICU. Crit Care Med 2013; 41: 1790–1801. DOI: 10.1097/CCM.0b013e31828a2abf.
- Bartolo M, Bargellesi S, Castioni CA, Bonaiuti D, Intensive Care and Neurorehabilitation Italian Study Group Early rehabilitation for severe acquired brain injury in intensive care unit: multicenter observational study. Eur J Phys Rehabil Med 2016; 52: 90–100.
- Falkenstein BA, Skalkowski CK, Lodise KD, Moore M, Olkowski BF, Rojavin Y. The Economic and clinical impact of an early mobility program in the trauma intensive care unit: a quality improvement project. J Trauma Nurs 2020; 27: 29–36. DOI: 10.1097/JTN.0000000000000479.
- Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009; 373: 1874–1882. DOI: 10.1016/S0140-6736(09)60658-9.
- Dinh M, Bein KJ, Byrne C, Nair I, Petchell J, Gabbe B, et al. Predictors of transfer to rehabilitation for trauma patients admitted to a level 1 trauma centre – a model derivation and internal validation study. Injury 2013; 44: 1551–1555. DOI: 10.1016/j.injury.2013.04.005.
- Dijkink S, van der Wilden GM, Krijnen P, Dol L, Rhemrev S, King DR, et al. Polytrauma patients in the Netherlands and the USA: a bi-institutional comparison of processes and outcomes of care. Injury 2018; 49: 104–109. DOI: 10.1016/j.injury.2017.10.021.