ABSTRACT
Background: One of the important goals in the treatment of spastic cerebral palsy is to maintain efficient and effective walking in order to be independent in activities and participate in society.
Objective: To compare the efficacy of foot combination taping of kinesio tape and athletic tape vs ankle foot orthosis in correcting spatiotemporal gait parameters in children with spastic diplegia.
Methods: Thirty-six children with spastic diplegia were randomly assigned into 3 groups; control, combination taping, and ankle foot orthosis groups. Children in the control group, in addition to those in both experimental groups, continued with conventional physical therapy, 1 h, 3 times per week for 4 weeks. Spatiotemporal gait parameters were assessed with the GAITRite system before and after the application of interventions.
Results: There were significant increases in walking velocity, step length, stride length, right single
support duration, and left single support duration of the ankle foot orthosis and combination taping groups compared with pre-intervention values. Moreover, the post-intervention values of the double support duration of the ankle foot orthosis and combination taping groups were significantly lower than pre-intervention values. There were no significant differences between the post-intervention values of the ankle foot orthosis and combination taping groups for all parameters.
Conclusion: The results demonstrated that combination taping is an effective alternative technique to ankle foot orthosis to improve spatiotemporal parameters in children with spastic diplegic in combination with conventional physiotherapy.
Key words: combination taping; ankle foot orthosis; gait parameters; cerebral palsy.
Accepted Nov 9, 2021; Epub ahead of print Nov 23, 2021
J Rehabil Med 2021; 53: jrm00240
Correspondence address: Mohamed A. Abdel Ghafar, Physical Therapy Program, Batterjee Medical College, Jeddah, Saudi Arabia. E-mail: pt12.jed@bmc.edu.sa
LAY ABSTRACT
Children with cerebral palsy have abnormal patterns of walking secondary to spasticity, which can negatively affect their functional abilities and quality of life. Several therapeutic interventions are used, with the aim of improving gait quality in those children so that they become independent in functional activities and can participate in society. This study compared the effectiveness of ankle bracing with the application of a combination taping on gait parameters. The results showed that both interventions are equally effective. Combination taping might be considered a promising alterative to ankle joint bracing, as it is a more functional and less aggressive technique.
INTRUDUCTION
Cerebral palsy (CP) is a lifelong motor impairment caused by an early brain injury. Depending on the dominant neurological signs of children with CP, the condition is classified as spastic, ataxic, athetoid, or flaccid (1). More than 70% of children with CP are spastic (2). Gait in children with spastic CP is frequently associated with abnormal gait kinematics, linked to increased walking energy cost, which may lead to activity limitations (3).
Plantar flexion in the ankle at the beginning of standing and in all phases of walking is one1 of the most common dynamic musculoskeletal deformities in children with spastic CP, which could be accompanied by additional abnormal joint positions of the lower extremities (4). The ability to maintain proper joint alignment of the lower extremity, and monitor the position of the foot while standing and walking, are critical prerequisites for gait in children with CP (5).
Lower extremity orthosis, such as ankle foot orthosis (AFO) is widely recommended in children with spastic CP to prevent the progression of the deformity and to improve the child’s gait efficiency (6). The solid AFO maximizes control by restricting both plantarflexion and dorsiflexion movements in the stance and swing phases. Its rigid structure prevents ankle rocker function and reduces excessive plantarflexion during the stance phase, thus facilitating clearance of the toes during the swing phase (7). The benefits of wearing an AFO on gait parameters in children with spastic CP have already been documented in the literature (8).
Athletic and Kinesio tapes are the 2 most common types of tape used in clinical settings. Both can be used on patients with orthopaedic or neurological dysfunctions. Athletic tape is a rigid/inelastic tape that restricts movement, while Kinesio tape is a form of flexible/elastic tape. Researchers have used them for similar purposes, such as spasticity control, muscle function facilitation, and joint stabilization (9). Furthermore, studies suggest that rigid tape is more effective than elastic tape at controlling joint mobility (10).
The use of Kinesio taping in paediatric rehabilitation has become increasingly popular in recent years. Recent systematic reviews reported moderate evidence that Kinesiology taping is a valuable complement to physiotherapy treatment in better-performing children with CP (11, 12). Combination taping is a technique first introduced by Kenzo et al. (13), in which Kinesio tape is combined with rigid athletic tape to maximize the treatment benefits. This approach remains briefly addressed in the literature with no prior studies has examined the effects of combination tapings of Kinesio tape and athletic tape in the CP paediatric population. Hence, this study was conducted to compare the effectiveness of foot combined taping vs AFO in correcting spatiotemporal gait parameters in spastic CP children with equinus deformity.
METHODS
Study design
This study was a single-blinded, randomized controlled trial. It was blinded to the assessor of the outcomes and was conducted from the period December 2020 to March 2021. The participants and their parents were given a clear, detailed explanation of the proposed procedures before starting the experiment, and a written informed consent statement was signed. The study was carried out in compliance with the 1975 Declaration of Helsinki, and approved by Batterjee Medical College Research and Ethics Committee (RES-2021-0022), and was registered by clinical registration trial (NCT04839939).
Participants
A total of 46 children with spastic diplegic CP recruited from local paediatric rehabilitation centres were screened for eligibility and 7 children were excluded for not meeting the inclusion criteria. A total of 39 children were enrolled in this study, out of which 36 (21 boys and 15 girls) completed the follow-up assessment, as shown in Fig. 1.

Inclusion criteria were: age range 8–15 years; able to stand and walk independently; have hypertonia ranging from 1 to 1+ according to the Modified Ashworth Scale (MAS); have a minimum 5° of passive ankle dorsiflexion with knees extended; level I or II on the Gross Motor Function Classification System (GMFCS); capable of understanding and following instructions. Children with previous corrective orthopaedic surgery, botulinum toxin injections in the lower extremities within the previous 6 months, skin disease, epilepsy, mental retardation, and visual or auditory problems were excluded. Table I shows the participants’ characteristics.

The children were allocated randomly into 3 groups; control, AFO, and combination taping groups. Randomization was done using specific software (random allocation software 1.0, 2011) into 3 equal groups. G*Power (Universities, Dusseldorf, Germany) software was used to calculate the sample size of the outcome parameter walking velocity, with an alpha of 0.05, power of 80%, and an effect size of 0.48. The sample size was ٣٦ children.
Procedures
The AFO group was provided with solid community-prescribed AFO (Fig. 2) with a wearing schedule of 6–12 h per day. Parents were given a detailed demonstration about how to use the AFO probably and watching for areas of skin overpressure. AFO must be worn with a smooth, long sock underneath with the child’s heel is fully encased in the AFO with the ankle strap and/or shoe fastened tightly.
The combination tapings group received the combination tapings technique, which was conducted by a qualified physical therapist with over 4 years of experience. Skin sensitivity was first tested before the tape application process. The technique started with the application of 2 5-cm wide Kinesio tape “I” straps (Kinesiology tape I-strip roll, Mueller Sports Medicine, USA). The first strap was applied from the lateral condyle of the tibia to the base of the first metatarsal bone with the ankle joint in plantar flexion to facilitate the action of the tibialis anterior (Fig. 3A). The tape was not stretched for the first 5 cm before being stretched up to 30% for the remaining parts (13). Functional correction was the aim of the application of the second “I” strap to assist ankle dorsiflexion and restrict plantar flexion. While the therapist holds the ankle in dorsiflexion, he applied the distal end of the tape 10 cm below the ankle joint. With almost 70% tension, the proximal end is applied 10 cm above the ankle joint (Fig. 3B). While one hand was holding each end of the tape, the child was asked to move the joint into plantar flexion. Finally, both hands moved the joint’s centre to apply the remaining tape (14).

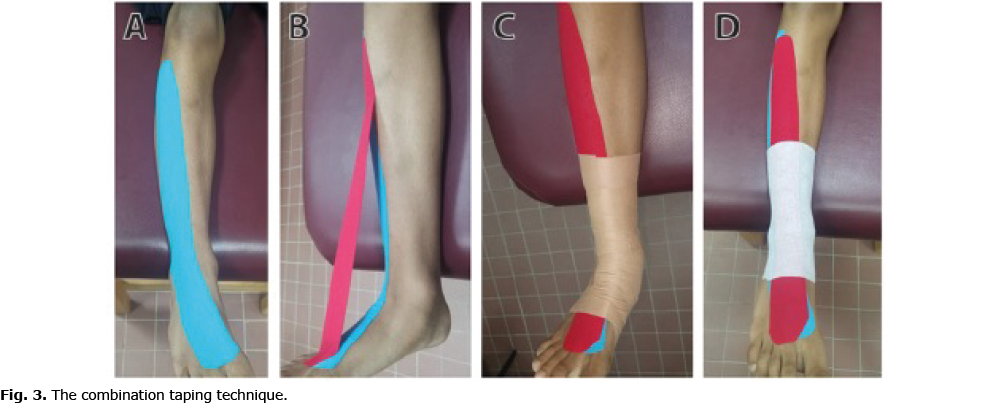
In order to complete the procedure, a 3-cm leukotape tape (Leukotape P Sports Tape, BSN Medical, NC, USA) was applied to the ankle using the conventional closed basket weaving technique (15). This technique used medial-lateral stirrups and heel locks in a figure-of-eight pattern to control hind-foot motion in the frontal plane (Fig. 3C). The ankle was placed in dorsiflexion during the rigid tape application, which was applied over a cover-roll stretch adhesive bandage to prevent skin irritation (Fig. 3D). Combination taping was done on both feet for 28 days, 24 h a day, and it was changed every 4 days (16).
Children in the control group, in addition to those in both experimental groups continued with 1 h, 3 times per week for 4 weeks of conventional physical therapy. Stretching for tight muscles, weak muscles strengthening, postural reactions training, proprioceptive training, and walking training were all part of the treatment plan, which was based on the neurodevelopmental approach.
Measurement
The GAITRite System (CIR Industries, Clifton, NJ, USA) was used to test the temporal and spatial parameters. The GAITRite is 5 m long and 0.9 m wide instrumented carpet. The walkway’s active area is 4 m long and 0.6 m wide with pressure sensors embedded in the horizontal grid into the carpet (each divided by 1.3 cm). When the subject walked across the carpet, the sensors closed under pressure, allowing data on spatiotemporal parameters to be collected. The walkway was linked to a computer, and spatiotemporal parameters were measured and saved with the GAITRite, Version 3.2b software package. This tool has been found to have excellent test-retest reliability (intra-class correlation (ICC)=0.91) (17).
A 5-min adaptation time was given to all participants before the actual measurement. The child then performed 3 walking trials at a self-selected pace with their own footwear for data collection. A trial was considered successful when gait data for 3 full strides at a steady pace on the walkway were obtained. A distance of 1 m was added at both ends of the walkway to allow acceleration and deceleration stages. Measurements were taken in 2 occasions while the children are wearing their own shoes: pre-intervention and after 4 weeks immediately after removal of the tape or AFO. Spatiotemporal parameters were assessed using the GAITRite system in accordance with the published guidelines (18). Parameters included were velocity, cadence, step length; stride length, single and double support times were all assessed.
Statistical analysis
To analyse the collected data, the Statistical Package for Social Sciences (SPSS) for Windows version 20.0 was used (Armonk, NY: IBM Corp.). Analysis of variance (ANOVA) test was used to determine whether there was a significant difference between the 3 groups in terms of age, weight, height, or body mass index (BMI), and the χ2 test was used to determine whether there was a significant difference between groups in terms of sex and hypertonia and GMFCS level. Prior to analysis the collected data, the normality test (Shapiro-Wilk) demonstrated that it was normally distributed (p > 0.05). The differences between step length, stride length, walking velocity, cadence, right single support percent of GC, left single support percent of GC, and double support percent of GC of the 3 groups were tested using the multivariate analysis of variance (MANOVA). A post-hoc test with the Bonferroni corrections were performed for the subsequent multiple comparisons. The significance level (α) of 0.05 was considered statistically significant.
RESULTS
Table I revealed no significant difference in the 3 groups’ age, height, weight, and BMI (p > 0.05). Furthermore, there was no significant difference between groups in terms of sex, hypertonia and GMFCS level (p > 0.05).
The pre-intervention values of the gait velocity, cadence, step length, stride length, right single support, left single support, and double support of the 3 groups were not significantly different (p > 0.005). The post-intervention values of the walking velocity, step length, stride length, right single support duration, and left single support duration of the AFO and combination taping groups were significantly higher than pre values. The post-intervention values of the double support duration of the AFO and combination taping groups were significantly lower than pre-intervention values (p = 0.003). There was no significant differences between the pre- and post-intervention values of the cadence of the 3 groups (p = 0.344, 0.193, 0.327, respectively), as shown in Table II.

The post-intervention values of the walking velocity, step length, stride length, right single support duration, and left single support duration of the AFO and combination taping groups were significantly higher than the control group (p = 0.038, 0.031; 0.014, 0.006; 0.026, 0.020; 0.018, 0.020; 0.010, 0.012, respectively), with no significant differences between the post-intervention values of the AFO and combination taping groups (p > 0.05). The post-intervention value of the double support duration of the AFO and combination taping groups were significantly lower than the control group (p = 0.024, 0.026, respectively), without significant differences between the post-intervention values of the AFO and combination taping groups (p > 0.05). Regarding cadence, there were no significant difference post-intervention values of the 3 groups (p > 0.05).
DISCUSSION
This study measured the changes in gait spatio-temporal parameters of children with spastic diplegia after 4 weeks of applying combination tape or rigid AFO. To our knowledge, no single study has yet compared the effects of combination taping vs AFO on spatiotemporal parameters in the CP paediatric population. The results of the study found a significant improvement in measured spatiotemporal gait parameters, but not cadence in both the combination taping and AFO groups.
In the combination taping group, these results could be attributed to the facilitatory effect of Kinesio taping on the tibialis anterior (TA) muscle activation level. The primary mechanism regarding the enhancement of muscle activation is excitation of the muscle primary and secondary nerve endings through the cutaneous fusimotor reflex that increases fibre tension (19). It is reported that afferents cutaneous mechanoreceptors have multisynaptic reflex connections with the motoneurone pools innervating the muscles underneath. When the muscles are active in standing or walking, cutaneous feedback may play a role in modulating motoneurone output and thereby contribute to stabilization of stance and gait (20). A recent meta-analysis conducted by Yam et al. (21) concluded that Kinesio taping can improve lower limb muscle strength in individuals with muscle fatigue and chronic diseases.
Children with bilateral spastic CP walk with equinus gait, which is defined by the ankle in plantarflexion throughout stance phase of gait and the hips and knees extended. This attributed to gastrocnemius and/or soleus spasticity with consequent antagonistic inhibition of TA muscle (22). The limitation of dorsiflexion leads to major changes in joint arthrokinematics, as talus position and gliding restriction (23). Kang et al. (24) have reported these changes to be the major causes of gait deviations; reduced stride length, decreased gait velocity, and risk of falls. Improved stride length and gait velocity in this study indicate increased activity of the TA during stance and swing phases of gait. Facilitation of the TA muscle will lead to a decrease in calf muscle tightness by reciprocal inhibition, which is a spinal process that inhibits a motor neurone pool of agonist when the antagonist is activated (25).
The complementary effect of rigid taping in the combination technique was to limit plantar flexion and holds the ankle joint in the close-packed position for increased stability. Ounpuu et al. (26) clarified that the specific characteristics of spastic CP gait interfere with the normal interaction of foot and ankle on ground and plantar flexion is maintained throughout the stance phase reducing plantar flexion moment and force production to prepare for swing phase. The authors added that solving these problems should be the primary goal of rehabilitation programmes to restore normal gait features of children with spastic CP. The rigid tape helps to correct the position of the foot required for proper initial contact, changing the toe gait of CP into heel-toe gait, allowing normal weight shift within the sole, and improving single-leg support (27). Kim & Park (28) found that when the ankle is dorsiflexed 10°, the movement of the centre of pressure during gait was significantly reduced, and it positively affected the balance ability.
The results of this study are in partial agreement with those of Junga et al. (29) who examined the immediate effects of Kinesio taping on gait parameters in CP children. They found a major improvement in gait velocity, step length, stride length, and single support time of the right leg. There were no major variations in cadence, single support time of the left leg, or double support. The differences in treatment duration and sample size could explain the partial disagreement between the 2 studies. Similarly, Lee & Bae (30) reported significant improvements in gait velocity, cadence, step length, stride length after taping the tibialis anterior and hamstring muscles in 11 patients with chronic stroke. Another study showed that Kinesio taping improved foot kinematics during early stance of gait in patients with chronic ankle instability (31).
In contrast with the results of the current study, Karadag et al. (32) concluded no difference between Kinesio taping and sham taping in improving gait velocity and step length in stroke patients with spastic equinus foot. The high and varying degree of spasticity, ranging from 2 to 4, based on MAS, may be the reason behind the reported results. Moreover, we have several concerns regarding the appropriateness of the amount of tension applied, the direction, frequency, and duration of Kinesio taping. Finally, the tool used for gait analysis was not mentioned clearly.
The improvement in spatiotemporal gait parameters in the AFO group can be explained by the ability of the orthosis to provide better ankle stability during the stance phase (33). AFO facilitates proper foot–ground contact at initial contact and reduces knee flexion at mid-stance by avoiding excessive forward movement of the tibia over the foot during the second rocker. This helps to considerably decrease the elevated knee extensor activation level, which is associated with the characteristic crouch gait of spastic diplegic children (34). In addition, AFO improves foot clearance during the swing phase.
The results of the study in this regards are in agreement with several previous studies (6, 35–37) that showed significant positive effects of wearing AFOs on gait parameters in children with CP with equinus deformities. In contrast, Kerkum et al. (38) concluded that after 4 weeks of rehabilitation using a ventral shell AFO, the spatiotemporal parameters, joint kinematics and kinetics of children with spastic CP did not change significantly. The small sample size is a threat to the external validity in their study and limits the degree of generalization of the results.
The insignificant difference in the results between the combination taping and AFO groups, gives an alternative non-invasive technique for the control of equinus deformity and calf muscle tightness in spastic diplegic children. AFOs had a large negative effect on the propulsive force prior to swing phase (8), impede sensory feedback during gait (33), and lead to weakness of the muscles through holding the ankle joint in a fixed position (39).
The current study has some limitations; first, only immediate effects after 4 weeks from the intervention were studied. Secondly, other types of AFOs, such as hinged, ventral shell, dorsal shell or posterior leaf spring were not included. Finally, kinematic and kinetic gait parameters were not integrated with the spatio-temporal parameters. Future studies are recommended to investigate these limitations.
CONCLUSION
The results of the study showed that combination taping is an effective alternative technique to AFOs to improve spatio-temporal gait parameters on the short term. Improving gait quality is an essential prerequisite for efficient walking in children with spastic CP to be independent in functional activities and take part in society.
The authors have no conflicts of interest to declare
REFERENCES
- Jonsson U, Eek MN, Sunnerhagen KS, Himmelmann K. Cerebral palsy prevalence, subtypes, and associated impairments: a population-based comparison study of adults and children. Dev Med Child Neurol 2019; 61: 1162–1167.
- Reddihough D. Cerebral palsy in childhood. Aust Fam Physician 2011; 40: 192–196.
- Kamp FA, Lennon N, Holmes L, Dallmeijer AJ, Henley J, Miller F. Energy cost of walking in children with spastic cerebral palsy: relationship with age, body composition and mobility capacity. Gait Posture 2014; 40: 209–214.
- Horsch A, Klotz MCM, Platzer H, Seide S, Zeaiter N, Ghandour M. Is the prevalence of equinus foot in cerebral palsy overestimated? Results from a meta-analysis of 4814 feet. J Clin Med 2021; 10: 4128.
- El-meniawy GH. Influence of ankle kinesio taping on ankle excursion and selected gait parameters in children with hemiparesis. Bull Fac Phys Ther 2010; 15: 87–95.
- White H, Jenkins J, Neace WP, Tylkowski C, Walker J. Clinically prescribed orthoses demonstrate an increase in velocity of gait in children with cerebral palsy: a retrospective study. Dev Med Child Neurol 2002; 44: 227–232.
- Scheinberg A. Book review clinical evaluation and management of spasticity. J Paediatr Child Health 2002; 38: 535–536.
- Lintanf M, Bourseul JS, Houx L, Lempereur M, Brochard S, Pons C. Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: a systematic review and meta-analysis. Clin Rehabil 2018; 32: 1175–1188.
- Desjardins-charbonneau A, Jean-sébastien R, Dionne CE, Desmeules F. The efficacy of taping for rotator cuff tendinopathy : a systematic review. Int J Phys Ther 2015; 10: 420–433.
- Reiter F, Danni M, Lagalla G, Ceravolo G, Provinciali L. Low-dose botulinum toxin with ankle taping for the treatment of spastic equinovarus foot after stroke. Arch Phys Med Rehabil 1998; 79: 532–535.
- Güçhan Z, Mutlu A. The effectiveness of taping on children with cerebral palsy: a systematic review. Dev Med Child Neurol 2017; 59: 26–30.
- Unger M, Carstens JP, Fernandes N, Pretorius R, Pronk S, Robinson AC, Scheepers K. The efficacy of kinesiology taping for improving gross motor function in children with cerebral palsy: A systematic review. S Afr J Physiother 2018; 74: 459.
- Kenzo K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Method. 3rd edition. New Mexico: Kinesio Taping Association; 2013.
- Kora A, Abdelazeim F, Olama K, Raouf E, Abdelraouf O. Muscle inhibitory vs functional corrective kinesio taping on gross motor functional abilities in children with spastic cerebral palsy. J Complement Altern Med Res 2018; 6: 1–9.
- Beam JW. Orthopedic Taping, wrapping, bracing, & padding. 3rd edition. Philadelphia: F. A. Davis Company; 2017
- Tabatabaee M, Shamsoddin MC and A. The effects of Kinesio taping of lower limbs on functional mobility, spasticity, and range of motion of children with spastic cerebral palsy. Egypt J Neurol Psychiatry Neurosurg 2019; 55: 2–6.
- Van Uden CJT, Besser MP. Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite). BMC Musculoskelet Disord 2004; 5: 1–4.
- Kressig RW, Beauchet O, Gaitrite E, Group N. Guidelines for clinical applications of spatio-temporal. Aging Clin Exp Res 2005; 18: 174–176.
- Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil 2010; 91: 1383–1389.
- Aniss AM, Gandevia SC, Burke D. Reflex responses in active muscles elicited by stimulation of low- threshold afferents from the human foot. J Neurophysiol 1992; 67: 1375–1384.
- Yam ML, Yang Z, Zee BCY, Chong KC. Effects of Kinesio tape on lower limb muscle strength, hop test, and vertical jump performances: a meta-analysis. BMC Musculoskelet Disord 2019; 20: 1–12.
- Armand S, Decoulon G, Bonnefoy-Mazure A. Gait analysis in children with cerebral palsy. EFORT Open Rev 2016; 1: 448–460.
- Koh E-K, Weon J-H, Jung D-Y. Effect of direction of gliding in tibiofibular joint on angle of active ankle dorsiflexion. J Korean Soc Phys Med 2014; 9: 439–445.
- Kang D, Kim Y, Lee K. Comparisons of lower extremity strength, cognition, and ankle mobility according to the 8.5 seconds cut-off point for the 8-foot up-and-go test in elderly women. J Korean Soc Phys Med 2015; 10: 87–93.
- Osama M, Shakil Ur Rehman S. Effects of static stretching as compared to autogenic inhibition and reciprocal inhibition muscle energy techniques in the management of mechanical neck pain: a randomized controlled trial. J Pak Med Assoc 2020; 70: 786–790.
- Ounpuu S, Gage JR, Davis RB. Three-dimensional lower extremity joint kinetics in normal pediatric gait. J Pediatr Orthop 1991; 11: 341–349.
- Son IH, Lee DG, Hong SK, Lee K, Lee GC. Comparison of gait ability of a child with cerebral palsy according to the difference of dorsiflexion angle of hinged ankle-foot orthosis: a case report. Am J Case Rep 2019; 20: 1454–1459.
- Kim C-S, Park S-Y. Effects of an ankle foot orthosis with ankle angles on balance performance in healthy adults. J Ergon Soc Korea 2011; 30: 291–296.
- SH Junga, SH Song, DR Kim, SG Kim, YJ Park, YJ Son GL. Effects of kinesio taping on the gait parameters of children with cerebral palsy: a pilot study. Phys Ther Rehabil Sci 2016; 5: 205–209.
- Lee D, Bae Y. Short-term effect of kinesio taping of lower-leg proprioceptive neuromuscular facilitation pattern on gait parameter and dynamic balance in chronic stroke with foot drop. Healthcare 2021; 9: 271.
- Deschamps K, Dingenen B, Pans F, Van Bavel I, Matricali GA, Staes F. Effect of taping on foot kinematics in persons with chronic ankle instability. J Sci Med Sport 2016; 19: 541–546.
- Karadag-Saygi E, Cubukcu-Aydoseli K, Kablan N, Ofluoglu D. The role of kinesiotaping combined with botulinum toxin to reduce plantar flexors spasticity after stroke. Top Stroke Rehabil 2010; 17: 318–322.
- Mf A, Ga J, Cl V, Abel MF, Juhl GA, Vaughan CL, et al. Gait assessment of fixed ankle-foot with spastic diplegia orthoses in children. Arch Phys Med Rehabil 1998; 79: 126–133.
- Rogozinski BM, Davids JR, Davis RB, Jameson GG, Blackhurst DW. The efficacy of the floor-reaction ankle-foot orthosis in children with cerebral palsy. J Bone Jt Surg - Ser A 2009; 91: 2440–2447.
- Hayek S, Hemo Y, Chamis S, Bat R, Segev E, Wientroub S, et al. The effect of community-prescribed ankle-foot orthoses on gait parameters in children with spastic cerebral palsy. J Child Orthop 2007; 1: 325–332.
- Buckon CE, Thomas SS, Jakobson-Huston S, Moor M, Sussman M, Aiona M. Comparison of three ankle-foot orthosis configurations for children with spastic diplegia. Dev Med Child Neurol 2007; 46: 590–598.
- Brehm M, Harlaar J, Schwartz M. Original report effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J Rehabil Med 2008; 40: 529–534.
- Kerkum YL, Brehm MA, Van Hutten K, Van Den Noort JC, Harlaar J, Becher JG, et al. Acclimatization of the gait pattern to wearing an ankle-foot orthosis in children with spastic cerebral palsy. Clin Biomech 2015; 30: 617–622.
- Bulley C, Shiels J, Wilkie K, Salisbury L. User experiences, preferences and choices relating to functional electrical stimulation and ankle foot orthoses for foot-drop after stroke. Physiotherapy 2011; 97: 226–233.